One of the most frequently diagnosed pathologies associated with respiratory dysfunction is compacted roots of the lungs. As a rule, when going for a chest x-ray, people do not even suspect that they have this problem. Despite the fact that it does not pose a serious threat to health and life, timely treatment is nevertheless necessary to avoid various complications.
If nothing is done, the patient may develop bronchitis, pneumonia and many other serious diseases. No one is immune from such unwanted ailments. During the examination, the doctor may announce unpleasant news when the root of the lung is compacted. Let’s talk in more detail about what this means for the patient. We will also provide information about the types of disease.
Lung root: what is it?
The root of the lung is a complex of structures located at the hilum of the lung. These include the pulmonary artery, vein, main bronchus, as well as nerves, lymphatic vessels, pleura, and fatty tissue. All these structures are located in a strictly defined order, but some of them on the left side are not visible on the x-ray, hiding behind the shadow of the heart.
In plain radiography and fluorography, the term “root of the lung” refers only to large vessels (artery, vein) and bronchus.
Main characteristics of the roots of the lungs
To determine a symptom such as compaction of the roots of the lungs on an x-ray, you first need to know the normal characteristics of these formations.
The root of both the right and left lungs consists of three parts: the head, the body and the tail. The tail includes terminal small branching vessels.
In radiology, the width of these structures is also determined. It is usually determined by the width of the right root and includes the arteries and intermediate bronchus. Normally its width is 1.5-2 cm.
It is also worth noting that the arteries in the roots of the lung are located more vertically, and the veins - horizontally. Sometimes their structure may be heterogeneous due to the fact that in some areas clearing of air in the bronchi is visible.
Digital code for describing the results of fluorography assessment
How often can I undergo fluorography? Find out by watching the Video.
02 — Darkening in the lung tissue (infiltration, atelectasis, rounded shadow, mid-lobe syndrome, etc.).
03 - Focal shadows in the lung tissue.
04 — Expansion of the mediastinal shadow, including an increase in the size of the root.
06 — Fibrous changes in the lung tissue (pronounced).
07 — Fibrous changes in the lung tissue (limited).
08 — Increased transparency of lung tissue (local and widespread emphysema).
09 — Changes in the pleura (adhesions, pleural layers, calcifications) are pronounced.
10 — Changes in the pleura (adhesions, pleural layers, calcifications) are limited.
11 — Petrifications are large in the lung tissue—multiple (5 or more).
12 — Petrificates are large in the roots—multiple (5 or more).
13 — Petrifications are small in the lung tissue—multiple (5 or more).
14 — Petrifications are small in the roots — multiple (5 or more).
15 — Large petrifications in the lung tissue are rare.
16 — Large petrificates in the roots are rare.
17 — Petrifications are small in the lung tissue—single.
18 — Petrificates are small in the roots—single.
19 — Changes in the diaphragm not associated with pleural pathology (diaphragmatic hernia, high diaphragm, etc.).
20 — Condition after lung surgery.
21 — Changes in the chest skeleton (scoliosis, kyphoscoliosis, callus, additional rib, osteophytes, etc.).
22 — Foreign body (projected onto the pulmonary tissue, mediastinal shadow in the soft tissues).
When several of the listed changes are combined, each of them is marked with a corresponding code in each graph cell. Localization and extent of changes are marked with a fraction on the second graph cell 1; 2; 3; 4; in the numerator - the right lung, in the denominator - the left lung (in the fields).
Lung field code number:
4 - first and second,
5 - first and third,
6 - second and third,
7 - first, second and third.
In the third graph cell, instead of the doctor’s signature, the personal number of the radiologist is substituted. A call for a follow-up x-ray examination is marked in the fourth graph cell with the number 1.
"Nurse's Directory" 2004, "Eksmo"
Differences in the structure of the roots of the lungs
It is necessary to understand that the left root is poorly visible on the x-ray, as it is covered by the heart, so sometimes it is difficult to see when the root of the left lung is compacted.
It should also be remembered that the root of the left lung normally has a heterogeneous structure, since it consists of almost only vessels, branching into small branches and intertwining with the left bronchus. While the right root has a more uniform structure.
Main causes of root compaction
There are many different diseases and syndromes that cause the roots of the lung to become denser. The main reasons include:
- Chronic obstructive pulmonary diseases (chronic obstructive bronchitis).
- Enlargement of the mediastinal lymph nodes (paratracheal, parabronchial) with the development of petrification (deposits of calcium salts) in them.
- Dilatation and protrusion of the vessel wall or aneurysm of the vessel.
- Changes in the structure of the bronchus under the influence of the tumor process.
- Pulmonary edema (fluid penetration into the lung parenchyma).
- An increase in connective tissue with the development of fibrosis, which occurs after prolonged inflammatory pulmonary diseases, lung injuries, and surgical interventions on the organs of the chest cavity.
- Tuberculosis of the bronchi (tuberculous bronchoadenitis), tuberculosis of the intrathoracic lymph nodes, primary tuberculosis complex. The last two forms belong to primary tuberculosis, most common in preschool children.
- Occupational diseases (asbestosis, metalloconiosis).
Chronic obstructive pulmonary diseases
This group of diseases is one of the most common reasons why the roots of the lungs are compacted and expanded. As a rule, this process is two-way, affecting both the left and right roots. Most often, the disease develops in long-term smokers and is characterized by alternating periods of exacerbation with periods of remission.
The main clinical manifestations are cough, which is especially disturbing to the patient in the morning - with viscous, sometimes purulent sputum. With a prolonged course of the disease, shortness of breath develops, which is first noted during physical exertion, and then at rest.
In addition to conducting a survey X-ray of the chest cavity, which is characterized by the fact that the roots in the lungs are compacted and stringy, sputum culture is also performed to determine the causative agent of the disease (viral or bacterial).
Etiotropic therapy, that is, treatment of the cause, depends on the pathogen that caused the exacerbation. If the cause is a bacteria, then taking antibiotics will be effective; if it is a virus, taking antiviral drugs will be effective.
Symptomatic therapy includes taking mucolytics, drugs that dilute sputum, and expectorants to make it easier to clear. They also take drugs that dilate the bronchi - adrenergic receptor agonists, corticosteroids.
Conditions for the development of the disease
The condition when the heart is enlarged in diameter is most often diagnosed in adults. Factors that increase the boundaries of the shadow of the atria and ventricles are varied and are often associated with pathology of the heart and blood vessels.
Common reasons include:
- high physical activity;
- pregnancy;
- Chagas syndrome;
- genetic predisposition;
- high pressure in the aorta and blood vessels;
- severe form of vascular anemia;
- various heart diseases;
- kidney dysfunction;
- ischemia, heart attack;
- the heart is enlarged to the left due to lung diseases.
Of course, there are factors that may not always lead to expansion. For example, viral infections, parasitic diseases, immune system diseases, and more.
Signs of growth of the organ shadow within the ventricles and atria are similar to other diseases of the cardiovascular system.
The following symptoms are observed:
- chest pain;
- dyspnea;
- swelling of the legs and arms;
- high fatigue;
- fainting;
- pale skin.
You can find out that the heart has expanded its boundaries during examination using ultrasound, radiography, echocardiography or MRI. For example, Figure No. 1 is presented in the form of a fluorography image. The shadow marked in the image indicates the expansion of the organ's shadow.
Figure No. 2 allows you to visually compare the normal state of the atria and ventricles, and the moment when the organ expanded its boundaries.
The course of treatment with medications depends on the severity of the disease:
- Diuretic medications reduce pressure in blood vessels.
- To avoid the risk of blood clots in the vessels, anticoagulants are prescribed.
- To restore the functioning of the cardiac system, angiotensin prescription blockers are prescribed. The drugs Warfarin and Heparin are effective in treating atrial and ventricular dysfunction.
- Medications of the beta blocker group are designed to normalize the pulse.
The expansion of the organ's shadow leads to various consequences - blood clots, cardiac arrest, rhythm disturbances, and death.
The greatest danger is the enlargement of the boundaries of the ventricle of the left chamber. This pathology most often leads to death.
If conservative treatment methods have no effect and the patient’s condition worsens, then doctors advise surgery. The type of intervention is considered on an individual basis. For example, they may prescribe inserting a defibrillator under the skin to adjust the rhythm.
Oncological diseases
A dangerous, but, fortunately, infrequent reason that the roots of the lungs are compacted and expanded is the oncological process in the bronchi and mediastinal organs. This process is usually one-sided, so changes in the root of the lung are observed only on one side.
Oncology implies a long-term chronic process with a gradual deterioration of the patient’s condition. A slight cough and heavy breathing are replaced by pain behind the sternum at the site of the tumor projection onto the chest wall (with compression of the nerves), hemoptysis, and severe shortness of breath. In addition to dysfunction of the pulmonary system, the entire body suffers. The patient loses weight, becomes exhausted, and fatigue and weakness appear.
After conducting a survey X-ray of the chest cavity in two projections, the radiologist makes a conclusion: “The roots of the lungs are compacted and have little structure.” Next, the attending physician issues a referral for a biopsy of the formation suspicious on the x-ray, which will determine not only the type of tumor (benign or malignant), but also its histological structure (from what tissue it was formed).
Therapy depends on both the stage of the tumor process and its type. Main therapeutic methods: surgery, radiation and chemotherapy. Surgery alone is used in the initial stages of tumor development; in later stages it is combined with other methods of therapy.
Occupational diseases
People in professions such as miners, metal welders, builders, that is, those who constantly interact with harmful environmental substances, are most susceptible to developing occupational diseases. This leads to the fact that on the radiograph the roots in the lungs are fibrously compacted and stringy. This picture develops due to the accumulation of harmful particles in the bronchi and alveoli, which settle on the respiratory tract. As a rule, root damage is not isolated, but is combined with the presence of focal shadows and heterogeneity of the lung parenchyma.
The symptoms of these diseases are not specific; When making a diagnosis, first of all, pay attention to the professional history (place of work, length of service). And the main method of treatment is changing qualifications and changing jobs.
How to decipher the results of fluorography?
02 - Darkening in the lung tissue (infiltration, atelectasis, rounded shadow, mid-lobe syndrome, etc.).
03 - Focal shadows in the lung tissue.
04 - Expansion of the mediastinal shadow, including an increase in the size of the root.
05 - Pleural effusions.
06 - Fibrous changes in the lung tissue (pronounced).
07 - Fibrous changes in lung tissue (limited).
08 — Increased transparency of the lung tissue (emphysema, local and widespread).
09 - Changes in the pleura (adhesions, pleural layers, calcifications) are pronounced.
10 - Changes in the pleura (adhesions, pleural layers, calcifications) are limited.
11 - Petrificates are large in the lung tissue - multiple (5 or more).
12 - Large petrificates in the roots - multiple (5 or more).
13 - Petrificates are small in the lung tissue - multiple (5 or more).
14 - Petrificates are small in the roots - multiple (5 or more).
15 - Large petrificates in the lung tissue - single.
16 - Large petrificates in the roots - single.
17 - Petrificates are small in the lung tissue - single.
18 - Petrificates are small in the roots - single.
19 - Changes in the diaphragm not associated with pleural pathology (diaphragmatic hernia, high position of the diaphragm, etc.).
20 — Condition after lung surgery.
21 - Changes in the chest skeleton (scoliosis, kyphoscoliosis, callus, additional rib, osteophytes, etc.).
22 - Foreign body (projected onto the lung tissue, mediastinal shadow in the soft tissues).
Root damage due to tuberculosis
A situation where the roots of the lungs are compacted usually occurs in children with primary pulmonary tuberculosis. These are forms such as primary tuberculosis complex and tuberculosis of the intrathoracic lymph nodes. However, these forms can also occur in older people during reinfection of an old lesion.
Tuberculosis is a chronic disease, so symptoms develop over a long period of time and gradually. Characteristic symptoms include a dry cough or with a small amount of sputum, possibly mixed with blood, chest pain, fatigue, lethargy, and weight loss.
After performing radiography in two projections, sputum culture and microscopy are performed to identify Mycobacterium tuberculosis, and a tomogram of the lungs is performed to more accurately localize the source of infection. After sowing the tuberculosis bacillus, its sensitivity to anti-tuberculosis drugs is determined, which is necessary to select the most effective treatment.
Drug therapy is based on the principles of continuity and long-term duration (minimum 6 months). It is also necessary to use a combination of at least 4 anti-TB drugs. Only if these principles are followed will the treatment be effective.
Treatment of pulmonary fibrosis
There are no specific treatments for this disease, which usually has a progressive course. Several experimental treatments for pulmonary fibrosis are currently being studied in some experimental clinical trials.
In younger patients, the most effective therapeutic option is lung transplantation.
However, there are a number of treatment methods aimed at slowing the progression of the disease and improving the patient’s quality of life (oxygen therapy, cortisone and immunosuppressants, pulmonary rehabilitation programs):
- Cortisone : an anti-inflammatory drug that suppresses the immune system's response. With long-term use, cortisone can also cause severe side effects (this drug exposes the patient to the risk of infections, can cause metasteroid diabetes, weight gain, osteoporosis, peptic ulcers, mental changes);
- Cyclophosphamide , Azathioprine : These drugs suppress the immune system's response;
- N-acetylcysteine : This is a mucolytic, expectorant, and antioxidant that also helps sick patients with pulmonary fibrosis;
- Oxygen therapy : serves to replenish the lack of oxygen caused by decreased lung function. The requirement is established based on blood gas analysis and oximetry. It can be administered only at night, during physical activity, or throughout a 24-hour period;
- Respiratory rehabilitation programs : its task is to teach the patient to breathe better and tolerate stress;
- Lung transplantation : This is the definitive therapy for pulmonary fibrosis. It is intended in selected cases, for patients without other concomitant diseases. Lung transplantation is a very complex procedure and is performed only in highly specialized centers.
All patients with pulmonary fibrosis should combine therapy with a healthy lifestyle, which includes:
- regular physical activity (perhaps as part of a respiratory rehabilitation program), without fear of shortness of breath. The more sedentary you are, the worse your muscle condition becomes; physical activity, on the other hand, allows you to better cope with stress and improves quality of life and mood;
- A healthy diet based on a diet rich in fruits, vegetables and whole grains, lean meats, poultry, fish, milk and low-fat dairy products. Instead, you should limit your intake of salt, sugar, animal fats and sweets. Those suffering from respiratory failure should avoid large meals and divide meals into smaller portions;
- you need to quit smoking and avoid exposure to secondhand smoke;
- get enough sleep and master relaxation techniques;
- It is necessary to get vaccinated against pneumococcal infection and regularly get it against influenza.
The roots of the lungs are heavy and compacted: what does this mean?
As noted above, this radiological syndrome most often occurs in smoker’s chronic bronchitis and occupational lung diseases. However, this symptom can also be detected in acute inflammatory diseases of the respiratory tract and cancer.
These strands are connective tissue fibers that stretch from the root to the periphery. Heaviness is usually combined with expansion and compaction of the root.
Although not highly specific, this syndrome allows the doctor to suspect a certain pulmonary pathology and refer the patient for further examination.
Symptoms of pulmonary fibrosis
Pulmonary fibrosis tends to present with the following symptoms:
- shortness of breath, wheezing (shortness of breath occurs at the beginning due to physical exertion, then it begins to appear more and more when a person gets dressed, walks around the house or talks);
- chronic “dry” cough that does not produce sputum;
- weakness, asthenia;
- chest discomfort;
- loss of appetite and weight.
Less commonly, the following symptoms may also be present:
- fever;
- pain in muscles and joints;
- hemoptysis (the release of blood from the respiratory tract, usually through coughing).
The roots of the lungs have little structure and are compacted: what does this mean?
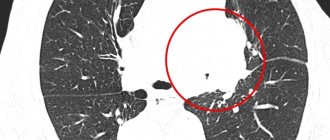
Violation of the structure of the lung root, that is, the inability to distinguish a vessel from a bronchus, the appearance of darkening on the root, usually occurs in primary tuberculosis and oncological processes.
On an x-ray with extensive tuberculosis or central lung cancer, instead of a root, a shadow of various contours may be visualized, representing a focus (up to 10 mm in diameter) or an infiltrate (more than 10 mm). This symptom may also be combined with compaction, which usually occurs with the deposition of calcium salts or calcification (petrification). Calcification is a sign of a chronic, long-lasting process.
Thus, just one radiological symptom (in the lungs the roots are fibrously compacted and tractable) can help to suspect many diseases: from ordinary bronchitis to lung cancer. Of course, we should not forget that radiography should be supplemented by other examination methods: computed tomography, biopsy, sputum culture, bronchoscopy, and so on. Additional examination methods are performed as prescribed by the doctor, depending on the path of his diagnostic search. It must be remembered that only a comprehensive examination will help make the correct diagnosis.