Tomographic studies are by far the most effective among non-invasive research methods. They are especially widely used for diagnosing cancer.
The term “tomography” is of Greek origin: “tomos” means “layer”, “grapho” means to write. Tomography in medicine is any diagnostic method that allows you to obtain layer-by-layer images of the structure of the human body.
- Computed tomography in the diagnosis of lung cancer
- Magnetic resonance imaging
- Signs of lung cancer on CT and MRI
Can CT scans make mistakes in diagnosis?
Like any other diagnostic method that is based on the analysis of indirect data, computed tomography produces results that have some probability of error. And although this probability is quite small, it is of great importance in diagnosing cancer. The most common causes of diagnostic errors are:
- Incorrect interpretation of received images;
- Low quality equipment, resulting in low-quality images.
The quality of the images also depends on the serviceability and correct settings of the tomograph, the patient’s behavior during manipulation, as well as some other external factors. Such reasons can lead to the appearance of additional interference in the image, which makes it difficult to decipher or is completely wrongly interpreted as a formation or metastasis.
The reliability of interpretation of tomographic images when diagnosing cancer directly depends on the experience of the radiologist and oncologist. This is especially important in complicated diagnostic cases, for example, the following diseases can be interpreted differently:
- Tuberculous infiltrate and peripheral lung cancer on CT;
- Retrocerebellar cyst and dilatation of the cisterna magna;
- Thrombosis and Pachionian granulations;
- Brain tumor and ischemic or hemorrhagic stroke;
- Epidural or subdural hematoma and subarachnoid hemorrhage;
- Malignant formation and aneurysm of a cerebral vessel.
Medical errors can also occur in the description of the size of the tumor, lymph nodes, and other important characteristic features.
The Yusupov Hospital employs the best highly specialized specialists, thanks to whom the percentage of human errors is reduced to zero. The doctors at the oncology clinic have extensive experience working with all manifestations of malignant processes. Hospital doctors carefully study all diagnostic data and also communicate in detail with patients so that the correct diagnosis is made as soon as possible.
Symptoms and signs of the disease
The most common symptoms of the disease are:
- cough that doesn't go away or gets worse;
- coughing up blood or rust-colored phlegm;
- chest pain that gets worse with deep breathing, coughing, or laughing;
- hoarseness;
- weight loss and appetite;
- breathing problems;
- feeling tired or weak;
- frequent or prolonged bronchitis and pneumonia.
Some respiratory cancers can cause syndromes, which are groups of specific symptoms.
What does lung cancer look like on a CT scan?
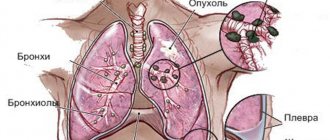
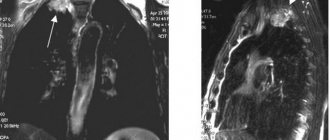
CT is the main method of visualizing the disease, on the basis of which further treatment is determined. The study also uses MSCT (multilayer computed tomography). The primary tumor produces a wide range of images. Non-small cell cancer can be centrally located, invading mediastinal structures, or peripherally, extending into the chest wall.
The edges of the tumor may be smooth, divided into lobes, or uneven and needle-like. The neoplasm can be uniform and dense or have necrosis and cavitation. Centrally located and cavitating tumors are more likely to have flat histology. Sometimes the tumor resembles an infectious pathology and is considered an area of compaction or is light-opaque. This type is more common in adenocarcinoma and its subtypes.
When the disease is discovered incidentally in a symptomatic patient, the tumor is often visualized as a solitary pulmonary nodule, which may have a variety of imaging appearances. The most accurate picture is obtained using PET CT for lung cancer.
What do cancer cells look like on a CT scan?
In the image obtained on a computed tomograph, tumors and metastases usually appear as formations of reduced density. But sometimes identifying cancer cells in images can be difficult for a number of reasons:
- Closely located hemorrhages;
- Accumulations of tissues of certain organs nearby;
- Calcification of metastases.
In such difficult situations, for a clearer image before the procedure, the patient is injected with contrast - a special substance that details the picture of the disease. At the same time, on computed tomography images, the formations show an increase in contrast, since their X-ray density decreases.
MSCT in oncology
One of the most functional diagnostic devices are multislice computed tomographs, which make it possible to detect tumors at their inception stages. The difference between such CTs and spiral ones is the presence of a large number (several tens or hundreds) of rows of detector elements. This solution ensured a proportional reduction in the duration of formation and an increase in the resolution of volumetric scanning images.
MSCT in oncology is a new level of effectiveness in medical research, achieved by improving the quality of constructing multiplanar and volumetric models of the examined areas. If the development of tumors is suspected, diagnostics using MSCT is mandatory, since it makes it possible to identify pathological changes at the earliest stages of development. And the likelihood of successful treatment of cancer directly depends on the efficiency and reliability of diagnostic measures.
How is a CT scan performed?
Before starting the study, the patient must provide the doctor with all the necessary data about his condition, as well as information about previous diagnostic methods.
Pregnant women are not recommended to have a CT scan due to possible risks to the baby. Tomography is performed only in emergency, life-threatening conditions.
Children under 5 years of age are usually given sedatives or anesthesia, which is directly performed by an anesthesiologist.
A computed tomography scan takes about 30 minutes, in rare cases – up to one hour.
You must remove all metal items and wear loose clothing.
Preparation for the examination depends on the area and the contrast agent used. In the latter case, it is necessary to refrain from eating food for 4 hours before the procedure, and, on the contrary, you need to drink as much as possible in order to quickly remove the contrast from the body.
If a CT scan is performed under anesthesia, it is prohibited to consume food and water for 4 hours.
The patient must lie still throughout the entire time to ensure reliable images.
The Yusupov Hospital provides patients with many services, including a complete diagnosis of cancer patients using a modern computed tomography scanner. The oncology clinic employs the best doctors who constantly confirm their qualifications and use European methods of diagnosis and treatment. The hospital has many awards and a huge number of grateful patients. Yusupov Hospital is one of the best medical institutions in the Russian Federation. The Yusupov Hospital operates around the clock, seven days a week, and therefore can receive you at any convenient time.
Author
Dmitry Yuryevich Frantsev
Doctor for X-ray endovascular diagnostics and treatment, Ph.D.
Lung cancer screening
Everyone in a row? No, not at all necessary. At the first stage, it is necessary to identify a risk group for pulmonary oncology, and it is these people who should undergo low-dose spiral CT at least once a year.
At-risk groups:
- Long-term smokers (20 years or more) aged 50 years and older;
- Recently quit smoking (less than 15 years since the last cigarette smoked);
- The presence of occupational hazards in the form of regular inhalation of any chemicals, heavy metals, dust or radon at work;
- Heredity for bronchopulmonary cancer (presence of relatives with lung cancer in the family);
- Severe form of chronic obstructive pulmonary disease.
Where the risk is high, computed tomography should be performed in a special low-dose mode (and the radiation exposure is low, and the effectiveness of early diagnosis of oncology is high).
Errors due to improper preparation and patient behavior
The appearance of artifacts in images may also be associated with the patient’s motor activity during scanning. Please remember that you are prohibited from moving during the entire examination. If necessary (for diagnosing small children, patients with claustrophobia, neurological diseases, severe pain, etc.), sedatives are used.
Distortions can also be caused by foreign objects in the body of the subject, too much weight of the patient, as well as improper preparation. For example, CT of internal organs is performed on an empty stomach, since active peristalsis creates artifacts in the images. You should also eliminate gases from the intestines as much as possible, for which a special diet is prescribed a few days before the procedure.
Contraindications
When performing CT OGK, there are relative contraindications, i.e. in a life-threatening situation, it can be performed in almost any patient.
The severity of contraindications is determined by the doctor. In some cases, it is advisable to cancel or reschedule the study.
Main contraindications for computed tomography of the lungs:
- pregnancy: X-ray radiation has a damaging effect on the fetus;
- severe obesity: permissible body weight depends on the resolution of the tomograph (usually no more than 120-160 kg);
- allergic reactions to iodine-containing drugs (when performing contrast-enhanced CT);
- young age of the patient: the appointment of a CT scan of the lungs for a child should be strictly individual due to the high susceptibility of growing tissues to ionizing radiation;
- inadequate mental state of the patient: inability to remain in a stationary position.
CT scan with contrast may be contraindicated in cases of severe renal or liver failure, decompensated diabetes mellitus, severe pathology of the thyroid gland, or breastfeeding.
Lung scanning modes for oncology
There are two main modes of computed tomography of the chest:
- Mediastinal – used to study the organs of the mediastinum (heart, aorta, interlobar fissures, intersegmental septa, pulmonary vessels, bronchi);
- Pulmonary – allows you to clearly visualize the intersegmental septa, interlobar fissures, and bronchial tree.
Tumor damage can be characterized not only by the formation of a central or peripheral focus of the pulmonary parenchyma. Intrabronchial cancers close the lumen and disrupt the passage of air through the bronchi. X-rays of the chest organs show hypoventilation or atelectasis of the pulmonary segment with endobronchial growth. The pulmonary CT mode of the lungs allows you to diagnose bronchial obstruction and determine associated changes. The technology is used to detect peripheral cancer. To verify the central neoplasm, both modes are used – mediastinal and pulmonary.
PET/CT is the most accurate method for diagnosing cancer
Meet Lilita Rosnere, radiologist/therapist at the RUS Nuclear Medicine Clinic and the Oncology Center of Latvia
Is it true that PET/CT is a unique method - the most accurate for diagnosing cancer? I read about a US study in which 24,000 patients were diagnosed with cancer using classical methods - ultrasound, CT scan, biopsy - and immediately afterwards they were examined using positron emission tomography (PET/CT), which resulted in to radical changes in treatment in about 36% of patients.
This remarkable figure effectively implies that without the PET/CT examination, nearly 9,000 patients would have received inappropriate treatment. I have been working in the field of oncology for 15 years, and as an attending physician, I often needed PET/CT examination, but for many years it was not available to us. We felt miserable. The method was available in neighboring countries - for a long time in Tallinn, in two state clinics in Lithuania, in Russia and throughout Europe, and Latvia was the only one without PET/CT! I felt sorry for my patients, because there are many patients with cancer diagnoses. Therefore, I am very glad that we have the opportunity to offer PET/CT examination here in Latvia.
What are the benefits of PET/CT examination?
The main difference is that PET/CT is a combination tool that allows you to simultaneously perform two different examinations - computed tomography (CT) and positron emission tomography (PET), which provides three informative scan images. The first is a CT image that reflects the anatomical structure of the human body. It allows you to look at organs, measure them and determine the size of formations. The second is a PET image. Functional imaging that accurately depicts any malignant cells, their behavior, as well as physiological processes. These two images are combined in digital form - the anatomical image is merged with the functional image and the third is the so-called hybrid image, which is of the greatest importance and contains comprehensive information about the tumor.
When the patient already knows that he has cancer - he has already undergone an ultrasound or computed tomography and the cancer has been diagnosed using a biopsy, a PET / CT examination is an important step in order to determine whether the disease has spread throughout the body, as well as to determine its stage. PET/CT is a full-body examination that allows the treating physician to make strategic decisions about subsequent necessary treatment much more quickly.
When you talk about the spread of a disease, do you mean metastases?
Not only. For example, PET/CT is also often used by hematologists who deal with malignant diseases of the blood and hematopoietic organs - lymphoma and leukemia, since these tumors are primarily systemic disorders, and not one focal disease such as breast cancer. If specialists know which lymphatic tissues contain cancer cells, it is much easier to choose the most appropriate treatment method.
Why do cancer cells glow during examination?
Before starting a PET examination, the patient is given a special radiodrug by intravenous injection, which is evenly distributed throughout the body and sends a signal to the diagnostic device. In order to accurately detect and transmit information about cancer cells, the radiotherapy drug is mixed with glucose, which accumulates in the cells that consume sugar most efficiently. Based on the examination results, we see the consumption of glucose by human tissues - muscles and internal organs, which is reflected by a certain glow. Malignant tumors especially stand out - they are constantly growing, using sugar for energy, so during the examination they consume glucose more intensively. During PET/CT, we can see tumors as glowing spots against the general background. In this way, malignant tumors reveal their location, size and other important information.
Can treatment change significantly if the exact spread of the disease is unknown?
Certainly! For example, a woman has been diagnosed with breast cancer. If the surgeon or attending physician knows this, the cancer can be removed. But if a specialist learns that a woman not only has primary cancer, but the disease has already spread to the bones, lymph nodes and other organs, then instead of surgery, a completely different therapy would be required.
Another important aspect of PET/CT is determining the effectiveness of treatment. For example, at the very beginning of treatment, six to nine cycles of chemotherapy are prescribed. PET/CT examinations are used in the middle of therapy, for example, after three cycles of chemotherapy, and if we see that there is no functionally active tumor tissue in the patient’s body, i.e. nothing glowed during the test, which means the tumor was stopped! Conclusion!? The remaining cycles of chemotherapy are no longer required. This way, the patient's body is not poisoned by chemicals in the first place. And secondly, it saves resources, since chemotherapy is quite expensive. The method allows you to detect incorrect treatment of a certain form of cancer and change the drugs used in time.
The third case when the use of PET/CT is appropriate and valuable is at the end of treatment for an oncological patient. The patient has undergone surgery, chemotherapy, radiation therapy and in a year or less a PET/CT scan will be the best way to make sure that everything is fine and the tumor has not returned.
I would like to emphasize that PET/CT definitely does not replace other examinations. For example, ultrasound and mammography of the mammary glands or ultrasound of gynecological organs, X-ray of the lungs, etc. Various examinations complement each other.
What to do if the cancer does not glow?
Before the procedure, all patients are checked to see if the type of cancer can be tested with this method. We will not examine a patient if we know that PET/CT is not appropriate in a particular case. Taking into account the metabolic processes in the human body, various radiopharmaceuticals have been developed that allow access to certain types of cancer. For example, a malignant prostate tumor does not consume glucose at all, so in the case of prostate cancer, the study is carried out using other drugs - choline (18F-choline) or gallium (68Ga-PSMA). 68Ga-PSMA has been recognized worldwide as the most effective drug for the diagnosis of prostate cancer - it is a prostate-specific membrane antigen, a highly sensitive agent that does not attach to any other inflammatory processes other than the androgen receptor in prostate cancer cells. This method allows you to detect prostate cancer, assess the spread of cancer and differentiate between inflammation and tumor processes. Gallium imaging is especially important for cancer recurrence after previous surgery or radiation therapy. It provides accurate and early diagnosis of relapse even at PSA levels below 1.0. Research shows that gallium can detect metastases in lymph nodes smaller than 5 mm. Such research could significantly change the pace of treatment.
A PET/CT scan of the prostate is very important as it immediately shows whether the pelvic lymph nodes are already cancerous and whether the lymph nodes need to be removed during surgery. However, if the surgeon is unaware of such malignancy, he removes only the prostate gland, leaving the lymph nodes intact and the tumor continues to spread. Additionally, the largest lymph node is not always cancerous. Sometimes a small lymph node may contain cancerous cells and remain intact. This is important to know.
What is the size of metastases that can be detected by PET/CT?
According to the literature - starting from 9 millimeters. But in practice we can see smaller ones. The lymph node is 4 millimeters in size, but it glows! We measure the intensity of radiation accumulation, which is an objective parameter, and the result shows that the node consumes glucose intensively. It becomes clear that the node is malignant.
Tell us about your greatest professional satisfaction during these months when you work with new equipment?
Our first patient we examined with PET/CT had lymphoma. He completed treatment and we needed to determine if treatment was complete or if it should continue. We looked it over and it was, as we say, clean. We were very happy to tell him such good news.
On the same day, we examined a young woman who had undergone treatment for a hematological tumor. She had various complications due to the therapy and she bravely dealt with them, but the CT scan still showed suspicious lesions in her abdomen. Her lymph nodes were enlarged and shrank during therapy but did not disappear. After conducting a PET/CT study, we found that the focal points are metabolically inactive. Thus, only tumor tissue remained, but the disease was no longer viable. We were pleased to share the good news with this patient.
But there is another side - we are the ones who announce news that is worse than what the patient hoped for and the doctor expected. The attending physician knows about one lesion, but we find three or four more, or even more. Unfortunately... So there is good news and bad news, but they are all valuable because the information obtained during the examination is a fact that the treating physician can work with, for example, change the method of treatment.
Are there situations when PET/CT is not required? A person wants and can afford it, but there is no need.
There are people who suffer from cancerophobia or simply have an exaggerated concern about their health, and they are willing to invest money and undergo examinations, although they do not have any prerequisites for a PET/CT scan. We usually convince such people that there is no need for examination and suggest that they see a doctor. PET/CT testing requires a specific purpose—the referring physician is asking specific questions of the diagnostic radiologist to make decisions about the patient's future treatment, such as the choice of therapy, or whether the patient is interested in the spread or recurrence of the disease.
How to apply for PET/CT?
PET/CT examinations at the Diagnostic Center of the Nuclear Medicine Clinic are carried out on the basis of a referral provided - this can be issued by a general practitioner, oncologist, surgical oncologist, hematologist, urologist or other specialist who believes that the patient needs a PET/CT examination (indications for examination PET/CT). You can also schedule a visit to an oncologist at the Nuclear Medicine Clinic, who will conduct a thorough examination of your health, medical history, inform you about the necessary examinations and further treatment, and, if necessary, prescribe a PET/CT examination.
LILITA ROZNERE
Radiologist/therapist at the RUS Nuclear Medicine Clinic and Cancer Center of Latvia
Benefits of CT
CT has proven itself to be an effective way to diagnose diseases of bone structures and mechanical lesions of the head and abdominal cavity. It also has a number of positive aspects:
- High accuracy of bone images;
- Accurate detection of tumors and bleeding;
- The procedure is painless;
- Speed of research;
- The result is a three-dimensional image;
- The radiation exposure is much less than with x-rays;
- Can be used if there are metal elements in the body or electrical devices;
- Low cost, unlike MRI.