Currently, up to 15% of surgical interventions in patients admitted with symptoms of an acute abdomen are performed for small bowel obstruction. In Europe, up to 60% of cases occur due to adhesions, 20% due to various hernias, and about 15% of obstructions are associated with neoplastic processes. In the USA, 50-75% of cases are associated with adhesions, in second place are Crohn's disease and inflammatory enteritis, and in last place is oncology.
Modern diagnostic approaches include abdominal ultrasound or standing radiography as the first line of imaging. Recently, there has been an increased tendency to use the ultrasound method, which, according to some authors, can replace classical radiography. Ultrasound allows you to correctly determine the presence of small intestinal obstruction, and often reveals a lot of different additional diagnostic information that is of decisive importance for treatment tactics. The main method of final, verified diagnosis of small intestinal obstruction at the moment is SCT/MDCT with bolus contrast enhancement, being the gold standard of imaging.
According to the mechanism of occurrence, acute small intestinal obstruction is divided into:
- lumen obstruction
- narrowing of the lumen
- external compression
- intussusception
- passage blockade
- colon obstruction
- strangulation/volvulus
- complex mechanism.
The etiology and mechanisms of small intestinal obstruction are well described in many manuals and monographs, so I will not duplicate this widely available information.
Small bowel intussusception
Ileal stenosis in Crohn's disease
Radiography
In the early stage of obstruction, plain radiographs in the supine position will show moderately distended loops of the small intestine with a small amount of air. When shooting in a standing position or on the left side, multiple gas-liquid levels are determined. Kerkring's folds are visible in the early stages; as the obstruction progresses, the loops stretch and the folds become blurred. Sometimes it is very difficult to distinguish swollen loops of the small intestine from the large intestine.
Plain radiography of the abdomen in a standing position
Plain radiography of the abdomen in the supine position
Interpretation of results
The data obtained is deciphered by a specialized specialist - a radiologist. It takes no more than half an hour to obtain the results of the study. Normally, the pictures should have a speckled image.
In the presence of flakes we are talking about the development of:
- lymphosarcoma;
- lymphogranulomatosis;
- malabsorption syndrome.
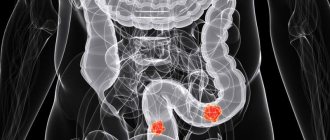
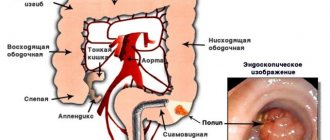
Polyps
An X-ray examination of the intestines can reveal polyps. The formations are localized on the mucous membrane and do not cause much harm. Despite this, they must be identified and removed, which eliminates the possibility of developing malignant degeneration.
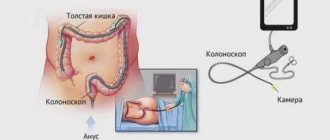
Signs of intestinal obstruction on x-ray
Intestinal obstruction has peculiar symptoms: pain in the abdomen and vomiting. In this case, intestinal motility is also impaired. The x-ray shows small intestinal obstruction in the form of a stop in the movement of contrast agent or air to other parts.
Intestinal dyskinesia
The disorder may be asymptomatic and detected during an x-ray for the first time. Intestinal dyskinesia is accompanied by insufficiency, that is, functional disorders.
X-ray signs of hypomotor dyskinesia include weakened peristalsis and intestinal tone. This is fraught with a slowdown in metabolic processes and contributes to weight gain. The development of intestinal obstruction should be highlighted as complications.
CT imaging with a simple form
Surgical classification of small bowel obstruction is also the basis of the classification used in radiology. There are three forms:
- simple/compensated form
- decompensated form
- complicated form.
-Dilated loops of the small intestine proximal to the transition zone (obstruction zone). -The transition zone should be understood as a zone of the intestine with an obvious difference in lumen diameter between the dilated proximal segment and the site of narrowing/obstruction. Visualization of this area depends on the cause and mechanism of the obstruction, as well as on the projection of the loop location (axial, frontal, etc.). Unfortunately, detecting this zone is not always possible. With an adhesive mechanism or inflammation, the sign of a “bird's beak” is well described by many. With obstruction as a result of a nutritional bolus, the transition zone will appear as a heterogeneous formation in the intestinal lumen without signs of contrast enhancement. - Collapsed loops of intestine distal to the level of obstruction. -Mixed nature of stasis of intestinal contents in dilated loops. Some authors have described the “fecaloid” type of stasis, described in the literature as “fecal contents of the small intestine”, in English literature as “small-bowel faeces sign”. The pathogenesis of this symptom includes many factors: slowing down the passage of contents, disturbances in the mechanisms of absorption and secretion in the small intestine, reflux from the colon due to insufficiency of the ileocecal valve, placement of a gastric tube. It must be remembered that this sign is nonspecific for small bowel obstruction; it can also be determined by ultrasound and plain radiograph of the abdominal cavity. -Normal non-thickened intestinal walls with homogeneous, uniform contrast enhancement. -In the jejunum, the pattern of mucosal villi (valvulae conniventes) is thin, and they look the same throughout. -Absence of pathological changes in the colon, the colon is usually collapsed or contains a small amount of fecal contents distributed throughout the lumen. - Absence of inflammatory changes in the mesentery and intraperitoneal fat. -Normal vascularization of mesenteric vessels. -Lack of free fluid in the abdominal cavity.
Various CT scans for a simple form of obstruction, schematically depict transient zones and adhesions, which, like a “collar” or “noose”, seem to strangle a loop of intestine.
The value of reconstructions in different projections to determine the level of obstruction.
Obstruction of the lumen by phytobezoar.
Obstruction of the lumen by phytobezoar.
Causes of acute intestinal obstruction
Acute intestinal obstruction can be caused by various reasons. They are divided into predisposing and producing. Predisposing causes contribute to increased mobility of intestinal loops or immobilization. This leads to the fact that the organ occupies the wrong position, and feces cannot move through it normally.
Predisposing factors can be anatomical and functional.
Anatomical reasons include:
- The presence of adhesions in the peritoneal cavity.
- Meckel's diverticulum.
- The mesentery is too narrow or too long.
- The presence of a hole in the mesentery.
- Presence of a hernia. The danger is represented by a hernia of the white line of the abdomen, inguinal and femoral hernia, as well as internal protrusions.
- Malformations of the organ, for example, mobile cecum, dolichosigma, etc.
- Peritoneal pockets.
- Tumors of the intestine or organs that are in close proximity to it.
Functional causes that can cause acute intestinal obstruction include:
- Excessive eating after a long period of abstinence. If a person has been on a diet for a long time and then eats a large amount of roughage, the intestines will begin to contract strongly. This can cause intestinal obstruction or “hunger man’s disease” (according to Spasokukotsky).
- Colitis of various origins.
- Previous spinal cord injuries, TBI.
- Trauma of a psychological nature.
- Strokes.
- Dysentery and other conditions that contribute to increased intestinal contractility.
Producing causes lead to spasms and intestinal paresis. A similar situation can be provoked by an excess of food, a sharp increase in intra-abdominal pressure, physical inactivity (forced bed rest and paralysis).
Decompensated form
All the signs described in the simple form are determined, additionally pathological changes appear in the abdominal cavity: - dilated loops of the small intestine proximal to the transition zone (obstruction zone); -collapsed intestinal loops distal to the level of obstruction; - normal, non-thickened intestinal walls with homogeneous, identical contrast enhancement; - free fluid between dilated loops of intestine, often in the form of a piquant detail of a woman’s toilet - tanga panties, therefore in many sources it is described as a sign of “tanga” (tanga sign); -free fluid in mesenteric pockets; -free fluid in the abdominal cavity.
Examples of fluid accumulation between intestinal loops (tanga) and in mesenteric pockets in the decompensated form.
Treatment of acute intestinal obstruction
If a person develops symptoms that indicate intestinal obstruction, they should be taken to a medical facility as soon as possible. Until the patient is examined by a doctor, he should not have an enema, take laxatives, painkillers, or perform gastric lavage. Treatment may involve either medication or surgery. It all depends on the characteristics of the course of the disease. With dynamic obstruction, it is possible to correct it with medication, but with mechanical blockage of the intestine, it will not be possible to do without the help of a surgeon. Often, to save the patient's life, surgery is performed on an emergency basis.
When the obstruction has just begun to develop, it is difficult to identify its form. Therefore, the doctor postpones the intervention for several hours. If taking medications does not lead to an improvement in well-being, the patient is sent to the surgical table. Provided that the patient has already been diagnosed with peritonitis or intestinal strangulation, the operation is performed immediately.
Drug correction often allows one to overcome coprostasis, as well as cope with obstruction due to a neoplasm in the intestine.
Medication correction
- Reducing pain intensity, influencing intestinal contractions.
Perinephric novocaine blockade is performed to reduce pain. Antispasmodics (Atropine, Spazgan, Drotaverine) are administered intravenously. If the patient is diagnosed with intestinal paresis, then to eliminate it, Neostigmine, a hypertonic sodium chloride solution is prescribed, and an enema is performed.
- Decompression of the gastrointestinal tract.
The stomach contents should be removed using a tube and a siphon enema, through which 10 liters of water are administered. Such measures can only be carried out if the patient has not developed peritonitis. If chyme is found in the stomach, this indicates a severe intestinal obstruction. Also, the volumes of injected fluid allow us to make an assumption about the level of obstruction. Carrying out decompression makes it possible to normalize the contractility of the intestine and improve microcirculation in its walls.
- Prevention or elimination of dehydration.
Patients with intestinal obstruction are prescribed infusion therapy. Patients are administered Ringer's solution, glucose, insulin, and potassium solution. The volumes of injected solutions are large and cannot be less than 3 liters. Soda is prescribed to patients with metabolic acidosis. During infusion therapy, blood pressure and urine output must be monitored. The patient is given a catheter in the bladder and subclavian vein.
- Bringing blood supply to the digestive organs back to normal.
For this purpose, albumin, plasma, protein, rheopolyglucin, pentoxifylline, and amino acids are used. If there are indications, the patient is prescribed cardiotropics. If the patient begins to pass gas, stool appears and the pain goes away, then this is a good sign. If after 2-3 hours the person’s well-being does not improve, he is prepared for surgery.
Surgery
If a patient develops a mechanical blockage of the intestine, surgery is required in 95% of cases. The remaining 4% of patients do not undergo it because they are in serious condition. Another 1% of patients simply do not seek medical help and die.
Contraindications to surgery for mechanical blockage of the intestine are only agony and pre-agony of the patient.
Indications for surgical intervention:
- Developing peritonitis.
- Intoxication and dehydration of the body, which corresponds to phase 2 of obstruction.
- Signs indicating intestinal strangulation.
Measures to prepare the patient for intervention:
- Placement of the probe into the stomach.
- Introduction of drugs that will ensure the functioning of the circulatory and respiratory systems.
- Carrying out massive infusion therapy.
The patient is given a catheter in the bladder, stomach and central vein. Endotracheal anesthesia is performed, and the operation is laparotomy with a midline incision. If the patient's obstruction is caused by a strangulated hernia, then spinal anesthesia can be performed.
The goals pursued by the surgeon:
- Determining the type of obstruction and performing an examination of the abdominal organs.
- Elimination of the cause that caused the blockage. The adhesions or hernia gates are dissected, and when the intestines volvulus or when a node is formed, they are eliminated. Disinvagination is also carried out, or resection of part of the affected area is planned.
- Assessment of the condition of the intestine and its possibility of further functioning. If the organ is not dead, it will have a burgundy or blue color, its mesentery is smooth, and hemorrhages are visible in some of its zones. The vessels continue to pulsate, there are no blood clots. The intestine reacts to exposure to warm saline with hyperemia, increased pulsation and contractions. Removal of the organ is required if blood clots form in the vessels; if it becomes black or dark blue, the mesentery will be dull and covered with hemorrhages. The intestine does not respond to treatment with a warm solution.
- Removal of the affected area. The part of the organ that has undergone necrosis, as well as the intestine at a distance of 40 cm from the zone of death, must be removed. Then anastomosis is performed.
- Unloading. When the organ loops are subject to excessive stretching, intestinal decompression is performed using nasogastric intubation of the small intestine with a probe. Drainage is performed through an enterostomy or cecostomy.
- Drainage and sanitation of the peritoneum. The abdominal cavity is washed with special compounds and dried. The drainage is removed through the anterior abdominal wall.
Period after surgery
If the operation is successful, the patient is placed in the intensive care unit. He must spend at least 3 days there.
Main areas of treatment and care:
- Avoiding dehydration, intoxication and infection of the body.
- Elimination of disorders of the respiratory system and cardiovascular system.
- The use of electrolytes to normalize the acid-base environment.
- Improvement of rheological blood parameters.
- Preventing the formation of blood clots. Fraxiparine is used for this purpose.
- To strengthen the body, vitamins and immunomodulators are administered.
- To prevent intestinal paralysis from occurring, its work is supported with the help of enemas, Proserin, Cerucal, electrical stimulation, etc.
In the first 3 days, the person must be in the intensive care unit. He undergoes percussion massage of the sternum and performs breathing exercises. This is necessary to normalize the functioning of the respiratory system.
The patient should be lifted out of bed as early as possible. This is done so that the intestines begin to contract and stagnation does not develop. It is recommended for the patient to get up for 2-3 days, if there are no contraindications.
For the first 3 days, a person receives parenteral nutrition. It is important to monitor his pulse, breathing rate, and the quality of the drainage discharge. During the same period, he receives antibiotics and anti-inflammatory drugs.
On days 4-7, the patient is transferred to the general ward. There he must observe semi-bed rest. The tube is removed from the stomach. From this time on, a person should receive food as usual, but it is served in semi-liquid and ground form (table 1A).
The bandage is changed on the Adam's apple for 2 days, the drainage is removed on the 4th day if there is no discharge from it.
To prevent the seams from coming apart, the patient should use a bandage. From day 5 you need to start doing gymnastics under the supervision of a doctor. The patient continues to receive vitamins, antibiotics, and immune stimulants. The menu is gradually expanding.
On days 8-10 after surgery, the person is transferred to table No. 15. He is already allowed to leave the ward.
The stitches will be removed on day 9-10. If no complications develop, the patient is discharged.
Over the next 3 months, a person will need to follow a strict menu, give up vegetables that stimulate gas formation, pickled and salty foods, fatty foods and semi-finished products.
Complicated form (most often as a result of strangulation)
Strangulation of the small intestine is characterized by thickening of the intestinal walls, vascular disorders and pronounced pathological changes in the mesentery and abdominal cavity. Diagnostic findings include: - dilated small bowel loops proximal to the transition zone (obstruction zone); -collapsed intestinal loops distal to the level of obstruction; -transient zone; - mixed nature of stasis of intestinal contents in dilated loops with a predominance of the liquid component; -thickening of the intestinal wall of a circular type. It is important to remember that this type of thickening of the walls of the small intestine with obstruction is usually associated with vascular disorders; - disruption of normal contrast enhancement of the intestinal walls. Changes range from hyperenhancement to no contrast enhancement at all. Various variations of these changes between the extremes described above can be observed simultaneously in different segments of the small intestine. The complete absence of enhancement means arterial reflex spasm and indicates the severity of the lesion; - a loop with thickened walls loses its elasticity and becomes rigid and elongated; - parietal pneumatosis of the small intestine, in especially severe cases intramural gas bubbles appear; - the appearance of pathological densities in the mesentery in the form of spreading matte infiltrates and heaviness due to hemorrhages into adipose tissue; - congestive changes in the vessels of the mesentery. At first, the diameter of the vessels increases, but over time, a reflex arterial spasm occurs, the mesentery will look depleted in vascularity. The vessels are narrowed or with a completely collapsed lumen; -gas in the lumen of the superior mesenteric vein; -gas in the lumen of the portal vein; - with torsions, the normal vascular anatomy of the mesentery is disrupted. The vessels seem to twist around the volvulus axis and pull along the modified mesenteric fat - like a snail shell or a tornado. For greater clarity, imagine a piece of straightened fabric on the table, which you pressed with your finger and began to twist without lifting your finger from the table. On CT scans you can often see a characteristic sign of a cone-shaped spiral (whirl sign); -free fluid in the mesenteric pockets and in the abdominal cavity. Sometimes the liquid may be of increased density due to the hemorrhagic component.
examples of strangulation complicated obstruction with characteristic changes in the mesentery, intraperitoneal fat, thickening of the walls of the small intestine and impaired contrast enhancement.
Twisting of the vessel during volvulus
Stages of acute intestinal obstruction
The pathology, despite its acute course, has a certain staged nature.
Experts distinguish 3 phases:
1st phase - reactive
The duration of the reactive phase is 10-16 hours. During this period, a person experiences intense pain similar to contractions. At first they are paroxysmal, with periods of calm, but later they become constant. Often the pain is so severe that the person goes into shock. Doctors call the reactive phase the “Jelius cry.”
When the reactive phase has just manifested itself, intervals without pain will be frequent, at which time the patient’s well-being returns to normal. However, when the intestines are strangulated, no clear spaces are observed. The pain goes from moderate to acute. High intestinal obstruction is accompanied by nausea and vomiting. With low intestinal obstruction, gas formation increases and there is no stool.
The pain is visceral, radiates to other organs, develops against the background of a spasm, in which the intramural nerve plexuses are irritated. Subsequently, intestinal motor function becomes depleted. The intestines become swollen and greatly stretched. As swelling increases, the pain becomes constant and intense. There are no periods of enlightenment.
Phase 2 - intoxication
After 12-36 hours, a toxic phase develops, in which paresis of the organ is observed. The pain becomes constant, the intestines stop contracting, the stomach swells and takes on an irregular shape.
The person develops vomiting, it is profuse, and it is impossible to stop it. The intestines will be full during this period, as will the stomach.
A man refuses water because he feels sick all the time. This leads to dehydration of the body, minerals, electrolytes, and enzymes are removed from it. The face becomes like a mask (the face of Hippocrates), the oral mucosa dries out, and the patient himself is very thirsty. He gets severe heartburn. Neither feces nor gases come out.
During this period, Valya's symptom, Sklyarov's symptom, Kivul's symptom, and symptom of peritoneal irritation appear. The lists function suffers. Since a lot of fluid accumulates in the intestines, it begins to leak through its walls. This becomes the first step towards the development of inflammation of the peritoneum.
Phase 3 - terminal
After 36 hours, the final stage of pathology develops. In this case, all organs are affected. The person begins to breathe quickly, body temperature rises to feverish levels, and there is no urination. The abdomen is no longer protruded forward, blood pressure drops, and the pulse becomes very rapid, but weak.
From time to time the patient vomits, which gives off the smell of feces. Then the patient develops blood poisoning, internal organ failure and death.
Ultrasound signs of small bowel obstruction
The main ultrasound signs of obstruction are visualization of dilated loops of the small intestine, decreased peristalsis, free fluid between the loops (tanga) and in the abdominal cavity. Also, ultrasound can sometimes detect the cause of the obstruction, for example, a tumor, thickening of the walls of the terminal segment of the ileum in Crohn's disease, etc. Ultrasound can solve the diagnostic dilemma when there are ambiguous radiological signs on a plain abdominal radiograph. The limit of the method is the low specificity in assessing the condition of the mesentery, as well as the dependence of the quality of diagnosis on the patient’s constitution and the operator’s experience.
The topic of intestinal obstruction as a result of intussusception will not be covered in this review; it is well described in many domestic and foreign publications. I think that all colleagues dealing with this problem know that ultrasound diagnostics is of decisive importance in the diagnosis of intussusception. An indicative observation was previously posted on our website:
examples of sonograms with dilated loops of the small intestine
Ultrasound makes it possible to perfectly locate free fluid in the abdominal cavity
What is intestinal obstruction?
Intestinal obstruction
– a pathology in which the process of evacuation of substances from the intestines is disrupted. It is especially characteristic of vegetarians and can be dynamic or mechanical.
At the first suspicion of intestinal obstruction, you should immediately contact a surgeon for help. Only he can make a final diagnosis and recommend the necessary treatment. Deciding solely on traditional methods on your own is very dangerous.
Acute obstruction can cause death, which is why it is so important to know its main symptoms and causes.
Statistics:
- After emergency surgery for intestinal obstruction, about 20% of patients die. If the pathology was severe, then these figures increase to 40%.
- Among all acute conditions requiring surgical treatment, ACI (abbreviation for acute intestinal obstruction) occurs in 8-25% of cases.
- If the cause of intestinal obstruction is a tumor, then the number of deaths is 40-45%.
- When the cause of acute intestinal obstruction is adhesions, death occurs in 70% of cases.
- In men, pathology occurs more often than in women - in 66.4% of cases.
- At risk are older people, whose likelihood of developing ACI increases 4 times.
Content:
Paralytic ileus
Paralytic or adynamic obstruction means a violation of passage through the intestines without the presence of mechanical obstruction of the lumen as a result of a decrease or complete absence of intestinal tone and peristalsis. Both the small and large intestines may be affected. Involvement of the stomach in the process reflects the seriousness of the situation. Paralytic ileus presents with complex radiological symptoms. We will limit ourselves to listing the main points that are always visualized in this pathology: - expansion of the intestinal lumen; - intestinal stasis with a predominance of the liquid component and air levels; -decreased tone and peristalsis. Dynamic monitoring of the listed signs is very important, which gives the palm to ultrasound as the most adequate and safe visualization method for adynamic obstruction.
Safe radiation dose for x-rays
Radioactive radiation affects a person all the time and does not harm him in small doses. It is impossible to avoid its influence, since the entire surface of the Earth is exposed to irradiation from space, and some of the natural radionuclides are in the external environment (the earth's crust, water, air). Doses of radiation absorbed by the body are measured in millisieverts (mSv). Natural background radiation is approximately 2 mSv per year.
For the safety of X-ray examinations, the maximum permissible radiation dose per year (MAD) was established at 100 mSv per year. This is the maximum allowable amount of radiation doses received per year that will not cause harm to human health.
With an X-ray of the chest area (CH), a person receives only 0.1 mSv, and with an X-ray of the hip joints - 1.47 mSv, which is much less than the permissible level. During spondylography (the so-called image of the back), the radiation dose is 1.5 mSv. With OGK fluoroscopy (a radiation diagnostic method that allows real-time monitoring of the condition of the tissues and bone structures of the chest area), the patient receives 1.4 mSv in 1 minute of examination.
Radiation readings may vary depending on the X-ray machine used. The more modern it is, the lower the radiation dose. The safe dose of radiation exposure for preventive studies is 1-2 mSv per year. The vast majority of medical examinations that use x-rays use low-energy x-rays that irradiate the body for a fraction of a second and are therefore considered virtually harmless to humans even when repeated many times.
How are x-rays done?
The need to prepare for the procedure depends on the type of examination to be performed. If an x-ray of the abdominal region or the lumbosacral spine is prescribed, then three days before the procedure it is necessary to exclude from the diet foods that contribute to increased gas formation. An X-ray of the intestines may additionally prescribe a cleansing enema or laxative. Several hours before the test you should not smoke, eat or drink.
Before the procedure, you must remove your jewelry, belt, and remove metal objects from your pockets. When taking an X-ray of the spine or chest, you must undress to the waist. X-rays of the phalanges of the hands and feet can be performed in clothing. Those parts of the body that are not being examined should be covered with a protective lead apron or cap. The doctor also puts on a special suit and goes into the next room, from where he controls the X-ray machine.
After the procedure, the patient is given an image or the examination result is recorded on digital media (flash card) in the case of digital x-rays. In the diagnostic protocol, the radiologist indicates the level of radiation exposure to which the patient was exposed.
Which is safer: X-ray or CT?
X-rays are safer for health, but the value of CT as a diagnostic method is much higher. CT allows you to obtain information about the condition of bones, soft tissues and blood vessels in a three-dimensional projection. Computed tomography is a method of non-invasive examination of human internal organs that uses x-rays. However, unlike X-rays, the radiation doses from CT scans are much higher due to multiple scans.
CT allows you to achieve a three-dimensional image thanks to the design of the device: the source of rays is a contour in the shape of the letter C, inside of which there is a couch for the patient. This allows you to take a series of images of organs from different angles, which are processed by a computer and create a three-dimensional image. In addition, the doctor has the opportunity to look at a cross-section of the organ, which, depending on the settings of the device, can reach a thickness of only 1 mm.
It is estimated that approximately 0.4 percent of cancers are caused by CT scans. Some scientists expect this level to rise in parallel with the increased use of CT scans in medical procedures. Experts estimate the risk of developing cancer from undergoing one CT procedure as 1:2000.
At what age do children get x-rays?
X-rays are prescribed to children of any age, but only if indicated and when other research methods do not provide the necessary diagnostic information. The advantage of this procedure is that the ability to make an accurate diagnosis justifies the risk associated with radiation. When radiography is performed on children, it is necessary to minimize exposure to ionizing radiation because:
- children are more sensitive to the effects of X-rays than adults, that is, the risk of cancer per unit dose of ionizing radiation is higher;
- the use of equipment and radiation settings intended for adults may result in excessive exposure of children;
- Children's life expectancy is expected to be longer, so the risk of cancer from radiation exposure is potentially higher than in adults.
In order to minimize possible harm to health, X-rays for children are performed using the lowest dose of radiation, which gives an image quality suitable for diagnostics. X-ray examination is performed for preventive purposes for children from 14 years of age.