Role in the body
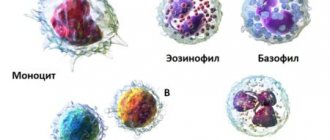
Mononuclear cells are divided into monocytes and lymphocytes. The first cells absorb foreign microorganisms and bacteria, and also spread information throughout the human body that an infection has invaded. Lymphocytes are responsible for producing antibodies that are necessary to fight pathogenic agents.
It is thanks to B-lymphocytes that strong immunity to various infectious diseases is developed. Immune memory makes it easier to endure re-infection without complications. In most cases, mononuclear cells in the blood indicate the development of a serious pathology.
Prevention and prognosis
To date, there is no specially designed prevention program that helps to avoid the fact that the level of mononuclear cells in a child’s blood will be increased (as in an adult).
You can reduce the likelihood of developing a deviation by following simple rules:
- maintaining a healthy and active lifestyle;
- balanced and nutritious nutrition;
- compliance with personal safety rules when in contact with toxic substances;
- constant strengthening of the immune system;
- adequate use of medications - only those prescribed by the clinician;
- identification at the initial stages of the course of those diseases that can provoke pathology;
- annual full preventive examination in the clinic - donate blood for laboratory studies and undergo instrumental examinations.
The prognosis depends on the etiological factor. If you refuse qualified help, the possibility of worsening the underlying problem and the development of life-threatening complications cannot be ruled out.
Kinds
Mononuclear cells have a simple, non-segmented nucleus and lack specific granularity. There are the following types of cells that allow us to talk about the deviation of mononuclear cells, the severity of the disease and the effectiveness of the therapy:
| Name | Description |
| Lymphocytes | Formed elements whose responsibilities include cellular immunity. They produce antibodies to bind and kill pathogens. The same thing happens to the cells of your own body if they are infected. Lymphocytes also have the ability to distinguish cancer cells in the blood and kill them. |
| Monocytes | Leukocyte cells whose responsibilities are the immune response and the synthesis of cytokines. They can distinguish a damaged cell, pathogenic flora or bacteria, damaged tissue as a result of inflammation and neutralize them. |
During a comprehensive examination, the level of these cells is determined, which helps to identify changes in the level of mononuclear cells. A hematologist will help you decipher the diagnostic results and establish the disease.
Treatment
Therapeutic tactics for high numbers of mononuclear cells depend on the disease and severity, the presence of complications that it caused. Conservative therapy may include the following groups of drugs:
- immunomodulators;
- hormonal drugs;
- hepatoprotectors;
- vitamins, minerals, multivitamin complexes;
- antiviral, antifungal agents;
- antibiotics;
- enzymes;
- antiparasitic drugs;
- anti-inflammatory drugs.
These drugs are selected individually depending on the symptoms and type of pathogen. If the increase in mononuclear cells is caused by tumor processes, radiation therapy and chemotherapy are prescribed.
Important! Most often, diseases that cause an increase in mononuclear cells require combination treatment, that is, a combination of drugs from different groups.
Reasons for the appearance of atypical cells in the blood
Mononuclear cells and other changes in the general blood test are provoked by numerous factors:
- helminth infection;
- suspicion of systemic lupus erythematosus, vasculitis;
- mononucleosis caused by the Epstein-Barr virus;
- acute viral diseases;
- immunodeficiency conditions;
- pathologies of bacterial origin (pneumonia, tuberculosis, endocarditis);
- individual sensitivity to certain medications;
- malignant or benign processes in the human body;
- anemia;
- kidney or liver diseases, which are accompanied by severe intoxication;
- food poisoning;
- overdose of medications.
In a child’s body, a change in the level of atypical cells occurs for the following reasons:
- autoimmune processes;
- oncological diseases;
- vaccination;
- severe intoxication of the body;
- pathological changes in the blood;
- long-term use of certain medications.
A hematologist will help you establish an accurate diagnosis and decipher the research results, as well as select the most effective treatment. A specialist who specializes in blood diseases. Considering the provoking factor that caused the change in mononuclear cell levels, the patient may need to consult other specialized doctors.
What are atypical mononuclear cells, what is their role in the child’s body?
Mononuclear cells are mononuclear blood cells. There are no granules in their cytoplasm (internal environment), so they are also called agranulocytes. Mononuclear cells include lymphocytes and monocytes, which play a special role in the child’s body. Lymphocytes are the main cells of the immune system, responsible for producing immunoglobulins to fight infections. Monocytes have the ability to absorb and neutralize harmful agents, while simultaneously signaling lymphocytes about the entry of foreign elements into the blood.
When some viruses enter the body, cells begin to change. Their size increases several times. The transformed blood element has a small nucleus surrounded by a large layer of cytoplasm. This is how atypical mononuclear cells (virocytes) are formed. If the level of altered cells significantly exceeds the norm, this signals infection with a dangerous disease - infectious mononucleosis, caused by the Epstein-Barr virus.
Mononuclear cell norms in adults and children
Mononuclear cells in a general blood test, namely their level depends on the person’s age:
Mononuclear cells in the general blood test (leukocyte formula) are normal
| Age | Monocyte count (%) | Lymphocyte count (%) |
| 0-5 years | 4-10 | 16-32 |
| 5-10 years | 4-7 | 40-60 |
| 10-15 years | 3-6 | 35-50 |
| 15-20 years | 3-7 | 30-45 |
| 20-50 years | 3-7 | 30-45 |
| over 50 years old | 4-8 | 35-50 |
Serious deviations from established norms indicate the development of a certain disease. Additional comprehensive diagnostics will help clarify the diagnosis.
Norms of indicators in children
The norm for increased agranulocytes in a child’s blood is 0-1%. Their number increases slightly (up to 10%) in autoimmune diseases and tumors. The highest level of atypical mononuclear cells in the CBC of a child is present in infectious mononucleosis. Sometimes their number exceeds 50% of white blood cells.
To confirm the diagnosis, blood is taken twice with an interval of five days. At the initial stage of the disease, the number of atypical cells is 10%. After a week, the number reaches a maximum of 60-80%.
Indications for examination
The patient comes to the hospital with certain complaints and existing symptoms, taking into account which the pediatrician or therapist prescribes an examination.
There are the following indications for diagnosis:
- infectious and viral diseases;
- food or medication poisoning;
- blood disease;
- miliary tuberculosis;
- applastic anemia;
- liver failure;
- treatment with cytostatics;
- pyogenic infections;
- state of shock.
During pregnancy, the level of mononuclear cells may change. The same applies to vaccinations, tumors, autoimmune pathologies, and HIV infection. A blood test for mononuclear cells is also prescribed to patients before surgery or before vaccination. Research will help ensure that there is no hidden infection and monitor the treatment being carried out.
What to do if there is a high level of mononuclear cells in the blood?
If the baby’s blood test shows a high level of atypical mononuclear cells, you should contact your pediatrician. He will assess the general condition of the baby, taking into account recent illnesses. This is necessary, since a viral infection affects the level of virocytes in the blood. After it, it may remain elevated for several more weeks.
If the baby’s diagnosis of EBV infection is confirmed, his treatment is limited to combating the existing symptoms. It includes agents that reduce fever, act as antiseptics and have a general strengthening effect. There is currently no specific therapy to help overcome the Epstein-Barr virus. Typically, this disease is characterized by a mild form and children recover completely. With rare exceptions, this virus causes:
- hepatitis A;
- splenic rupture;
- swelling of the larynx.
If the liver has been damaged, the child requires a certain diet supplemented with medications that have a hepatoprotective and choleretic effect. If there is a bacterial infection, antibiotics and probiotics are also used. If the disease is severe or accompanied by serious complications, it is likely that hormonal drugs, tracheostomy or artificial ventilation of the lungs, or removal of the spleen will be prescribed.
Infectious mononucleosis virus
In some situations, changes in blood cell levels occur due to the Epstein-Barr virus. Infection of the human body occurs through airborne droplets during direct contact with a patient or a carrier of pathogens. There is also a risk of transmission of infection from mother to child (placental).
Adolescents and young adults are more likely to experience infectious mononucleosis (90%). The main feature of the disease is the damage to all lymph nodes in the human body, tonsils, spleen and liver.
Mononuclear cells in a general blood test above the established norm cause characteristic symptoms:
- body temperature rises;
- pain appears during swallowing;
- a specific plaque forms on the tonsils;
- the patient is concerned about symptoms of intoxication (weakness, nausea);
- there is congestion in the nasal passages, against which the patient snores at night;
- cervical lymph nodes enlarge;
- The sclera and skin turn yellow.
The time from infection to the appearance of the first signs of the disease is 5-60 days. In most cases, infectious mononucleosis resembles a sore throat, but an accurate diagnosis must be made by a pediatrician or therapist. If necessary, the specialist prescribes a comprehensive diagnosis, the results of which will help make the correct diagnosis.
Why do mononuclear cells increase?
There are many factors or diseases that lead to an increase in the number of virocytes, and all of them are associated with the entry of a viral or bacterial infection into the body.
These include the following reasons:
- Infectious mononucleosis;
- autoimmune diseases;
- polycythemia, leukemia;
- fungal infection;
- parasitic diseases;
- tuberculosis, purulent processes;
- digestive tract infections.
It should be noted that the highest level of virocytes is detected in infectious mononucleosis. This disease develops as a result of the Epstein-Barr virus, therefore it has the second name EBV infection. Almost always, the pathology is accompanied by an increase in atypical mononuclear cells over 10%, which is the main diagnostic sign confirming this disease.
The source of infection is an infected patient or healthy person (carrier), in whose body there is a virus, but due to good immunity the disease does not develop. Most often, the pathology is transmitted through patients who, due to an unexpressed symptomatic picture, do not seek help from the hospital, as a result of which the disease is not identified.
The route of transmission can be contact, household (through common objects) and airborne droplets. The incubation period for infectious mononucleosis is quite long, and about 2 months can pass from the moment of infection to the appearance of the first signs.
Main manifestations of infectious mononucleosis
Extensive medical practice shows that babies under one year of age rarely suffer from infectious mononucleosis, which is explained by innate passive immunity transmitted from the mother. In addition, it has been established that this disease is most often observed in older children - 7-10 years old and, as a rule, in boys.
The duration of the acute phase of the disease is 15-20 days. As the infection develops, it affects the nasopharyngeal tonsils, lymph nodes, spleen and often the liver. But first of all, the immune system suffers, since initially it has to resist a serious pathogen.
Then, against the background of reduced immunity, in most cases various infections begin to occur, accompanied by complications such as otitis media, pneumonia, tonsillitis, etc. In some cases, the leukocytes of a child or adult with EBV infection consist of more than 50% virocytes.
The main role in the diagnosis of this and other infectious diseases is played by the results of laboratory tests. With their help, it is possible to establish a diagnosis relatively quickly and accurately, develop therapeutic tactics and conduct regular quality control of treatment. After recovery, the patient must be observed by a hematologist for at least a year and have his mononuclear cell levels checked.
Symptoms
Diagnostic measures will help to accurately determine abnormalities associated with mononuclear cells in the blood.
However, there are clinical signs that will allow you to suspect problems and promptly go to the hospital:
- a large amount of sweat is released;
- the person complains of general weakness and weakness;
- joint and muscle pain occurs;
- sudden fever appears;
- decreased ability to work;
- the skin becomes very pale;
- The cervical lymph nodes become enlarged and pain appears during palpation;
- a person breathes more often through his mouth;
- the voice becomes hoarse;
- shortness of breath appears;
- appetite worsens;
- sleep is disturbed, daytime sleepiness appears;
- mucous membranes and sclera turn yellow;
- hepatosplenomegaly develops.
In most cases, changes in the level of mononuclear cells in the blood occur as a result of the development of a specific disease. Therefore, the patient will also have characteristic signs of concomitant pathology.
Signs
It is very important not to miss signs of atypical mononuclear cells in the blood. Since the first cause is mononucleosis (herpes type 4), the causative agent of which is EBV, you should first pay attention to the throat. White plaque, pustules, and painful sensations should alert you. Due to a decline in immunity, herpetic sores may appear on the skin. Body temperature increases. The jump will most often be high (with a bacterial etiology of the disease, a low-grade condition is observed). The lymph nodes of the submandibular as well as the cervical region are enlarged. Nasal congestion, runny nose, and painful sensations when swallowing appear.
Attention! In case of mononucleosis, at a doctor’s appointment after examining the throat, the abdominal cavity is palpated. The spleen and liver may be greatly enlarged. In the acute period, these organs will be enlarged.
By carefully observing, you can see the following development of the disease in children:
- a sharp rise in temperature, fever against this background;
- painful sensations in the head, joints and muscles;
- on the second day, symptoms appear in the tonsils;
- cough;
- abdominal pain;
- skin disorders (herpes, jaundice).
Diagnostics for deviations from the norm
The main method of diagnosis is a general and biochemical blood test. The examination is prescribed by a hematologist, taking into account the person’s complaints and his condition. It is important to differentiate the disease, since many symptoms of the disorder are similar to other pathologies (ARVI, diphtheria, viral hepatitis, acute leukemia).
In addition to laboratory tests, the patient is prescribed additional diagnostic methods, taking into account the results of a general blood test:
- Ultrasound examination of the abdominal organs (ultrasound);
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- chest x-ray;
- fibrogastroduodenoscopy (FGDS).
To clarify the diagnosis, taking into account the provoking factor and concomitant disease, the patient may be prescribed a biopsy.
Diagnostics
The main diagnostic criterion is a general blood test. The procedure requires minimal preparation: avoiding eating on the day of the examination and minimizing physical activity. The interpretation of the results is carried out either by the attending physician or by a hematologist.
To accurately determine the cause of the disorder, a whole range of diagnostic measures is necessary:
- studying the medical history - can immediately indicate the underlying disease;
- collection and analysis of life history;
- familiarization with family history;
- palpation and percussion of the abdomen;
- study of the condition of the skin, mucous membranes and sclera;
- measurement of heart rate and temperature;
- a detailed survey of the patient - to clarify the full symptomatic picture;
- blood chemistry;
- microscopic examination of feces;
- general urine analysis;
- culture of blood and feces;
- serological tests;
- PCR tests;
- hormonal and immunological tests;
- Ultrasound of the peritoneum;
- irrigoscopy;
- FGDS;
- CT and MRI of internal organs;
- biopsy.
Consultations with specialists such as: endocrinologist, nephrologist, infectious disease specialist, gastroenterologist, immunologist may be required.
Preparation for blood and urine tests
The procedure for collecting biological material requires compliance with the minimum rules to obtain the most accurate results:
- On the day of the examination, the patient is not recommended to eat.
- Before the analysis, it is necessary to completely eliminate physical activity.
- The day before blood sampling, it is recommended to refrain from drinking alcohol, fatty and fried foods.
- A week before taking the study material, you must stop taking medications.
- In the morning before the examination, it is not recommended to brush your teeth; it is enough to rinse your mouth.
- Before starting urine collection, hygiene procedures must be carried out.
Immediately before the blood test, patients should rest well and relax for 15-20 minutes.
Signs of increased mononuclear cell levels
Symptoms of a large number of virocytes in the blood may be as follows:
- heat;
- increased sweating;
- enlarged lymph nodes in the neck and under the jaw;
- pain and sore throat;
- hoarseness of voice;
- runny nose;
- swelling of the pharyngeal mucosa;
- rashes on the skin;
- hyperemia of the throat mucosa;
- general weakness.
In a child, increased mononuclear cells are accompanied by an increase in the size of the spleen and liver.
The incubation period for infectious mononucleosis lasts from one to two weeks. After this, the upper respiratory tract begins to be affected.
If there are symptoms of elevated levels of mononuclear cells in children, it is necessary to consult a specialist and undergo an examination to exclude or confirm suspicion of the disease.
How are the tests carried out and what do they show?
Mononuclear cells in a general blood test and the viral infection that provoked their appearance will help determine the following diagnostic measures:
| Name | Description |
| General blood analysis | Test results show moderate leukocytosis. The leukocyte formula contains wide-plasma lymphocytes (atypical mononuclear cells). |
| General urine analysis | The results of laboratory tests will help establish a complete picture of the inflammatory process, against the background of which the level of mononuclear cells has increased. |
| Biochemical analysis | The level of aldolase and alkaline phosphatase increases. Jaundice is indicated by increased bilirubin. |
| Linked immunosorbent assay | Specialists determine specific antibodies. The results allow us to identify the Epstein-Barr virus and determine the degree of development of the disease. |
| Chemiluminescence immunoassay | The test helps confirm the presence of IgG antibodies. Questionable results obtained require re-testing after 5 days. |
| Polymerase chain reaction | The most informative diagnostic method that will show accurate results even with a minimal number of pathogenic cells. PCR also helps to identify the DNA of the causative agent of the disease and create the most effective treatment regimen. |
| Monospot test | A diagnostic method that allows you to detect acute infectious mononucleosis in the first 2-3 months after infection of the human body. Chemical reagents are used during the study |
If necessary, the patient is prescribed a consultation with other specialized specialists (endocrinologist, nephrologist, infectious disease specialist, immunologist, gastroenterologist).
Lab tests
Blood tests in adults and children, their interpretation are an important condition for determining the number of mononuclear cells and prescribing the necessary type of treatment. The procedure is very important, as it makes it possible to detect human pathological conditions at an early stage.
How is the analysis for the presence of such cells carried out?
During diagnosis, changes in the level of pathological cells are analyzed. To do this, the doctor determines normal red blood cells and counts all monocytes and lymphocytes. If there are more than 10% of pathologically altered leukocytes, it is considered that the person is suffering from an acute form of the pathology.
Often, specialists detect from 5 to 10% of changed cells.
Change in blood picture
The number of altered blood cells indicates how aggressive a particular pathology is. Sometimes the number of virocytes in the blood can reach 50%. This happens very rarely when a person first experiences an infection.
If the number of mononuclear cells in a child’s general blood test significantly exceeds the normal number, then other diagnostic methods must be used. They allow you to determine the state of the blood in doubtful cases. Sometimes a significant appearance of atypical cells occurs in the acute phase of the disease. To make a correct diagnosis, you need to repeat the analysis - after about a week.
During the acute phase of the inflammatory process, it is necessary to check the ferritin level. Its concentration increases during the acute phase of the inflammatory process.
How to take a blood test for mononuclear cells correctly
The presence of atypical mononuclear cells in a general analysis can only be accurately determined if the blood sampling procedure was carried out correctly. The material for the diagnostic procedure must be submitted in the morning, before the morning meal. It is forbidden to consume not only any food, but also juices and tea.
Read also Estradiol in women: norms and causes of deviations
Before a blood test, you should limit physical activity. It is best to sit quietly for 15–20 minutes.
Decoding the results. How are mononuclear cells designated?
Only a pediatrician, therapist or hematologist can fully examine the examination results. The specialist, guided by the data obtained, will make an accurate diagnosis.
A general blood test shows:
- increase in atypical cells by 10%;
- increase in monocytes by 40%;
- lymphocytes increased by 10%;
- the total number of lymphocytes and monocytes is 80-90% when compared with the total number of leukocytes.
White blood cells and erythrocyte sedimentation rate (ESR) will be slightly increased. The same applies to neutrophils (by 6%).
Blood test for monocytic sore throat
The thing is that with monocytic tonsillitis, mononuclear cells look completely different from those of a healthy person. At the height of the disease, a general blood test for mononucleosis can show the usual changes characteristic of inflammation and viral infection. This is moderate leukocytosis, neutropenia, that is, a decrease in the number of neutrophils, and an increase in the number of lymphocytes and monocytes, and this laboratory phenomenon is called mononucleosis. Mononucleosis as a laboratory phenomenon occurs in many viral infections. But it is precisely with this disease that atypical mononuclear cells appear in the blood.
These are lymphocytes. They differ from the usual ones:
- larger sizes;
- their nuclei are like those of monocytes;
- in this case, the protoplasm is stained with basic dyes, that is, it is basophilic in nature and surrounds the nucleus with a wide rim.
Morphologically, it turned out that in the early stages of the disease, B-lymphocytes act as mononuclear cells, the cytoplasm of which contains special immunoglobulins, which are produced in response to the introduction of the virus, and then circulate freely in the blood. At the height of the disease and towards the end, the baton is taken over by T-lymphocytes, which make up the majority of the population of atypical mononuclear cells. Their second designation is virocytes. In fact, virocytes in the blood are not at all “overwhelmed” with viruses. These are our immune cells in the active fight against the virus.
In order to see them, you don’t need any complex methods at all: PCR, enzyme immunoassay and other methods. A simple blood test is enough. It is necessary to prepare, dry, fix and stain the smear and calculate the leukoformula under a microscope.
Typically, the number of atypical mononuclear cells in the blood correlates well with the clinical manifestations and duration of the disease. The height of the disease is characterized by an exceptionally high number of mononuclear cells, and when determining the percentage, it turns out that it often reaches 90% of all monocytes and lymphocytes.
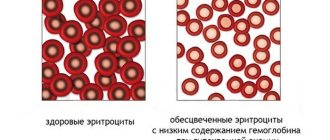
Against this background, the analysis usually does not show any anemia, the number of red blood cells and hemoglobin level remain normal, the number of platelets may vary. So, at the height of the disease at the height of the fever, their number decreases, but this laboratory sign is unstable and is usually not taken into account, just like the erythrocyte sedimentation rate. It may be normal, or even slightly above normal.
After normalization of temperature and reduction of peripheral lymph nodes, the number of leukocytes normalizes and the number of atypical mononuclear cells decreases. They are not so “conspicuous” when studying a blood smear, or, as laboratory assistants say, they begin to show less polymorphism. Plasma cells, or B-lymphocytes, completely disappear, and during the recovery period, ordinary lymphocytes predominate in the leukocyte formula. Sometimes, with a drop in temperature, the relative number of eosinophils increases slightly, but this symptom cannot be considered obligatory.
Clinically, things don't look so smooth. Mononucleosis is most easily tolerated by children, but if the disease occurs in adults, the period of convalescence, or recovery, sometimes lasts a long time, well-being is restored slowly, as well as ability to work. In the evenings, a slightly elevated temperature may bother you for a long time. As for the enlargement of the lymphoid tissue of the spleen and liver, it can remain restless for even several months after recovery and discharge from the hospital, manifesting itself in an enlarged liver and spleen. As for the tendency to mild leukopenia and lymphocytosis, they can last up to 2 years.
This sign occurs only in this infection and is therefore pathognomonic. What it is? This is the name of a bright, peculiar symptom that alone signals the presence of any disease, and occurs only with it. Thus, in infectious diseases, a pathognomonic symptom is the detection of Belsky-Filatov-Koplik spots on the oral mucosa. This phenomenon is characteristic of measles infection. If an ophthalmologist notices a red ring on the patient’s iris, then this is a copper deposit, and this symptom will be pathognomonic for Wilson-Konovalov disease, or hepatocerebral dystrophy. In medicine, there are many other pathognomonic symptoms, the accidental discovery or conscious search of which can greatly simplify diagnosis.
Now the dear reader knows what atypical mononuclear cells are, what it means if these cells appear in the blood.
How are abnormal mononuclear cells treated?
Mononuclear cells in a general blood test often indicate the development of a viral infection. Treatment of patients is carried out in most cases comprehensively and on an outpatient basis. The doctor prescribes medications, taking into account the results of the examination and the individual characteristics of the human body.
The main goal of therapy is to support the proper functioning of the immune system and eliminate the symptoms of the existing disease, as well as cope with the source of pathological processes.
Patients are prescribed the following medications:
| Group of drugs | Name | Application |
| Antipyretics | Ibuprofen, Paracetamol | Medicines help reduce high body temperature. Capsules should be taken orally, taking into account the time interval of 6-8 hours. The recommended dosage for adults is 200-400 mg 3-4 times a day. The medicine is taken short-term for 2-3 days. |
| Topical anti-inflammatory medications | Strepsils, Faringosept | Infectious mononucleosis causes a sore throat. Medicines help reduce discomfort and discomfort. It is recommended to dissolve 1 lozenge every 2-3 hours. The maximum daily dosage is 8 tablets. Therapy continues for 3 days. |
| Antibacterial drugs | Amoxicillin, Ciprofloxacin | Medicines are prescribed to patients in case of a bacterial infection. The dosage is calculated taking into account the weight and age of the patient. Adults and children over 2 years of age are prescribed 125-500 mg once a day. For small patients, the dosage is calculated taking into account body weight. It is 20-100 mg/kg 2-3 times a day. |
| Choleretic agents | Allohol, Hofitol | The drugs enhance the production of bile and support the functioning of the liver. The adult dosage is 1-2 tablets 3-4 times a day. Children are prescribed 1 tablet 3 times a day for a month. |
| Antiviral drugs | Anaferon, Viferon | The medicine is taken orally before or after a meal. The tablet should be kept in the mouth until it is completely dissolved. On the first day, the patient is prescribed 1 tablet every 30 minutes for 2 hours. Then you need to take 3 more tablets at regular intervals. Starting from the second day of treatment, you should take 1 tablet 3 times a day until complete recovery. |
| Immunomodulators | Immunal, Imudon | It is recommended to take the medicine orally with a sufficient amount of water. The standard dosage for an adult is 1 tablet 3-4 times a day. The duration of treatment takes 1-8 weeks. |
To strengthen the immune system, patients are prescribed vitamin complexes. Medicines have anti-inflammatory and analgesic effects. Additionally, patients are advised to adhere to a strict diet, since the virus has a strong negative effect on the liver.
| Recommended Products | Prohibited Products |
|
|
During therapy, the patient should also refrain from any physical activity; it is important to maintain bed rest. For 1-2 weeks, eat right and adhere to the drinking regime. After treatment, the patient should be observed by a doctor for another 6 months to prevent a relapse of the disease.
It is impossible to avoid increasing the level of mononuclear cells in human blood. There are only general recommendations from a hematologist.
In other situations, the main thing is to go to the hospital in a timely manner with alarming signs and undergo a full examination to make an accurate diagnosis. The results of a general blood test and other tests are necessary for a specialist to draw up an effective treatment regimen.
Prevention
Considering that changes in the number of atypical mononuclear cells can be associated with various diseases and types of pathogens, there are no exact preventive measures. But, since most often a high rate is observed in infectious diseases, nonspecific prevention is necessary aimed at increasing immunity:
- health procedures (for example, hardening);
- adaptogens;
- immune stimulants;
- vitamin preparations, especially in the autumn-spring period;
- playing sports;
- rejection of bad habits.
Also, preventive measures include the use of medical masks when communicating with infected people (applies to airborne diseases). Children who have been in contact with patients with infectious mononucleosis are given emergency vaccination with a specific immunoglobulin.
Exceeding the permissible values of atypical mononuclear cells always means that a pathogen has entered the body. The severity of deviations from the norm depends on the state of the body and the immune system. According to statistics, cell levels increase in children aged 2 to 10 years, which is associated with a high risk of contracting infectious mononucleosis.
What do mononuclear cells look like?
Mononuclear cells are even larger leukocytes than lymphocytes, which are the largest among all leukocytes. In mononuclear cells, despite their large lymphocytic size, the nucleus is very similar to that of monocytes, and these cells have a wide belt of cytoplasm, which is well stained with basophilic dyes. Their number increases, and at the height of the disease can exceed 30%, often making up the overwhelming number of all leukocytes - up to 60%, and even up to 90% of all leukocytes. Such a high absolute mononucleosis in the peripheral blood is a characteristic pathognomonic sign of the disease of the same name.
At the same time, all other indicators of red blood - the number of red blood cells, color index and hemoglobin level are not changed. The number of platelets in infectious mononucleosis can decrease sharply, including a decrease to 30 thousand, but quickly returns to normal. ESR does not change significantly in infectious mononucleosis. The illustration below shows atypical mononuclear cells “in the interior”, against the background of red blood cells, which allows us to draw a conclusion about their true size.
During convalescence, or during the recovery period, the number of atypical mononuclear cells begins to decrease quite quickly, they cease to be different, and they all look the same. As laboratory technicians say, their polymorphism disappears in a general blood test. Despite this smoothing, the number of lymphocytes remains predominant over neutrophils in the leukoformula.
During the recovery period, due to an increase in mononuclear cells, there is a phenomenon of granulocytopenia, or a decrease in the number of granulocytes, which include the leading neutrophils in a healthy person. The lower the temperature in patients during the recovery period, both in adults and in childhood, the greater the chance of an increased number of eosinophils appearing in the peripheral blood, but within low limits - up to 9%.
Why and how to diagnose virocytes
To identify mononuclear cells, a small patient will have to donate blood for clinical testing. Studying the cells and counting them helps to correlate them with the amount of other blood components and make a final verdict - whether virocytes are elevated or not. Mononuclear cell percentages are significant in the following cases:
- If the child undergoes a routine examination. It happens that the baby’s parents don’t even suspect a change in the blood composition, and the child’s complaints are “written off” to the increased workload at school. Identification of virocytes makes it possible to identify the most serious illnesses in the early stages of development, which means that the likelihood of a cure increases. Preventive medical examinations for children in hospital conditions are initiated 1 or 2 times a year.
- The child complains of a sore throat, weakness, lethargy, apathy, nothing makes him happy. The baby doesn’t know anything about depression yet, so the pediatrician immediately discounts this option.
- If a chronic illness for which the child is registered has worsened. Children who get sick almost immediately after getting rid of a cold or virus deserve special attention. A blood test can determine the presence or absence of protective antibodies in the plasma.
- Research is also important if a child is scheduled for surgery.
Additional symptoms of the disease
Other characteristic symptoms that are visible to an experienced doctor at the patient’s bedside can also help make the diagnosis of infectious mononucleosis. Usually, along with the general infectious onset of the disease, with an increase in temperature to febrile levels, with the appearance of moderate intoxication, chilling and sweating, attention is drawn to a significant increase in the lymph nodes of the posterior cervical group.
They increase in a chain along the posterior edge of the sternocleidomastoid muscle, as well as in the area of the mastoid process of the temporal bone. Despite the significant enlargement of this group of lymph nodes, which can even change the configuration of the neck, making it thicker, significant pain is usually not felt. Only during palpation, as well as in the case of intense head rotation, do children and adults feel slight pain in the neck.
In some cases, the lymph nodes do not enlarge at all, or their size changes only slightly; this clinical picture often occurs in adults and therefore may go unnoticed. In this case, the lymph nodes do not cause redness of the skin. No symptoms of suppuration or local inflammation can be detected. Other groups of lymph nodes, for example, submandibular and cervical, increase less significantly.
Sometimes a sore throat develops, which is a form of infectious mononucleosis, and various changes often occur in the nasopharynx, and therefore patients have difficulty breathing through their noses and prefer to breathe through their mouths, although upon examination the nasal passages are not clogged with mucus and there is no discharge from the nose. Experienced doctors call this condition “dry nasopharynx.”
Prognosis and possible complications
Mononucleosis has a favorable prognosis - with timely, competent treatment, in almost 100% of cases, complete recovery occurs within a few months. Complications are rare. Early consequences include:
- Splenic rupture. Occurs when the organ is greatly enlarged. Accompanied by internal bleeding and requires immediate surgical intervention.
- Asphyxia. It is observed when the airways are blocked by swollen tonsils.
- Nervous system disorders (meningitis, encephalitis).
- Attachment of a bacterial infection - sore throat caused by streptococcus, bronchitis, sinusitis.
- Lymphadenitis is an inflammatory disease of the lymph nodes.
Complications of mononucleosis may not appear immediately. We are talking about the late consequences of the disease. Against the background of the disease, hemoglobin drops significantly, resulting in anemia, which is observed for several months after recovery. The Epstein-Barr virus negatively affects the heart and can lead to the development of myocarditis - damage to the heart muscle. Jaundice sometimes develops due to liver damage. After suffering from mononucleosis, the pancreas may become inflamed.
Origin of cells
Cells have different functions
- T-killers (cytotoxic) - destroy altered cells of their own body, for example, during tumor transformation or infection with intracellular parasites;
- T helper cells - signal the detection of foreign proteins by other immune cells;
- T-suppressors - regulate the strength of the immune response.
B lymphocytes are formed and mature in the bone marrow, after which they enter the bloodstream and settle in the lymph nodes and spleen for further differentiation. After contact with a foreign protein, they are activated and begin to synthesize protective antibodies - immunoglobulins. B lymphocytes ensure the neutralization of pathogens and promote their elimination from the body.
A small portion of activated B lymphocytes circulate in the blood for years or for life – they are responsible for immune memory. Thanks to them, in the event of a second encounter with the same infection, the immune response develops many times faster than the first time. Thus, the disease does not develop at all or occurs in a mild form.
In response to the impact of foreign proteins on the immune system, lymphocytes are activated. This process is accompanied by an increase in the nucleus and the amount of cytoplasm, since they accommodate a large number of synthesized proteins.
Some viruses are capable of directly enhancing the synthetic activity of lymphocytes, which leads to the formation of atypical mononuclear cells. Such changes can be described as an extreme degree of activation of lymphocytes - they increase in size by 4-5 times. In a blood smear, atypical mononuclear cells appear as cells with a wide cytoplasm and a relatively small nucleus.