October 8, 2020 Admin Home page » Ultrasound of the pelvic organs Views: 3193
Gynecology and ultrasound have been “together” for quite a long time. This type of diagnosis has become an integral part of the examination for suspected diseases of the female reproductive system and more. Ultrasound is used during pregnancy and during preventive examinations (not always). It can also be done at your own request by making an appointment at a private clinic.
What are follicles, their role in the body
Folliculus are multilayered hollow formations surrounded by epithelium and connective tissue. They protect the site where the oocyte matures until ovulation, and also influence the synthesis of estrogen.
Follicles in the ovaries, the normal number of which is about 500 thousand, are formed at birth. They begin their growth during the girl’s puberty and go through certain development cycles. This is an ongoing process that ends during menopause. Most specimens die within a certain cycle as a result of atresia. The rest goes through all stages of evolution.
There are 3 stages of growth:
- small;
- big;
- active maturation.
Each element has one female reproductive cell and follicular cells.
Folliculometry
This procedure is actively used to control the formation and development of the egg. It is based on ultrasound, which is why medical experts today consider it the most accurate way to determine the time of ovulation.
Folliculometry allows you to record the size of the endometrium even before the moment when the ovulatory process begins, as well as the number of eggs and the “dimensions” of the dominant, if by the time of observation it is no longer noticeable.
For the first time, such a procedure is carried out on the 10th day of the cycle. Afterwards, every couple of days it is necessary to do repeated examinations until the cell is released or menstruation occurs.
Thanks to folliculometry, it is possible to determine a favorable day for fertilization naturally or for taking already mature cells for IVF. In addition, the procedure helps to discover what is preventing conception.
Types of follicles
In accordance with the stage of development, elements are divided into certain types:
| Primordial | This type includes immature elements that are located in the superficial parts of the ovary. They have a flat shape. They are located in large numbers, but the sizes are the smallest. |
| Primary, or preantral | This type includes awakened elements that have entered the maturation phase. They are larger than previous follicles and have a cubic shape. |
| Secondary or antral | Folliculus at this stage have a more mature form. They are multilayered, and cavities filled with liquid are formed between the layers. There is an additional thecal membrane, which appears before the cavities and is decisive in the identification of this element. |
| Tertiary, or preovulatory, or mature | Elements of this type reach maximum development and therefore have the largest size. Their cavities are filled with liquid and surrounded by a theca membrane. |
Stages of development by day of the cycle
The maturation of elements occurs continuously. During the growth stages, their active formation occurs.
Follicles in the ovaries, the normal number of which in girls reaches about 6 million, directly depend on the maturity and health of the parents. Reproduction of elements occurs during intrauterine development. During life, they are spent in the same quantity as they were formed earlier.
There are 3 stages of development. At the first preantral stage, follicles consist of a nucleus and epithelial cells. Before this they are in a state of rest. During puberty in girls, the elements move to the stage of small growth.
The elements are gradually covered with new layers and microscopic fluff. They become multi-layered and begin to secrete the female hormone estrogen. At this stage, capillaries and connective tissue are formed. The amount of liquid in the cavities begins to increase.
During this period, various diseases during childhood, stress, and anxiety can negatively affect the number of folliculus.
Some of the elements die, and some move to another stage - great growth. At this time, the egg accumulates nutrients, and a cavity with follicular fluid is formed. The cells begin to produce large amounts of estrogen.
The third stage is the shortest. The follicle begins to mature 12 hours before ovulation and disappears 2 days after fertilization. If the process is successful, cell division continues, and the maturation stage ends with the formation of a haploid set of chromosomes.
How to prepare for an ovarian ultrasound
In the absence of any adverse symptoms, the best time to conduct a routine study is the 5th-7th day of the cycle, which, as a rule, occurs at the end of menstrual bleeding. To get a complete picture, the ultrasound will have to be repeated three times: on days 8, 14 and 22. Be that as it may, studying the ovaries alone is not enough. It is possible to draw up a complete clinical picture only after examining the entire reproductive system, in particular by establishing the normal size of the uterus.
How is an ovarian ultrasound performed? The patient can choose one of three methods.
- Transabdominal. The lower abdomen is lubricated with a special gel, and then a wide sensor is moved. It must be said that this is not the most informative method, since it allows you to see only obvious pathologies.
- Transvaginal. This method is more modern and informative. With its help you can see all the changes that occur in the ovary. To do this, the ultrasound machine sensor is inserted directly into the vagina, but not too deep, so that the uterine os remains intact.
- Transrectal examination. It is carried out through the rectum. This is the only way to examine the pathology of the ovaries in virgins without damaging the hymen.
In order for the ultrasound picture to be as complete as possible, the patient needs to prepare for the procedure in a special way. Thus, before a transabdominal ultrasound, it is necessary to follow a three-day diet, limiting the consumption of foods that cause fermentation in the gastrointestinal tract. This is especially true for cabbage, beans, black bread and soda. It will not be superfluous to take sorbents - Espumisan, Sorbex, activated or white carbon. An hour before the scheduled time of the ultrasound, you need to drink a liter of water, but you will be able to urinate only after the procedure.
Vaginal ultrasound also involves taking sorbent drugs, but the bladder, on the contrary, must be empty. You need to prepare for a transrectal examination even more carefully, getting rid of not only urine, but also feces. 12 hours before the ultrasound you will have to do an enema or use modern laxatives - Guttalax, Senade. Microkisms in the form of rectal suppositories (Norgalax) are suitable.
It happens that none of the above methods manage to see the ovary on the ultrasound machine screen. This can be prevented by severe bloating or severe pelvic adhesive disease. Another reason is the organ’s too small size, which indicates its premature depletion. It may also happen that the ovary will not be in the right place at all - it may be absent due to a congenital pathology or a surgical intervention. In any case, it is too early to draw any conclusions after one failed research attempt. Most likely, you will have to take a course of sorbents and visit the ultrasound room again.
The role of the dominant follicle
Selection of the dominant follicle occurs in the third developmental cycle. The element size is approximately 20 mm. It develops normally if the body is healthy and there are no pathologies.
In the fluid that fills the follicular antrum, the estrogen content increases sharply. A rise in its level causes the release of luteinizing hormone and ovulation. When the wall of the dominant follicle ruptures and the egg is released, the process of reduction division is restored.
Why doesn't the gap occur?
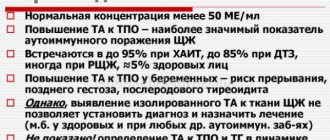
The vesicle may not rupture due to hormonal imbalance. Most often, in this case, folliculogenesis is practically not impaired. The membrane for the release of the egg does not burst if the size of the vesicle is small or the level of the following hormones is disturbed:
- estradiol;
- luteinizing;
- follicle-stimulating;
- 17-OH-progesterone;
- prolactin.
The pouch is able not to rupture during inflammatory and infectious processes in the genital organs.
The normal course of ovulation is restored after adjusting the woman’s hormonal levels.
Normal number of follicles in the epididymis by age
Follicles in the ovaries, the normal number of which serves to determine the morphological criteria for age, depend on the hormonal activity of the body. An important argument evaluating the reproductive system is age. The main patterns of follicle development depend on the hormonal regulation of body functions.
Starting from adolescence, under the influence of hormones from the anterior pituitary gland, cyclical changes occur in the ovaries in girls. The endocrine system controls each folliculus.
The genetically determined stock of folliculus by age is:
- at the moment of birth there are 2 million immature elements;
- 11 thousand pieces are lost every month;
- by the time of puberty, 300–400 thousand remain;
- Before the onset of age-related menopause, 1000 pieces are lost. monthly;
- By the age of 47-50, the ovarian reserve is depleted.
As a result, by the age of 45, a woman has a low probability of conceiving, despite the fact that menstrual cycles and hormonal activity of the ovaries persist.
Normal number of follicles during pregnancy
The follicles located in the ovaries have their own norm, which is an assessment of the upcoming superovulation during fertilization.
Their number is interpreted as follows:
- less than 5 – infertility;
- 5-7 – low probability of fertility;
- 8-15 – pregnancy is possible;
- 16-30 – normal;
- more than 30 – polyendocrine syndrome, accompanied by impaired ovarian function.
During pregnancy, the female body is not completely freed from the folliculus. Only those that have awakened with a dominant follicle are destroyed. The rest are dormant and awaken after the birth of the child.
Normal number of follicles during menopause, menopause
With the onset of menopause, changes occur in the functioning of the genital organs and hormonal imbalance. Follicles in the ovaries, the number of which is limited, change sharply and shrink during menopause. It is their absence that determines the decrease in estrogen levels. As the number of periods decreases, the folliculus also decreases.
The norm of follicles in the ovaries during menopause changes along with the level of hormones
During menopause, the elements significantly complicate the course of the last independent menstruation. During this period, the ovaries decrease in size and are susceptible to various diseases. If they begin to increase, then this may be caused by the development of a cyst, polycystic disease, or malignant tumor.
It is important to visit a gynecologist once every six months during this period in order to diagnose the disease in time.
How do follicle sizes normally change during the cycle?
At the beginning of each menstrual cycle, under the influence of follicle-stimulating hormone, new folliculi begin to develop in the ovaries.
The process of folliculogenesis with a standard cycle of 28 days occurs as follows:
- at the age of 5 days, the size of the antral follicles is up to 5 mm;
- by day 7 they increase at a rate of 1 mm per day;
- on day 8, a dominant is selected. It continues to grow at a rate of 2 mm per day and reaches sizes of up to 15 mm. The remaining folliculi regress and disappear;
- The ovulatory phase occurs on day 14. The dominant follicle reaches a size of 24 mm, then it bursts and an egg is released from it.
The average lifespan of an oocyte is from 12 to 24 hours.
What is folliculometry and why is it performed?
The technique monitors the growth and development of the folliculus in the ovaries and helps determine the possibility of conception. Ultrasound examination is recommended to be performed from the eighth to tenth day of the menstrual cycle. On the eighth day, the dominant follicle will be noticeable.
An ultrasound examination is performed to obtain the following information:
- assessment of the condition of the uterus and ovaries, their correspondence to the phase of the cycle;
- study of the functioning of the ovaries;
- obtaining confirmation of ovulation;
- determining the time when the oocyte leaves the follicle;
- identifying the causes of menstrual irregularities and ovarian dysfunction;
- elucidation of factors influencing the absence of ovulation during menstruation;
- assessment of cyclic changes in the endometrium and identification of possible pathologies;
- establishing the usefulness of the luteal phase of the menstrual cycle, based on the information obtained about the corpus luteum;
- control over the process of egg maturation during hormonal therapy.
Repeated folliculometry is carried out subject to the presence of an ultrasound of the pelvic organs, completed no later than 6 months ago.
A repeat series of ultrasound examinations is carried out in order to:
- establish the fact of ovulation;
- determine the phases of the menstrual cycle;
- find out the day the egg is released;
- perform in vitro fertilization;
- diagnose infertility;
- control the effect of hormonal drugs on the ovaries.
When performing folliculometry, attention is paid to the maturation of follicles and the endometrium.
Disorders due to improper development of the dominant follicle
If the development of the dominant folliculus is disrupted, ovulation does not occur, since the oocyte cannot come out. In such cases, observation and ultrasound are performed. Starting from the 10th day of the cycle, the growth of the dominant folliculus is monitored. If it matures slowly, the egg cannot be released from the ovary. In this case, treatment is prescribed. During the next cycle, observe the result.
Violations in the development of the dominant element can occur for various reasons:
- early onset menopause, resulting from surgery or naturally;
- pathology of ovarian function;
- problems with ovulation;
- lack of estrogen;
- disorders of the endocrine glands;
- infections of female genital organs;
- pituitary adenoma.
Pathology in the maturation of the dominant is caused by depression, stress, and nervous tension.
If there is a Graafian blister, when will ovulation occur?
The presence of a Graafian vesicle implies that ovulation will occur soon, but in clinical practice this does not always happen.
If there are endocrine disorders, insufficient or excessive production of the FSH hormone, then ovulation may not occur, and the “graaf bubble” will not burst.
In this case, the following ultrasound picture is possible:
- Follicular cyst.
- Follicle regression.
- Persistence.
- Luteinization.
Detection of a “Graafian vesicle” does not mean that ovulation will occur with 100% probability. In most cases, this happens, and especially when it has reached its maximum size, but no one has canceled the endocrine mechanisms of a pathological nature.
IMPORTANT! If the dominant follicle has reached a size greater than 24 mm, then it is permissible to talk about the presence of a cyst. In this case, ovulation will not occur.
Possible deviations
Follicles in the ovaries, the number of which may be exceeded or underestimated, may stop growing or developing to the desired size. In this case, the woman does not ovulate. The cause of deviations is detected using ultrasound and determining the level of sex hormones in a woman.
Persistence
The pathology is caused by an imbalance of hormones, which is necessary for the regulation of the menstrual cycle.
Persistence can be recognized by the following symptoms:
- low level of progesterone in the blood;
- increased estrogen levels;
- the dominant follicle exists for a long time;
- there is no luteal phase of the menstrual cycle;
- there is no corpus luteum and fluid in the retrouterine space.
Therapy is aimed at normalizing hormonal levels. Doctors prescribe medications that reduce estrogen levels in the follicular phase and increase progesterone levels in the luteal phase of the menstrual cycle.
Exceeding the size norm
Excessive enlargement of the follicle may indicate a cyst. The formation is a cavity filled with fluid, sometimes with blood or pus. In this case, the diameter of the folliculus exceeds the norm and becomes more than 30 mm. In this case, it is necessary to puncture and suction the follicles.
The pathology causes disruptions in the menstrual cycle and painful symptoms in the lower abdomen.
Absence
Temporary absence of folliculus is mainly associated with the psychological state of the woman. As soon as the body is restored, the elements are formed again.
Failures can be caused by the following factors:
- incorrectly selected contraceptives;
- endocrine diseases;
- a sharp change in weight up or down.
The disappearance of the folliculus over the age of 45 is a natural process, as menopause occurs.
Regulating the process of follicle maturation
The main goal of therapy is to restore the normal menstrual cycle and relieve the woman of infertility. You can achieve results by stimulating ovulation, reducing or increasing the number of antral follicles.
Stimulation of ovulation
Stimulation of ovulation is carried out after undergoing comprehensive diagnostics aimed at identifying the causes of pathologies in the menstrual cycle. Antiestrogenic agents are prescribed to stimulate the production of estradiol and follicular growth.
Cyst prevention is carried out using injections of hormonal drugs Praegninum or Gonakor. Stimulation is not carried out if the ovarian reserve is depleted during menopause and if the fallopian tubes are obstructed.
Decreased number of antral follicles
If the folliculus content is increased, therapy is aimed at normalizing the hormonal balance. You can regulate the production of follicle-stimulating and luteinizing hormone, estrogens, prolactin and progesterone using combined oral contraceptives.
Depending on the pathology, medications are prescribed:
- Duphaston;
- Estradiol E2;
- Angelique®;
- Clomiphene;
- Klimonorm®.
Combined hormonal drugs are used to treat menstrual irregularities, reduce or eliminate ovulatory syndrome.
Is it possible and how to increase the number of antral follicles?
The production of anti-Mullerian hormone affects the number of folliculus. With the help of a vitamin complex, as well as preparations containing biologically active substances, it is possible to increase the stimulation of ovarian functions and increase the chances of successful maturation of eggs.
But it is impossible to enhance the production of the hormone with medications, since the number of folliculus depends on the genetic characteristics of the body and the age of the woman.
The oocyte develops inside the follicles in the ovaries. Changes in hormonal levels and the possibility of conception depend on the norm of their quantity. Deviations from the norm may result in a risk of various pathologies. There may be several reasons for violations, so it is important to undergo a qualified examination to avoid infertility.
Article design: Mila Friedan
Treatment
Very often, the condition in which small follicles are diagnosed recovers on its own after 1-2 cycles.
If recovery does not occur, treatment is prescribed. Treatment for this condition depends on the causes that caused it. If a woman has been taking contraceptives, they should be discontinued. If it turns out that the cause of the pathology is systemic diseases, therapy for the underlying pathology is necessary.
The basis of drug treatment is the use of hormonal drugs. In some cases, the doctor may recommend surgery - cauterization of the ovaries (removal of underdeveloped structures). With timely treatment of the pathology, ovarian function is completely restored.