What is pulmonary infiltrate?
With a pulmonary infiltrate, healthy tissue is replaced by a pathological formation filled with fluid, chemicals or some kind of cells. This formation is large and dense. By the way, there can be either one or a whole set of seals. And in inflammatory processes, lobar damage to the lungs by infiltration formations is generally characteristic.
As a rule, infiltration is caused by various inflammatory processes, which are divided into several types: hemorrhagic, leukocyte, lymphocytic, eosinophilic.
Features of the problem
First of all, in addition to a general idea of what an abscess in the lung is, you should also know what this disease is like. In medicine, it is customary to conventionally divide this phenomenon into forms. In this case, we mean classification according to the causes of the abscess, its location in the lung, the severity of decay and the timing of development.
So, if we highlight the causes of an abscess, in addition to those already mentioned earlier, doctors usually identify two separate factors:
- Primary – we are talking specifically about the factor of physical damage to the organ (bruises, injuries, ruptures, etc.), subsequently which results in fibrosis and suppuration. At the same time, we are talking not only about the severity of the damage and the occurrence of problems during healing; if the wound is serious, bacteria and microorganisms from the outside are attached, which can cause the formation of an abscess.
- Secondary - often implies the presence of some deviation and problem of the respiratory channels of the lung. This may be the previously mentioned pneumonia (pneumonia), blockage of the bronchi due to the formation of tumors, as well as blockage of the channels due to foreign objects.
If we raise the issue of positioning, there are also only two factors: abscesses are divided into central and peripheral. Everything is quite simple here, in the first case we are talking about formation closer to the central regions of the organ, in the second we mean the appearance of a lesion on the periphery of the organ, that is, on the edge.
As for the degrees of severity, everything is quite individual and depends on many factors. But when observing and making a diagnosis, for which the doctor must examine the lung abscess on an x-ray, three stages of the disease can be distinguished:
- Mild – symptoms and accompanying problems are mild, the person feels bad, but not critical.
- Medium – symptoms make themselves felt more clearly, there are more of them, and the disease becomes more acute.
- Severe – there is a critical manifestation of symptoms, serious consequences and associated complications are possible.
The last thing I would like to talk about in terms of the characteristics and classification of the problem under discussion is the timing of development. Here again there are two points with different predictions:
- Acute abscess - no more than 6 weeks pass from the beginning of the formation of the lesion to getting rid of it with healing and scarring of the tissue, while the prognosis is favorable and everything ends with the patient’s recovery, as well as relief from most of the symptoms.
- Chronic - the course of the disease can significantly exceed the period established above, while the disease transitions from states of exacerbation to remission and back.
As you can see, the classification of this disease is quite extensive, but is not particularly severe, that is, making a diagnosis from an experienced specialist should not cause problems. However, to understand the situation and respond correctly, you need to know about the symptoms of this disease, diagnostic methods and risk factors.
Types of infiltrates in the lungs
In modern medicine, the types of infiltration are classified depending on the contents of the detected compactions. There are chemical, inflammatory and tumor forms.
In the chemical form, the appearance of infiltrates is most often a consequence of surgery in the lung area. Or compactions may appear as a result of the introduction of chemicals into the lung tissue.
Inflammatory infiltrate syndrome in the lungs appears as a consequence of an infection. In this case, leukocytes, erythrocytes, lymphoid and other cells can be found inside the seal. With timely medical care, such formations, as a rule, resolve on their own. However, in some cases they can grow.
With tumor infiltration, the compaction contains malignant cells. Such formations grow abnormally quickly. And in this case, the prognosis for the patient may be disappointing.
It is important to remember that the presence of infiltrates means that the lungs will not be fully used when breathing. And if such neoplasms occupy a large area, then there is a serious danger to the patient’s life.
Causes
Factors causing infiltration include:
- Pneumonia. With pneumonia, infiltration manifests itself acutely. It is caused by pathogens that attack organ tissue. The respiratory part of the lungs is involved in the process. The phenomenon occurs against the background of acute respiratory infections and influenza. The patient's temperature rises and sputum is produced when coughing. In severe cases of the disease, respiratory failure occurs.
- With eozonophilic infiltrate, the cause is associated with a disorder of the immune system. Signs of the disease are similar to those of pneumonia. Corticosteroids help improve the patient's condition.
- Infiltrative tuberculosis . The pathological process develops gradually. The patient has a temperature of 37.5 degrees for a long time and a slight cough. The X-ray image shows places of calcification, a path to the root, and damage to the upper lobe.
- In case of cancer, neoplasms, metastases, and a prolonged cough are detected, in which sputum is released in minute quantities. The images show darkening and places where tumors have disintegrated. Metastases appear in the form of numerous shadows.
- If a benign formation has developed, the outlines of the shadows are clear, there are no tracks, nearby tissues are unchanged.
- Foci of pneumosclerosis.
- Pyogenic diseases - abscess, gangrene.
Pulmonary infarction rarely leads to infiltration. It occurs against the background of: thromboembolism, hemosiderosis, hemosiderosis, echinococcosis, sarcoidosis. In this case, patients exhibit the following symptoms:
- shortness of breath;
- cough (wet or dry);
- pain that appears when breathing (the symptom occurs if the pleura is damaged).
The doctor conducting the examination notices that one half of the chest lags behind during breathing. The patient hears moist rales and characteristic crunching sounds.
The strength of symptoms depends on the size of the infiltrate, the reasons for its development and the location of the lesions. With tumor formations or impaired bronchial drainage system, the respiratory process is slightly weakened, other signs are not detected.
Clinical manifestations
Infiltrates can appear in just a few days. The appearance of such formations is accompanied by quite pronounced symptoms, such as:
- Pain in the lung area;
- Low-grade body temperature (from 37.1 to 38), which lasts for a long period;
- Unnatural paleness of the skin;
- Sometimes you can visually notice swelling at the location of the compaction;
- If there is a cough, then there is blood in the sputum (this means that the infiltrate is decomposing).
Pain in the lung area is a possible symptom of infiltration in the lungs.
The described set of symptoms is similar to those that occur with pneumonia, so a number of additional measures will be required to clarify the diagnosis.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Weight loss (emaciation, weight loss, thinness, weight loss, weight loss) | 90% |
| General weakness (fatigue, tiredness, weakness of the body) | 80% |
| Chest pain when breathing and coughing (chest pain) | 50% |
| General increase in body temperature (fever, fever) | 50% |
| Night sweats | 40% |
| Coughing up blood (blood in sputum) | 30% |
| Dry cough in the morning | 30% |
| Cough that gets worse at night | 20% |
| Constant or periodic shortness of breath without connection with body position or stress | 15% |
Peculiarities of manifestation in various diseases
Infiltration most often occurs as a result of various diseases. And sometimes, by characteristic signs, it is possible to determine which particular illness caused this phenomenon.
Pneumonia
It occurs due to infection in the lungs, usually due to a cold or flu. Seals appear quite quickly. In this case, the occurrence of infiltrates is accompanied by a strong wet cough and fever. In severe cases, respiratory failure may develop.
Tuberculosis
The patient suffers from a slight cough and a slightly elevated temperature (up to 37.5). The process of formation of infiltrates proceeds quite slowly. An x-ray can show calcifications in the upper part of the lungs.
Malignant tumor
If there are malignant cells inside the resulting infiltrate, then on an x-ray it will look like a shadow. In the same image, you can see foci of the tumor and even metastases, if they have already appeared. The patient in this situation has a prolonged cough, during which little sputum is coughed up.
What to do if you suspect a disease
PCR diagnostics of infections
A positive result of PCR diagnostics for the presence of the causative agent of tuberculosis with a high degree of accuracy indicates the presence of this infection.
Blood chemistry
In tuberculosis, increased levels of C-reactive protein may occur.
Biochemical examination of urine
Tuberculosis is characterized by a decrease in the concentration of phosphorus in the urine.
Analysis for CEA
In tuberculosis, the level of CEA (carcinoembryonic antigen) is increased (70%).
General blood analysis
In tuberculosis, the number of platelets (Plt) is increased (thrombocytosis), relative lymphocytosis (Lymph) (more than 35%), monocytosis (Mono) is more than 0.8 × 109 /l.
Fluorography
The location of focal shadows (foci) in the image (shadows up to 1 cm in size) in the upper parts of the lungs, the presence of calcifications (round-shaped shadows, comparable in density to bone tissue) is typical for tuberculosis. If there are a lot of calcifications, then it is likely that the person had fairly close contact with a patient with tuberculosis, but the disease did not develop. Signs of fibrosis and pleuroapical layers in the image may indicate previous tuberculosis.
General sputum analysis
During a tuberculous process in the lung, accompanied by tissue disintegration, especially in the presence of a cavity communicating with the bronchus, a lot of sputum can be released. Bloody sputum, consisting of almost pure blood, is most often observed with pulmonary tuberculosis. In pulmonary tuberculosis with cheesy disintegration, the sputum is rusty or brown in color. Fibrinous clots consisting of mucus and fibrin may be detected in the sputum; rice-shaped bodies (lentils, Koch lenses); eosinophils; elastic fibers; Kurschmann spirals. An increase in the content of lymphocytes in sputum is possible with pulmonary tuberculosis. Determination of protein in sputum can be helpful in the differential diagnosis between chronic bronchitis and tuberculosis: with chronic bronchitis, traces of protein are determined in the sputum, while with pulmonary tuberculosis in the sputum the protein content is higher and can be determined quantitatively (up to 100-120 g /l).
Rheumatoid factor test
The rheumatoid factor level is higher than normal.
Diagnostics
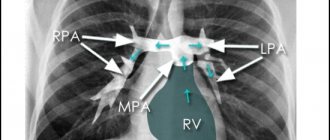
The main way to detect infiltrates is x-ray examination. In this case, the compactions in the image will be darkened areas, the size of which exceeds 1 cm. The outlines of these areas depend on the form of infiltration and the localization of the compactions themselves.
In pneumonia, the seals in the image have an irregular shape and unclear contours. In a chronic inflammatory process, the contours are clear, but the shape is jagged. In the case when the appearance of compactions is caused by pathogenic microorganisms. Then one can observe necrosis of lung tissue.
X-ray is one of the methods for diagnosing infiltrates in the lungs
In the diagnostic process, it is important to determine not only the presence of infiltrates themselves, but also the reason for their appearance. X-rays also help partly with this. So, for example, if a whole lobe of the lung is affected by compactions, then this is most likely a consequence of pneumonia or tuberculosis, and if not, then differential diagnosis is required to make sure that the resulting formation does not contain malignant cells.
A specialist can often suspect the presence of a malignant tumor based on an x-ray. Since in this case the seals will have regular shapes and clear contours.
By the way, with a malignant tumor, at the initial stage of its development, infiltrates can only be detected by chance during a routine preventive examination, since the patient does not complain about anything. There are no symptoms of the disease at this time.
Signs of infiltration in the lungs according to X-ray examination
Infiltration is characterized by a moderate increase in lung tissue and its increased density. It is for this reason that radiological signs of infiltration in the lungs have their own characteristics.
With infiltration in the lungs of the inflammatory type, uneven outlines and irregular shapes of darkening are observed. During the acute stage of infiltration in the lungs, blurred outlines are observed, gradually turning into the tissue that surrounds the lungs. With chronic inflammation, the contours are jagged and uneven, but more clearly expressed. With the inflammatory form of infiltration in the lungs, you can often see branching light stripes - these are the bronchi filled with air.
Due to the fact that the pathogen causes damage to the respiratory organs in a number of inflammatory diseases, tissue necrosis of varying degrees can be observed, which, in turn, significantly increases the severity of the disease.
In order to prevent the development of necrosis and restore the integrity of bronchial and pulmonary tissue, the following type of treatment can be recommended: marsh cudweed, medicinal sweet clover, yarrow, birch leaves and buds, aloe and medicinal medicine.
Treatment
During treatment, patients are often advised to remain in bed until complete recovery, since even minor physical activity during this period can be detrimental to the body. It is also very important to monitor your diet. Food should contain the entire necessary set of microelements and be easily digestible.
Medication
Most often, infiltrates are treated by prescribing a complex regimen of antibiotics from various groups. The necessary medications should be prescribed by a specialist, since after carrying out all the necessary diagnostic measures, he will know exactly which set of drugs is optimal for each specific case, as well as which drugs can and cannot be combined within the same course of therapy. For example, the simultaneous use of bactericidal and bacteriostatic drugs can lead to irreversible consequences and create a serious danger to the patient's life. As a rule, taking one antibiotic lasts no longer than 10 days.
In addition, depending on the type of pathogen identified, mucolytic, expectorant, diuretic and antiviral drugs may be prescribed. Diuretics help relieve swelling, and in combination with mucolytics they significantly facilitate expectoration. Antiviral drugs are often prescribed in combination with antibiotics.
Traditional methods
Treatment with traditional medicine can be another addition to complex therapy to combat infiltrates. However, using folk remedies on your own, without consulting a specialist, is not recommended. In addition, it is important to consider that traditional medicine alone cannot cure infiltrates. Below are several folk recipes that can be used to complement medical treatment.
Garlic
The most popular folk method is inhaling garlic vapors. To prepare the required mixture, several cloves of garlic are peeled and grated, all this is poured into a jar and the resulting mixture is inhaled for 5 - 10 minutes. This is done several times a day; during the procedure, it is important to breathe through the nose and mouth alternately.
Garlic inhalation - a folk method of treatment
Immune-boosting mixture
Take 5 large aloe leaves and put them in the refrigerator for 4 days. Then grind in a meat grinder with one lemon and add a glass of honey. Mix everything and drink a teaspoon three times a day.
Onions with milk
Take and finely chop two medium onions, then mix them with a glass of hot milk and boil for 5 minutes over low heat. Then let it brew for 4 hours and you can drink. You should take a spoonful of the decoction every three hours. The remedy is effective in the first few days of illness.
Honey with plantain
Take dried plantain leaves, which were collected in May, crush them and put a not too thick layer on the bottom of a glass jar, then pour a layer of honey over it all. Thus, the selected container is filled to the top, closed with a lid and buried approximately 70 cm into the ground. After 3 months, the composition is dug out, filtered through cheesecloth, boiled for half an hour in a water bath and bottled. The mixture should be taken a short period of time before meals, one tablespoon (for children, one teaspoon). The finished composition must be stored in the refrigerator.
Treatment of pulmonary tuberculosis (infiltrative and focal)
Tuberculosis must be treated in a specialized medical institution. Treatment is carried out with special first-line tuberculostatic drugs. Therapy ends only after complete regression of infiltrative changes in the lungs; this usually requires at least nine months, or even several years. Further anti-relapse treatment with appropriate drugs can be carried out under clinical observation conditions. In the absence of a long-term effect, the persistence of destructive changes, the formation of foci in the lungs, collapse therapy (artificial pneumothorax) or surgical intervention are sometimes possible.
Essential drugs
There are contraindications. Specialist consultation is required.
- Isoniazid (Tubazid) is an antituberculosis, antibacterial, bactericidal agent. Dosage regimen: the average daily dose for an adult is 0.6-0.9 g, it is the main anti-tuberculosis drug. The drug is produced in the form of tablets, powder for the preparation of sterile solutions and a ready-made 10% solution in ampoules. Isoniazid is used throughout the entire treatment period. If the drug is intolerant, ftivazid is prescribed, a chemotherapy drug from the same group.
- Rifampicin (semisynthetic broad-spectrum antibiotic). Dosage regimen: taken orally, on an empty stomach, 30 minutes before meals. The daily dose for an adult is 600 mg. For the treatment of tuberculosis, it is combined with one anti-tuberculosis drug (isoniazid, pyrazinamide, ethambutol, streptomycin).
- Streptomycin (a broad-spectrum antibiotic used in the treatment of tuberculosis). Dosage regimen: the drug is used in a daily dose of 1 ml at the beginning of treatment for 2-3 months. or more daily or 2 times a week intramuscularly or in the form of aerosols. When treating tuberculosis, the daily dose is administered in 1 dose, in case of poor tolerance - in 2 doses, the duration of treatment is 3 months. and more. Intratracheal, adults - 0.5-1 g 2-3 times a week.
- Ethambutol (anti-tuberculosis bacteriostatic antibiotic). Dosage regimen: taken orally, 1 time per day (after breakfast). It is prescribed in a daily dose of 25 mg per 1 kg of body weight. It is used orally daily or 2 times a week in the second stage of treatment.
- Ethionamide (synthetic anti-tuberculosis drug). Dosage regimen: prescribed orally 30 minutes after meals, 0.25 g 3 times a day, if the drug is well tolerated and body weight is more than 60 kg - 0.25 g 4 times a day. The drug is used daily.
Complications
Among the most serious complications arising from pulmonary infiltration is the development of respiratory failure, which over time will lead to oxygen starvation, and then to irreversible changes in internal tissues and organs. Therefore, this disease requires timely effective medical therapy.
In addition, infiltration can contribute to the appearance of diseases such as pneumosclerosis, atelectasis, as well as the appearance of irreversible changes in the organs of the respiratory system. In some cases, sclerotic areas form at the site of resolved infiltrates.
The need for an x-ray after opening the formation
You already know how important it is to take radiography to make a diagnosis and prescribe treatment, but there is another important factor - you can, and in some situations even need to look at the image after drainage of the abscess; in radiology, this phenomenon will be referred to as a cleared abscess or a sign of a false cyst .
So, after hiding the capsule, the process of expectoration and the complete discharge of purulent contents, the following picture is observed in the photographs:
- The walls of the annular body are thinned;
- No liquid level, even minimal, should be visible;
- There is a gradual overgrowth of the abscess area with connective tissue, due to which the formation retains its size and shape for some time, but then turns into a scar.
If the recovery goes well and no complications are observed, all signs of the disease disappear within about one month, breathing returns to normal, the cough should completely go away, and the person’s general condition returns to normal.
Differential diagnosis of formations of the upper mediastinum
In addition to goiters, bronchogenic cysts can also be found in the upper mediastinum (more than half of all bronchogenic cysts are localized in the upper mediastinum), as well as tumors of nervous tissue (neurinomas and neurosarcomas), pleural tumors (mesothelioma) and tumors of the lymph nodes.
Thus, a smooth transition of the contour of the shadow of a parietal formation near the shadow of the spine may be characteristic of a neurogenic tumor. If the shadow is adjacent to the inner surface of the chest wall, one may suspect mesothelioma, a tumor of the soft tissues of the chest wall, or (less commonly) a neuroma of the intercostal nerves.
CT. A formation of the upper mediastinum was detected, located partially behind the manubrium of the sternum, adjacent to the wall of the trachea anteriorly and laterally, with no signs of invasive growth. It is clear that the formation is not associated with the thyroid gland (it is located separately from it and is separated by a “strip” of adipose tissue)
Computed tomography of the mediastinum in the patient revealed an enlargement of the left lobe of the thyroid gland due to goitrous transformation (the enlarged lobe is marked with arrows in the images)
It is carried out using multi-axial fluoroscopy and radiography, contrasting of the esophagus, tomography (linear and computer), pneumomediastinum, diagnostic pneumothorax, angiography, ultrasonography.