In our country, the method of magnetic resonance imaging, or MRI, appeared not so long ago, but has already become a favorite among both doctors and patients. Its main feature is absolute safety. Previously, it was possible to find out whether there were pathologies in the human body only with the help of X-ray examination. But radiography has a large number of contraindications; in addition, this method does not always show the most reliable picture. An MRI is a completely different matter. The diagnosis is much more reliable and harmless - so much so that it can be used to examine both infants and women expecting a child.
Is it advisable and safe to perform an MRI while pregnant?
The period of a woman’s life that she devotes to bearing a child does not always proceed calmly and without any diseases that appear during pregnancy or worsen. When the doctor sees the prerequisites for a serious pathology that threatens the life of the expectant mother and her child, he may prescribe magnetic resonance imaging (MRI). But making such a decision must be balanced and careful, since such diagnostics have their own contraindications for pregnant women.
MRI of blood vessels in a pregnant woman
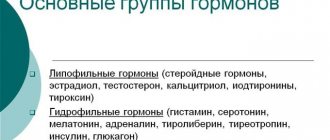
The concept includes:
- MRA of the brain.
- MRA of neck vessels.
Indications for vascular MRI during pregnancy
- Headaches, fainting, tinnitus, dizziness, decreased hearing or vision.
- Anomalies in the development or course of blood vessels.
- Injuries in the head or neck area.
- Vascular diseases, tumors, thrombosis.
The study does not require preliminary preparation. Diagnostics of each zone lasts about 20 minutes.
Can it be done during pregnancy at the beginning and end of pregnancy?
Carrying out an MRI in the early stages of gestation can have its own negative impact on the baby.
The operation of the tomograph is accompanied by emissions of a certain amount of thermal energy and noise. The first three months of the formation of all structures of the future newborn are extremely important, and such external influence can lead to an imbalance in the formation of organs and systems, and to the future appearance of serious malformations or anomalies.
The second and third trimesters are less susceptible to tomography, and therefore are considered more favorable for diagnostic measures. At this time, the main aspect of a successful and safe examination is the absence of contraindications on the part of the expectant mother.
Since the most important stages of development are associated with the first trimester of gestation, the second and third are considered more favorable for tomography, although they are associated with some risks.
Experts believe that the best option is to perform tomography during pregnancy planning. This will not affect the expectant mother's reproductive system and will help avoid many of the risks associated with MRI during pregnancy.
Is magnetic resonance imaging harmful for pregnant women?
The most accurate and safe way to diagnose changes in soft and cartilaginous tissues today is MRI. This procedure allows you to “enlighten” the unhealthy organ, identify all existing anomalies and make the correct diagnosis as accurately as possible. Therefore, in some cases, MRI during pregnancy simply does not have alternative options - it is prescribed if other diagnostic methods (ultrasound, tests, etc.) are impossible or uninformative.
Despite the fact that additional impact on the body of the expectant mother during such a delicate period is extremely undesirable, sometimes MRI is the most optimal solution, since this study allows you to more carefully monitor the condition of the fetus or diagnose the development of the disease in the patient herself. In addition, the procedure has virtually no negative effect on the body, therefore it is considered safe, including during pregnancy.
What are the special features for pregnant women?
MR imaging is associated with a number of features. They play an important role for expectant mothers carrying a baby:
- A fear of enclosed spaces may develop due to a specific restructuring of the mental state.
- The noise produced by the device causes discomfort even in ordinary patients, and in an expectant mother it can cause panic.
- The procedure is often performed with the use of a contrast agent, which is associated with additional risks and the possible presence of allergies.
- The diagnostic procedure must be agreed upon with a specialist, taking into account the baby’s activity schedule, so that the moment is most appropriate and does not cause stress for him.
- It is preferable to carry out diagnostics in an open-type apparatus, which is associated with changes in the woman’s body, in particular with an enlarged abdomen.
How to carry out the procedure
The expectant mother is invited to an MRI at the beginning of the day; both the woman and the fetus are usually calm at this time, which is important for obtaining high-quality images. It’s better to go “small” in advance; Problems will arise if you want to go to the toilet during a procedure that cannot be interrupted.
Before entering the tomograph tunnel, at the doctor’s request, you will have to remove your mobile phone, keys or bank cards from your pockets; remove watches from your hands, as well as clothes with metal parts - zippers, buttons. Get rid of metal jewelry.
Decorative cosmetics can also harm research; Powder, mascara and eye shadow sometimes contain metal salts. When going for an MRI, avoid wearing layers of makeup, otherwise the procedure will be wasted.
Here are some features of an MRI of a pregnant woman:
- a woman lies down on a couch along the tomograph tube with her feet forward - this position reduces the risk of claustrophobia; the doctor specifies the area of study where the magnetic field will later be generated;
A woman is placed in the tomograph tunnel with her head towards the exit - this reduces the risk of fear of closed spaces - the doctor is obliged to warn the patient that the procedure will stop immediately if the woman so desires; such a statement has a calming effect, especially since it is possible to sound an alarm while in the tomograph;
- During the procedure you cannot toss and turn or change positions; immobility is the main condition for obtaining an accurate image;
- towards the end of gestation, due to the increased mass of the fetus, lying on your back is uncomfortable, and breathing is difficult; the pregnant woman is allowed to turn on her left side - this will not spoil the “picture”;
- Before the scan, the woman is left in the tomograph for some time so that the baby in the womb calms down after the mother.
During the MRI, the patient does not experience any discomfort or pain. However, there is still one inconvenience: when working, the tomograph makes a lot of noise. Knowing this, bring headphones or earplugs to the procedure. However, clinics with a high level of service provide such devices, and even free of charge.
Is it worth doing an MRI partially during pregnancy: is it harmful to the fetus?
Having a complete picture of the condition of the expectant mother and knowing the timing of gestation, the specialist makes a conclusion about the need for tomography.
Heads
An examination of the expectant mother's head may be aimed at diagnosing:
- Severe pain, without a clear idea of its etiology.
- Suffered trauma.
- Causes of frequent fainting and dizziness.
- Appearing memory and thinking disorders, sudden decrease in intellectual abilities.
- Developed seizures.
- There is a suspicion of the development of encephalomyelitis, vasculitis or stroke.
- Conditions of the vascular system, regarding which the woman’s history contains information about chronic or recently developed pathologies.
- Deviations in the functional ability of the visual organs.
- Existing sinusitis, sinus abnormalities, or a sudden change in sense of smell.
- Present thyroiditis or other pathologies of the thyroid gland.
This method is also relevant in cases where an ultrasound examination of the head cannot be performed or its results need to be confirmed. The whole procedure is quite simple and takes from 15 to 30 minutes.
Spine
An MRI scan of the spine of a woman carrying a child can be performed to determine:
- Causes of disorders in the blood circulation of the spinal cord.
- The presence of malformations or any injuries of the vertebrae and intervertebral discs.
- The causes of pain or numbness in the limbs.
- Developed inflammation of the spinal column, myelinopathy or myelinoclasty.
- The presence of narrowing of the spinal canal.
- Conditions of protrusions or hernias, osteoarthrosis or osteoarthrosis.
The study is carried out without any specific preparation and takes about 20 minutes.
MRI of a uterine scar
A scar on the uterus can occur in women who have experienced:
- Carrying out a caesarean section.
- Some gynecological operations, for example, myomectomy or reconstructive plastic surgery.
- Uterine rupture in previous births.
- Damage caused by invasive procedures.
- Abdominal injuries.
MRI is aimed at determining the condition of the scar left on the uterus and is a way to determine the extent of its thinning and the risk of rupture. The study will help specialists decide on the most appropriate method of delivery.
The presence of a uterine scar does not always guarantee complications in pregnancy and childbirth, but monitoring its changes is an integral part of gestational control.
Pelvis and joints on the limbs
The pelvis and joints of the limbs are examined in a number of situations:
- The appearance of pain syndrome.
- Existing anomalies in the development of joints.
- Damage to bone tissue, existing infectious or degenerative processes affecting bones and joints.
- Determination of the state of neoplasms.
- Existing connective tissue pathologies.
- Entry of foreign bodies.
- Suspicion of fluid accumulation in the pelvis.
There is no need for special preparation before the examination and the tomography takes no more than 30 minutes.
Are there alternatives to MRI?
Is it necessary to do an MRI of the head, neck, pelvis and other parts of the body during pregnancy, or can you use other hardware diagnostic options? In some cases, it is quite possible to choose. For example, if there is a suspicion of diseases of the internal organs, a woman can resort to the already classic ultrasound - it is cheaper, and, like tomography, does not pose any danger. However, there are a number of situations when MRI cannot be done, and the patient must take a risk by choosing radiography.
X-ray or MRI?
Can pregnant women have an X-ray of the brain or pelvis instead of an MRI? When answering this question, you need to carefully weigh all possible consequences. It is no secret that X-ray radiation, having a long-term effect on the body, destroys soft tissues and changes the structure of DNA. However, if you wear metal prostheses or pacemakers, then radiography becomes the only possible option. It is this method, due to its efficiency, that is prescribed for internal bleeding. MRI is not so quick, which can significantly worsen the situation.
When is an MRI completely contraindicated during pregnancy?
To prescribe an MRI, a specialist needs not only indications for it, but also the absence of contraindications. During pregnancy, it is strictly forbidden to carry out such diagnostics in a number of cases:
- Less than 12 weeks. This is due to the fact that this period of gestation is associated with the beginning of the formation of all organs. At this time, any influence exerted on the fetus, be it heat or noise (which are typical for MRI), can negatively affect the processes of embryonic systems.
- A pacemaker installed in a pregnant woman, or any metal or dentures.
- A woman's body weight exceeds 200 kg.
- Tendency to epileptic seizures, a history of claustrophobia or convulsive syndrome.
For MRI with the use of a contrast agent, the following are contraindications:
- Chronic kidney pathologies.
- Hemolytic disease in the mother.
The condition of the expectant mother is carefully examined by a specialist before he makes a final conclusion about whether she can undergo an MRI.
MRI is deservedly considered a highly informative and extremely safe procedure that does not require any specific preparation. Timely diagnosis can help not only to begin treatment measures to help the pregnant woman, but also to prevent some complications, such as rupture of the uterine scar. It can be carried out in virtually any case, but the effect of a tomograph on a pregnant woman and her baby is a more serious issue. It requires the most informed decision of a specialist.
What is MRI and how does it differ from other studies?
Magnetic resonance imaging is a method of obtaining a “picture” of internal organs to assess their structure and condition. The human body is three-quarters water; A strong magnetic field is formed inside the tomograph, which acts on hydrogen atoms, causing them to absorb energy and then emit it. Clear photographs of an area of the body or a specific organ are obtained, and from different angles - almost in 3D mode.
Not a single detail in the studied area of the body will be hidden from the “all-seeing eye” of the tomograph.
A computer program analyzes the data and translates the information into an image on the screen.
The first tomographs appeared in clinics by the early 80s of the 20th century; the devices gave a flat “picture”, and during the MRI procedure, patients experienced unpleasant sensations. In the first years of the 21st century, it was possible to achieve a two-dimensional image and eliminate the body’s negative reactions; tomographs continue to improve, and the MRI method is recognized as leading in the field of diagnostics.
Advantages of MRI:
- high contrast of images, which means image accuracy;
- ease of operation of the device;
- diagnosis of microscopic changes in the structure of an organ or tissue, allowing to detect pathology at an early stage;
- reliability of results;
- safety of the procedure for the body.
The arsenal of a tomograph, an entire software and hardware complex, includes radio waves and a magnetic field; No negative effects on organs and tissues were detected during operation of the device. This MRI compares favorably with other hardware diagnostic methods - radiography and computed tomography, where one cannot do without high-frequency ionizing radiation, which causes cell mutation. Just 4 examinations using X-rays give the annual rate of radiation load on the body.
True, X-ray scanning lasts several seconds, and the MRI procedure lasts from 20 minutes to one hour; Patients with severe pain or claustrophobia find it difficult to withstand examination in a tomograph. The study will also give an error if a person has implants - electronic or metal. And implants do not affect the results of radiography.
Is MRI dangerous for pregnant women?
This relatively young diagnostic method has not yet earned the rating of “completely safe for expectant mothers.” So far, no negative consequences of MRI have been identified, however, theoretically, doctors assume complications may arise in pregnant women. A patient in position is sent for an MRI only if a threat to life or health is detected. You shouldn’t lie down under the influence of a magnetic field just out of curiosity.
In the early stages, the most important thing happens in the mother’s womb: the fetus’s organs and systems are formed, and disruption of this process can lead to serious consequences. In addition, the baby is not yet protected by the placenta. Gynecologists prefer to play it safe and avoid prescribing MRIs for pregnant women in the 1st trimester. But when a girl had the procedure done, not yet knowing about conception, there is no reason to panic; The doctor won't even prescribe additional medications. No developmental abnormalities were found in children whose mothers underwent MRI in the 1st trimester over the years of using the procedure.
However, in the case of MRI, it is premature to talk about decades of observation; There is no information yet about possible changes in the health of adults who were exposed to radio waves during fetal development. Experiments were carried out on animals and no negative effects were found.
So the method is recognized as safe for the woman and the fetus, but with reservations and precautions. The story with ultrasound is encouraging: previously, ultrasound diagnostics were suspected of having a harmful effect on babies in the womb, but later the suspicion was removed. Perhaps the same thing will happen with MRI.
With or without contrast agent
To obtain high-quality images, magnetic resonance imaging uses a substance called gadolinium, a soft silvery metal; Before being placed in a tomograph, the patient is given contrast with gadolinium salts intravenously.
Information about the properties of gadolinium is conflicting; The metal continues to be studied in laboratories. Until recently, the substance was considered low-toxic and left the body quite quickly. New research conducted in the United States raises concerns: the metal is recognized as toxic and capable of accumulating in the body.
The clinical consequences of substance retention are still being studied. It was found that gadolinium salts overcome placental protection; This property alone is a sufficient basis for prohibiting a contrast element when performing an MRI on a pregnant woman.
MRI with the use of contrast agents containing the metal gadolinium is contraindicated for expectant mothers
In addition, gadolinium can provoke allergic reactions.
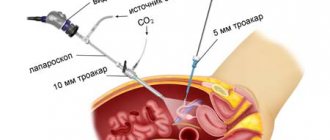
Exceptions for CT scanning for pregnant women
Let's consider cases when pregnant patients are still prescribed CT. Such exceptions include studies:
- cervical spine,
- skulls,
- brushes,
- feet,
- chest.
A CT scan can reveal dangerous tumor growths, various inflammations, and diseases of soft tissues and bones.
The need for a computed tomography scan is determined by the attending physician. It is important to understand that CT scans are prescribed for pregnant women in exceptional cases, such as when the risk of suffering from a possible disease significantly exceeds the effect of X-ray radiation on the pregnant woman’s body and the fetus. (For example, if a patient has infectious and inflammatory diseases, tumors, or extensive injuries, then the woman’s health will be a priority).
The most dangerous period for performing a CT scan is from 8 to 15 weeks of pregnancy. Before and after this period, the effect of CT on pregnancy will be lower.
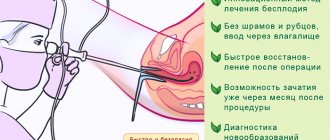
When is a fetal tomography prescribed?
During pregnancy, an MRI can be prescribed to examine not only the woman, but also the unborn baby. The need for such a procedure arises if:
- Ultrasound examination of the fetus is not possible due to maternal obesity.
- The fetus is positioned incorrectly, making it difficult to examine in other ways.
- The screening results showed pathologies of fetal development, and their confirmation or refutation is necessary before artificial termination of pregnancy for medical reasons.
During pregnancy, MRI of the fetus is rarely done: to track its development, the data obtained from examining the mother’s blood and ultrasound of the unborn baby is sufficient. This research method is used in cases where the question of maintaining or terminating a pregnancy arises.
What pathologies are diagnosed?
There are many diseases that begin with the above symptoms, and most of them can be quickly cured if detected in the early stages of development.
An MRI of the head will reveal the following pathologies:
Contrast MRI of the brain
- oncological foci;
- vascular disorders;
- pituitary gland abnormalities;
- nerve diseases;
- hemorrhages, strokes;
- structural brain disorders;
- causes of headaches and other symptoms.
Thanks to the capabilities of MRI, it is possible to take pictures of any projection of the brain, which will provide a detailed examination of its organs from all angles and see even the smallest disorders that can overshadow the life of a pregnant woman.
So you don’t need to condemn yourself to several months of suffering while waiting for the birth of your baby, but take the advice of a specialist who wants to help get rid of the unpleasant manifestations of the disease.
Consequences of CT scanning for pregnant women
Sometimes there are cases when a woman had a CT scan without knowing that she was pregnant, for example, at 4-5 weeks. Let's try to figure out what to do in such cases, whether it is necessary to terminate the pregnancy and what the consequences are for the fetus.
There is no need to make hasty conclusions if a CT scan was performed at such an early stage. The fetus at 4-5 weeks is not yet so much exposed to x-ray radiation. And if its mutation does occur, then with a high degree of probability, the woman’s body will reject the fetus, which will lead to a miscarriage of the embryo. If this does not happen, then the birth of a healthy child is quite possible. In any case, various developmental anomalies can be detected by ultrasound examination up to 18 weeks of pregnancy, and then decisions can be made.