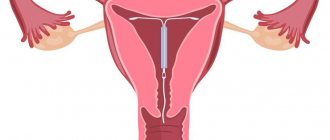
In vitro fertilization (IVF for short) is often the only chance to get pregnant. Before artificial insemination or transfer of embryos into the uterine cavity, it is necessary to conduct a thorough examination of the uterine cavity to ensure that the organ is ready to carry a pregnancy. For this purpose, hysteroscopy is performed before IVF - a procedure that can be both diagnostic and therapeutic. In order for it to be as effective as possible and not lead to complications, it is important to correctly select the appropriate date for the manipulation, as well as evaluate the feasibility of the procedure as a whole.
What is hysteroscopy
If we explain the essence of diagnostic hysteroscopy in simple language, then it comes down to examining the uterus (its cervix, cavity and tubal orifices) using optical (fiber optic) devices (hysteroscope, hysterofibroscope and hysteroresectoscope).
In modern gynecology, hysteroscopy before IVF has become the most popular endoscopic examination. This method is considered completely safe, does not threaten women's health and does not interfere with getting pregnant. This method is unique in that it can provide a solution to several issues at once regarding the prevention and detection of problems in a woman’s gynecological health. This optical method can be used for the following purposes:
- surgical;
- diagnostic;
- control.
The diagnostic test consists of a qualitative examination of the uterus.
During surgical exploration, the integrity of the uterine mucosa is disrupted.
The control method is carried out to assess the quality of the treatment provided.
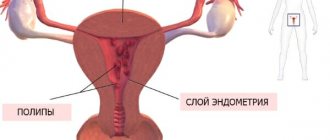
Thanks to hysteroscopy, the causes of many gynecological pathologies are identified (inflammatory diseases, endometrial polyps, infertility, bleeding) and the identified pathologies are immediately treated (polyps, adhesions, etc. are removed)
Diagnostic hysteroscopy
This type of examination is also called “office hysteroscopy.” The procedure is characterized by the fact that it can be carried out in the gynecologist’s office, and not on the surgical table.
Office hysteroscopy is carried out for research purposes and differs from usual in that the device itself is less than 3 mm thick. This means that neither local nor general anesthesia is required. In some cases, a woman may be prescribed sedatives.
Office hysteroscopy is performed in cases where the doctor knows for sure that the woman does not require surgical intervention. Such a procedure may only involve inspection and collection of the necessary material.
The procedure is diagnostic in nature, therefore, for example, hysteroscopy for endometriosis can show thickening of the endometrium, but cannot completely cure the disease.
Indications for Hysteroscopy
- Endometrial cancer;
- Infertility;
- Not systematic gestation;
- Monitoring during hormonal therapy;
- Foreign body in the pelvic organs;
- Clarifying the location of the intrauterine device;
- Examination in the postoperative period to ensure there are no blood clots;
- Perforations in the walls of the uterus (fistulas);
- Menstrual irregularities;
- Before the in vitro fertilization procedure, in order to ensure that there are no contraindications to it.
Contraindications to Hysteroscopy
Office hysteroscopy is contraindicated for women who:
- The result of a vaginal smear showed the presence of infections;
- Inflammatory process in the pelvic organs;
- During tonsillitis, acute respiratory infections, ARVI, pneumonia.
What is needed for the procedure
To conduct an examination, a woman must provide the following research results:
- General blood analysis;
- Blood test for Rh factor;
- Blood test for hepatitis B and C;
- Blood for PW and AIDS;
- Results of smears from the uterus and canal;
- Colposcopy results;
- Fluorography;
- ECG results;
- Ultrasound of the pelvic organs.
7 days before the procedure, the woman must stop douching and use vaginal suppositories or tampons. You cannot have sexual intercourse for a couple of days, and the day before you need to do an enema.
After the procedure
Hysteroscopy most often takes place without consequences for the body. After the manipulations, the woman is recommended to abstain from sexual intercourse for at least 2-3 weeks.
She should also protect herself from physical activity and visiting baths and saunas. A woman should not forget about the hygiene of the external genitalia. If suspicious discharge or discomfort (itching, rash and redness) appears, she should consult a doctor.
It is necessary to measure body temperature after the procedure. It shouldn't go up. There should be no chills, fever or weakness. Pain in the area of manipulation, that is, in the lower abdomen, is normal. Only if this pain lasts longer than 4-5 days should a woman visit a gynecologist.
Blood discharge within 3 days after manipulation is considered normal. It is important for a woman to ensure that blood does not fill more than 1 pad per hour, otherwise this is internal bleeding.
If during hysteroscopy diagnostic curettage of the uterine walls, removal of polyps or a biopsy was performed, then bleeding may continue for up to 7 days. They also should not fill more than 1 pad per hour.
Hysteroscopy and IVF
This procedure allows for the timely identification and treatment of diseases that may interfere with the successful attachment of the embryo and its gestation.
Hysteroscopy before IVF significantly increases the chances of a successful fertilization outcome. During the procedure, the doctor may perform manipulations to cauterize the cervix, dissect adhesions and partially scrape out the endometrium.
Hysteroscopy before IVF is a mandatory procedure. During this procedure, the walls of the uterus are examined for the presence of any diseases that interfere with the successful implementation of in vitro fertilization.
If it is not carried out, the woman and the doctor cannot be 100% confident in the successful outcome of IVF. In some clinics, doctors do not perform this procedure.
From the point of view of fertility doctors, this is the wrong method. You cannot be guided solely by test results in order to say with confidence that the embryo will implant and the pregnancy will proceed normally.
Advantages of the procedure - Hysteroscopy for IVF
After unsuccessful IVF, you should also undergo hysteroscopy. If the pregnancy is terminated 2 or more times after in vitro fertilization, and the doctor does not prescribe a test, the woman should sign up for this procedure herself.
Stimulation of the ovaries, collection and fertilization of eggs, their transfer and maintenance in a cryochamber in the future are very expensive manipulations. In order not to have them done over and over again, a woman should undergo hysteroscopy to determine the reasons for “failure to carry a pregnancy.”
Before cryotransfer, it is also recommended to perform a hysteroscopy to ensure the absence of polyps, adhesions and endometriosis.
Pregnancy may not occur precisely for these reasons. A frozen embryo may be of the best category, but will not implant due to concomitant diseases.
Advantages of this procedure
The most important advantage is the information content of the method. The doctor can clearly see the inner layer of the uterus on the monitor and can easily determine the presence of any diseases.
It is impossible to achieve the same information content and accuracy with ultrasound examination. When removing a polyp, other tissues are not damaged, and there is no need for abdominal incisions (albeit microscopic) during laparoscopy.
Possibility of a “gentle” abortion. This method of terminating a pregnancy will cost a woman several times more.
But this procedure guarantees accuracy and minimization of injuries. The chance of getting pregnant after this type of interruption is much higher than after medical abortion and vacuum.
Cons of the procedure
The most important disadvantage is limited action.
Hysteroscopy can help detect diseases of the cervix, the uterine cavity itself and the fallopian tubes.
But the procedure is not able to identify problems in the ovaries and distant parts of the fallopian tubes, which is where the largest number of adhesions usually occur.
Why is hysteroscopy needed before IVF?
Hysteroscopy prescribed before IVF allows a woman to replace several unpleasant procedures at once (for example, curettage in a hospital setting). Ultrasound, for example, is not able to detect minor intrauterine pathologies. The hysteroscopy method and its optical capabilities make it possible to:
- assessment of patency of the cervical canal;
- diagnostics of endometrial health;
- cauterization of erosions;
- cervical biopsy;
- dissection of adhesions or intrauterine septa;
- removal of polyps.
This method also allows the doctor to choose the correct IVF protocol scheme and treatment method.
Hysteroscopy before IVF is not mandatory but extremely useful and desirable. Most often, this method is used for diagnostic purposes (office hysteroscopy), but sometimes it is combined with minor surgical procedures (curettage).
Most women believe that successfully performed IVF already guarantees the result of bearing and delivering a healthy child on time. However, many gynecological pathologies of the mother can interfere with the successful continuation of pregnancy and reduce this expensive procedure to nothing.
Therefore, it is completely justified to perform a hysteroscopy before a number of negative embryo transfer results are obtained. This will maximize the chances of a successful pregnancy and birth of a child.
Indications for hysteroscopy
Is hysteroscopy necessary before IVF - that’s the main question. There are two opinions on this matter.
The first is that this procedure is mandatory before IVF, because Using this method, a doctor can exclude or confirm the uterine genesis of a woman’s infertility. Namely, the reason for the lack of pregnancy can be all those formations that are described above, and when performing hysteroscopy, the surgeon not only assesses the condition of the endometrium, but can remove everything that interferes with the implantation of the embryo. And besides, the injured endometrium provokes active growth of the functional layer, which is what allows the embryo to better implant itself on the wall of the uterus.
Another opinion is that this procedure is not necessary, since there are no direct indications, and the woman will not be subjected to anesthesia, the preparation time for IVF is reduced. Considering all this, whether hysteroscopy before IVF is necessary, only your doctor decides.
Hysteroscopy of the uterus before IVF has the following indications:
- a history of several unsuccessful attempts;
- habitual miscarriage;
- signs of abnormal development of the uterus;
- infertility of unknown origin;
- frequent uterine bleeding.
This procedure is very effective, as it helps to identify diseases that reduce the chance of getting pregnant, for example: polyps, endometrial hyperplasia, endometriosis, developmental abnormalities, bleeding, uterine fibroids, adhesions, synechiae.
What can be determined during hysteroscopy
By prescribing a hysteroscopy method before IVF, the doctor thereby aims to prepare the endometrium for the most successful in vitro fertilization. This method is called minimally invasive, that is, it is as harmless as possible to the woman’s health. In addition, how to carefully assess the condition and quality of the uterine mucosa; with this endoscopic method, it is possible to simultaneously perform minor surgical interventions to remove obstacles to the implantation of the embryo in the uterine cavity (benign neoplasms, nodes, adhesions, etc.)
Thanks to this minimally invasive method, it is possible to identify the following types of pathologies:
- hyperplasia, polyps or atrophic changes in the endometrium;
- congenital pathology of the uterus;
- adenomyosis;
- foreign objects;
- intrauterine synechiae;
- submucosal nodes.
Very often, women suffering from infertility experience several pathologies of the gynecological organs, which can actually be identified during examination.
Why is examination carried out before IVF?
If a married couple has already had an unsuccessful attempt at in vitro fertilization, hysteroscopy with separate diagnostic curettage (RDC) is mandatory. The specialist prescribes an endoscopic examination before in vitro fertilization and performs certain manipulations.
These include:
- assessment of patency of the cervical canal;
- determination of the condition of the internal mucous membrane;
- possibility of cauterization of erosions;
- cervical biopsy;
- carrying out dissection of septa or adhesions inside the uterus;
- removal of polyps.
Why is the procedure necessary before IVF? It allows you to select the necessary in vitro fertilization protocol scheme and treatment tactics for the doctor. This method replaces several diagnostic procedures for the patient - ultrasound, which sometimes cannot detect minor pathological changes in the uterus, and curettage in a hospital setting.
The study allows the doctor to detect the following disorders in the patient:
- congenital anomalies of the uterus;
- submucosal nodes;
- synechia;
- hyperplasia or atrophic processes in the endometrium;
- polyps;
- adenomyosis;
- foreign objects.
Quite often, women suffering from infertility have several types of disorders in the reproductive system. With the help of hysteroscopy, specialists can prepare the body for IVF as fully as possible, curing diseases.
Preparing for the study
There are a number of rules for preparing for this study. It includes both a special examination and drug treatment. Before hysteroscopy, a thorough examination of the woman is necessary, which includes:
- gynecological examination on a chair;
- fluorography;
- examination of discharge (from the vagina, cervical canal) for microflora and degree of purity;
- analysis to determine helminthic infestations;
- Ultrasound of the pelvic organs;
- complete blood count, determination of blood group and Rh status;
- blood tests for dangerous infections (syphilis, AIDS);
- other types of studies as indicated (blood biochemistry, urine analysis, cardiac ECG, consultation examination by doctors of other specialties, etc.)
There are also rules for the women themselves who are undergoing this endoscopic examination. The main ones include:
- taking a shower before the procedure, shaving the perineum and pubis;
- for anxiety before bed, take light sedatives (Novopassit, motherwort, peony, valerian, etc.);
- emptying the bladder before the study;
- leave decorations at home;
- take with you a set of hygiene products (pads, clean shirt, cotton socks);
- 2 hours before the procedure, the doctor prescribes one of the antibiotics to prevent infectious complications.
Who should refrain from hysteroscopy - contraindications
Despite its effectiveness and relative safety, in some cases the procedure cannot be carried out categorically.
Contraindications to endoscopic examination:
- The patient is in serious condition.
- The development of any infectious diseases in a woman.
- Malignant neoplasms of the cervix and the threat of their spread to surrounding tissues.
- The presence of uterine bleeding, which significantly impairs the effectiveness of the procedure.
- Violation of the coagulation properties of blood due to the threat of massive bleeding after the study.
- Menstruation: They obstruct normal vision of the uterine cavity.
- The appearance of inflammation in the reproductive organs: before hysteroscopy, it is necessary to carry out a treatment course for an acute disease or an exacerbation of the chronic course of the disease.
- Severe narrowing of the cervix: during passage of the instrument there is a high risk of damage to the integrity of the cervical canal.
In these cases, the procedure is prescribed solely for health reasons.
On what day is hysteroscopy done before IVF?
Most often, the hysteroscopy procedure is performed on days 5-7 of the cycle (proliferative phase). It is at this time that the uterine mucosa is least susceptible to bleeding.
The procedure is not recommended at other times for the following reasons:
- risk of bleeding;
- possibility of complications;
- low information content of the procedure (due to thickening of the endometrium).
Occasionally, the procedure is recommended for 3-5 days before the start of menstruation (in the secretory phase).
Indications for hysteroscopy before IVF
Like any endoscopic examination, hysteroscopy has its indications and contraindications.
This method may be indicated for:
- Disorders of the cervical canal (areas of narrowing, foreign bodies, polyps).
- Intrauterine disorders (polyps, nodes, synechiae, hyperplastic or dystrophic processes, chronic endometriosis).
- Several unsuccessful attempts at IVF.
Contraindications
No matter how good and effective hysteroscopy is, in some cases it is absolutely forbidden.
Contraindications for this method are:
- The patient’s serious condition for any ailment (until the condition is fully compensated).
- Any infectious diseases (due to the risk of infection spreading in the body).
- Cancers of the cervix (due to the risk of spreading to surrounding tissues). This can be facilitated by liquid media used during manipulation.
- Uterine bleeding. However, this procedure will have low effectiveness due to the presence of blood clots in the uterus.
- Pathologies of blood clotting (due to the risk of severe bleeding after any surgical interventions).
- Menstruation. Due to the low effectiveness of the study (poor review), it is carried out no earlier than 5-7 days of the cycle.
- Inflammatory processes in the genital organs. This method is not used for exacerbation of chronic ailments. It is first important to treat inflammation and reduce the activity of ongoing pathological processes.
- Narrowing (stenosis) of the cervix. This can seriously damage the integrity of the canal when the endoscope is inserted.
In all such cases, hysteroscopy is performed only for health reasons.
Who is contraindicated for testing before artificial insemination?
Before diagnostic hysteroscopy is performed, the doctor must make sure that the patient has no contraindications to such manipulations. These include:
- infectious processes in the body;
- chronic diseases in the acute stage;
- menstruation;
- cervical stenosis.
These same conditions are a contraindication to hysteroscopy with RDV before IVF.
Interesting fact! According to WHO statistics in the United States for 2020, 1.5% of patients with previously diagnosed infertility were denied pre-IVF hysteroscopy due to a naturally occurring pregnancy.
To exclude the presence of contraindications, before each examination using a hysteroscope, the doctor gives a referral to the woman for a comprehensive diagnosis, which includes:
- Ultrasound of the uterus and pelvis;
- laboratory tests of urine;
- laboratory blood tests;
- microbiological examination of a smear from the vagina and cervix;
- examination in the gynecologist's chair, which allows you to assess the current condition of the cervix and the reproductive organs;
- consultation with a therapist in the presence of chronic diseases.
The final answer to the question of whether hysteroscopy is needed for IVF or whether the procedure should be abandoned is given by the final examination. Immediately before the procedure, the doctor may ask the patient to measure her body temperature to make sure that she has no signs of a hidden inflammatory process. If abnormalities are detected during this examination, further diagnostics may be required. After this, the patient will be prescribed treatment, and after that it will be possible to repeat the attempt at hysteroscopy.
How is hysteroscopy performed?
Most often, diagnostic hysteroscopy is used before IVF. The procedure is performed in a gynecological clinic or center. The procedure can also be performed on an outpatient basis.
No incision is made during this study. Optical equipment is inserted into the body through the vagina.
The sequence of such a study is as follows:
- The patient is in a gynecological chair.
- Previously, this operation was performed without anesthesia. However, due to the pain, the manipulation is now performed under general short-term anesthesia (usually intravenous drip). If intravenous anesthesia is contraindicated, mask anesthesia is used.
- In rare cases, other types of anesthesia are used (epidural, spinal, endotrachial anesthesia).
- During the study, the main vital functions of the body (cardiac activity, breathing) are monitored.
- Treatment of the external parts of the genital organs and the surface of the thighs (inner) with an alcohol solution.
- Exposure of the cervix using a vaginal speculum.
- Insertion of a probe into the uterine cavity with Hegar dilators.
- Introduction into the cavity of a special composition that allows you to examine uterine abnormalities.
After opening the cervical canal, insertion of the hysteroscope.
- On the monitor, the surface of the uterus is enlarged and perfectly visible.
- If necessary, microoperations are performed in the cavity (curettage of the uterine mucosa, removal of polyps, etc.)
- The image being manipulated is written to disk.
- At the end of the operation, the hysteroscope is removed and the uterine cervix closes spontaneously.
- After recovery from anesthesia, the woman is observed by an anesthesiologist for at least 2 hours.
- Usually the patient is inpatient (from several hours to 4 days).
What is hysteroscopy and what problems does it solve in the fight against female infertility?
In the treatment of infertility in women, hysteroscopy and IVF are often inextricably linked. Firstly, this procedure allows us to identify pathologies of the uterus that prevent the occurrence and successful gestation of pregnancy. Secondly, it is used to prepare the uterus for the process of bearing a fetus, as well as to eliminate detected pathologies. Thirdly, despite the fact that hysteroscopy involves penetration into the uterine cavity, it is the most gentle diagnostic and therapeutic method in gynecology. The procedure can significantly improve the prognosis of artificial insemination, and in some cases it helps the patient become pregnant on her own.
The essence of the procedure is to examine the uterine cavity using a special device - a hysteroscope. It is a device equipped with a thin tube, at the end of which there is a light source and a video camera with the possibility of multiple magnification. The image from it is fed to the monitor, thanks to which the doctor will be able to see even minor changes in the endometrium of the uterus, in the submucosal layer of the organ cavity and the mouths of the fallopian tubes. The design also contains medical manipulators: forceps, loops, scissors, coagulator and others. With their help, the doctor can:
- take biological material from the cervix and uterine cavity for more in-depth research;
- eliminate causes of infertility such as synechiae, uterine septum, fibroids and polyps;
- remove foci of endometriosis in the uterine cavity;
- eliminate cervical erosion.
The procedure is indicated at the stage of diagnosing infertility; it is used to eliminate obstacles to pregnancy. Hysteroscopy is performed after unsuccessful IVF and after spontaneous fading of pregnancy, miscarriage and long-term absence of natural pregnancy. This procedure is absolutely safe and painless (local or general anesthesia is used). It greatly increases the chances of successful conception and delivery, which is why most gynecologists and reproductive specialists recommend this procedure to women.
Important! The timing of hysteroscopy and when IVF can be done after it are considered individually, depending on the causes of infertility and the individual characteristics of the patient.
Despite the high effectiveness rates (more than 10% of patients become pregnant on their own after hysteroscopy), the procedure cannot be called a panacea in the treatment of infertility. Sometimes difficulties with conception and pregnancy arise for other reasons. In this case, the results of hysteroscopy also play a significant role in diagnosis: if no pathological changes are found directly in the uterus, the doctor will more carefully look for causes in the endocrine and other systems.
How should a woman behave after the procedure?
After the procedure, a woman is usually recommended the following course of action:
- take antibiotics according to the regimen prescribed by your doctor;
- hygienic washing of the genitals (twice a day);
- daily temperature measurement twice;
- for painful manifestations, use painkillers recommended by the doctor;
- exclusion of bathing in the bathtub or ponds (only a shower is acceptable);
- exclusion of any stress (physical, psychological), sexual activity, thermal procedures (for at least 2 weeks);
- monitor the type and amount of discharge from their genitals.
IVF after hysteroscopy: medical statistics about increasing chances
According to the observations of practicing gynecologists-reproductologists, the chances of a positive IVF result after hysteroscopy increase significantly. Thus, successful embryo implantation occurs 30-60% more often, the number of miscarriages is reduced by 20-40%, and the number of unsuccessful IVFs is minimized.
To achieve the desired result, just carrying out the procedure is not enough. In the postoperative period, you should strictly adhere to medical recommendations for better recovery. Avoid intense physical activity, try to be in the fresh air more often and avoid stressful situations, and eat right. Depending on the clinical picture, the specialist will prescribe drug treatment (if required).
When drawing up a new IVF scheme, the detected anomalies will be taken into account, which will make it possible to draw up a more accurate embryo transfer protocol.
At the Genesis clinic, which specializes in the treatment of infertility, including ART methods, diagnostic, surgical and control hysteroscopy is performed by gynecological surgeons with many years of practical experience. Thousands of successfully performed operations and the availability of modern equipment allow us to reduce operational and postoperative risks and ensure high efficiency of IVF after hysteroscopy. You can make an appointment by calling the phone number listed on the website, or by coming in person to the address St. Petersburg, Kirochnaya St., 64. Still have questions? We are waiting for your call to inform you about the manipulation in more detail.
Possible complications
Complications after hysteroscopy are very rare. This method is minimally traumatic and is in no way comparable to conventional uterine curettage. However, sometimes after this procedure I may have:
- spasmodic pain in the lower abdomen;
- slight bleeding or “spotting”;
- flatulence after anesthesia.
Usually all these troubles are harmless and disappear after a few days.
Immediate consultation with a doctor is required when a woman experiences breakthrough bleeding and abdominal pain.
Thus, hysteroscopy before IVF is a very revealing type of study. Many pathologies (for example, polyps) are diagnosed with 100% accuracy. At the same time, you can get rid of these pathologies. Take care of your health and the health of your future children!
What hormonal medications did you take to stimulate ovulation?
- Gonal 33%, 3977 votes
3977 votes 33%3977 votes - 33% of all votes
- Clostilbegit 25%, 2989 votes
2989 votes 25%
2989 votes - 25% of all votes
- Menopur 16%, 1937 votes
1937 votes 16%
1937 votes - 16% of all votes
- Puregon 14%, 1699 votes
1699 votes 14%
1699 votes - 14% of all votes
- Decayed 8%, 984 votes
984 votes 8%
984 votes - 8% of all votes
- Menogon 3%, 365 votes
365 votes 3%
365 votes - 3% of all votes
Total votes: 11951
Voted: 8788
January 17, 2018
×
You or from your IP have already voted.
Sources used
- Hysteroscopy / L. F. Mozheiko, G. I. Gerasimovich; Minsk Medical Institute // Medical news: magazine. — 1996.
- Treatment of female and male infertility. Assisted reproductive technologies / Kulakov V.I., Leonov B.V., Kuzmichev L.I. - M.: Medical Information Agency, 2008.
- Zuev V.M. Treatment of benign diseases of the cervix, vagina and vulva using a CO2 laser: Abstract of thesis. dis. Ph.D. honey. Sci. - M., 1988.
- St. Petersburg State Budgetary Healthcare Institution “Family Planning and Reproduction Center”
How is hysteroscopy performed?
Nowadays more advanced methods are used; hysteroscopy is mandatory before IVF. Equipment and methods may differ depending on the goals pursued. A gyroscope is used - a narrow tube with an LED and a camera, which is inserted into the cavity, and the image is transmitted to the monitor screen. The picture enlarges as you approach the area of interest.
Hysteroscopy before IVF allows the doctor to carry out in detail and in a convenient manner:
- examination of the uterine mucosa (endometrium);
- check the patency of the fallopian tubes;
- study the slightest features of genital diseases.
For diagnostic purposes, hysteroscopy usually takes 5–40 minutes. You can return home almost immediately. It is also called “office”, since the procedure is simple to carry out and causes minimal inconvenience. It can be performed by a gynecologist, without using a surgical table.
For diagnostic hysteroscopy, a thinner device is used: less than 3 mm. Anesthesia is usually not needed. Sometimes sedatives are used. Diagnostics involves only examination and collection of a small amount of material for research.
The days of the menstrual cycle must be taken into account: hysteroscopy before IVF is scheduled on days 6–10 of the menstrual cycle. At this time, the walls of the organ are thinner, which makes inspection easier. Hysteroscopy does not affect the ovulation process. During this period of the cycle, blood loss during surgery will be less. Hysteroscopy is also a gentle surgical method.
In a very short time you can, for example:
- cut adhesions;
- cauterize the erosion;
- remove polyp.
Hysteroscopy is performed under anesthesia, so the procedure is painless. When carrying out manipulations the following are used:
- local anesthesia: cervix;
- general anesthesia.
Methods
Many women wonder how endometrial biopsy helps them get pregnant. It must be said that the procedure itself does not affect the process of conception. The results of the examination, as well as subsequent treatment, play a decisive role in this.
Depending on medical indications, the procedure can be performed using several methods. In most clinics, they do complete curettage of the mucosa, which is a traumatic biopsy. Vacuum aspiration and pipel biopsy cause the least harm. Let's take a closer look at the features of each method.
Scraping
The presented method of performing endometrial biopsy in medical practice is also called classical. To carry out the procedure, the woman must be given anesthesia, since it is associated with severe pain. Manipulations to remove the mucous layer are performed with a curette.
During the procedure, a medical instrument is inserted into the vagina, which completely removes the mucous layer of the reproductive organ and cervical canal. During the recovery period, the patient must be under the supervision of a doctor in a hospital setting.
Pipel
This type of biopsy is by far the safest and most painless, and does not require complex preparation. The woman needs to go to an appointment with a gynecologist. The night before, you need to carry out hygiene procedures, but do not douche.
How to do a pipel endometrial biopsy. Source: agu.life
The entire procedure is performed according to the following algorithm:
- The woman is positioned as comfortably as possible in the gynecological chair;
- Next, the doctor dilates the vagina with a special instrument;
- The cervix is then treated with an antiseptic solution;
- Finally, a sample of biological material is taken.
The duration of the procedure takes no more than five minutes, and the scraping itself is sometimes taken within a quarter of an hour. After this, the woman can go home, since there is no need to stay in hospital. Manipulations are carried out on days 21-23 of the menstrual cycle, sometimes a biopsy is done before regular bleeding (about 5-7 days).
As for the cost, it varies depending on which clinic performs the procedure. The price can range from 1800-8000 rubles. Diagnostic results can be obtained in about 10 days, which is when the doctor will be able to make a final diagnosis and prescribe treatment.
Aspiration
Another common method for diagnosing the endometrium before IVF is aspiration biopsy. This procedure is a minimally invasive surgical procedure, but is not accompanied by severe pain.
Needle for performing aspiration biopsy of the endometrium. Source: epikriz.com.ua
To perform a biopsy, a specific syringe with a unique design is used. Thanks to it, endometrial cells are aspirated from the uterine cavity. A long needle-like tip is inserted into the reproductive organ itself. To carry out the procedure, the patient does not need to be anesthetized, and the body does not need to be thoroughly prepared beforehand.
The cost of an aspiration biopsy is identical to a pipel biopsy. It is very important that a woman trusts the procedure only to those clinics that have a special license to perform such manipulations and an experienced gynecologist.
Other
In gynecology and reproductive medicine, especially when examining the genital organs before a planned in vitro fertilization procedure, they may resort to various methods for examining the endometrium, since it is the condition of this layer that determines whether the embryo will be able to attach to the wall of the uterus.
Some clinics resort to a procedure such as CGU biopsy. The main distinguishing feature is that the collection of biological material is carried out by line-shaped scrapings. After the procedure, women experience no pain and no bleeding.
During one cycle, no more than three CGU biopsies can be performed, but there is no negative impact on the body, the hormonal levels do not change, and the mucous membrane is not injured. Often, the indication for the procedure is a suspicion of a precancerous condition or the formation of tumors in patients before IVF.
The principle of hysteroscopy with biopsy. Source: mymammy.info
Hysteroscopy with biopsy may also be performed before in vitro fertilization. It is performed on patients who are suspected of developing uterine fibroids, hyperplasia, tumors or polyposis. Manipulations are performed under general anesthesia, and samples of the material are taken with a hysteroscope.