Treatment after hysteroscopy of an endometrial polyp is an important final stage of a complex of therapeutic measures, which reduces the risks of complications and relapse of pathology. From this article you will learn what is included in the final stage of treatment, why it is necessary, and also what the removal of formations in the uterus by hysteroscopy is.
Briefly about hysteroscopy
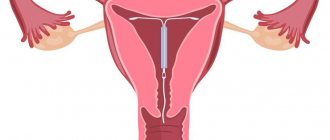
Hysteroscopy is a therapeutic and diagnostic manipulation that allows you to visually evaluate the uterus from the inside, identify pathological formations or anomalies in its structure and, if necessary, remove them promptly, that is, without penetrating the abdominal cavity. This method is endoscopic and is performed using a special optical device - a hysteroscope - by a trained specialist.
Translated from Greek, hysteroscopy means “to examine the uterus.” Manipulation can be diagnostic or therapeutic. Diagnostic hysteroscopy is performed not only to examine the internal uterine surface, but also to collect material (endometrium) for histological examination (biopsy). During therapeutic hysteroscopy, surgical interventions are performed, for example, removal of tumors or foreign bodies.
Chest hurts
A woman’s condition after hysteroscopy is very painful, and this happens very often, but if breast tenderness is mixed with the aching pain in the abdomen, this is an alarming symptom. Hormonal imbalances affect the entire body as a whole. The patient feels depressed and overwhelmed. But in addition to psychological problems, physiological ones are of great importance.
Important information: if your breasts hurt, most likely the level of progesterone in the blood exceeds the norm; it is very important to immediately consult a gynecologist for detailed advice. He will prescribe appropriate medications to normalize the patient’s condition as soon as possible.
Preparation for the procedure
Since hysteroscopy is an invasive procedure and is akin to surgery, before undergoing it the patient is prescribed an examination (excluding emergency cases):
- blood and urine tests (general tests);
- smears from the vagina and cervix to determine the microflora;
- blood for syphilis and hepatitis;
- blood for HIV infection;
- blood biochemistry (especially blood glucose in overweight patients);
- blood group and Rh factor.
The following instrumental methods are prescribed:
- Ultrasound of the pelvis;
- Ultrasound of the abdominal cavity (if indicated);
- fluorography;
- blood clotting test;
- ECG (if indicated).
If the patient has chronic extragenital diseases, a consultation with a doctor of the appropriate profile with corrective therapy is indicated. If colpitis is detected, vaginal sanitation is prescribed (up to 1–2 degrees of cleanliness).
The examination is carried out on an outpatient basis. After admission to the hospital, the patient is given a cleansing enema (bowel preparation) before the procedure, and immediately before hysteroscopy it is necessary to empty the bladder. Eating on the day of the procedure is prohibited due to intravenous anesthesia during hysteroscopy. Hysteroscopy is planned for days 5–7 of the cycle, that is, in the first (proliferative) phase, when the new functional layer of the endometrium has just begun to grow and the inner surface of the uterus is accessible for inspection.
It is also necessary to abstain from sexual intercourse 3 days before the procedure, and stop douching a week before. The use of spermicides and vaginal suppositories 7 days before hysteroscopy is also not recommended.
Chlorhexidine for thrush: what rules to follow during treatment?
Have you been fighting thrush for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure thrush by taking it every day.
75% of women have experienced symptoms of a fungal infection at least once in their lives. They especially suffer during pregnancy due to the physiological characteristics of this period of life. Despite the “banality” and prevalence of the disease, coping with it is not so easy.
To increase the effectiveness of therapy, doctors prescribe antiseptics along with antifungal drugs. Chlorhexidine for thrush (as an antiseptic) will be effective when prescribed in combination with antimycotics, and is not contraindicated during pregnancy.
Types of hysteroscopy
Hysteroscopy, depending on the purpose, can be:
- diagnostic – when it is necessary to identify the causes of “problems” in the female line (to diagnose endometrial polyposis, submucosal myomatous node or other pathology);
- therapeutic - after examining the inner surface of the uterus, surgical intervention is performed (excision of polyps, resection of a myomatous node, dissection of adhesions or septum in the uterus);
- control - carried out after a certain time (usually six months) after intrauterine interventions using hysteroscopy.
For a successful operation, it is necessary to straighten the uterine walls, stretch and expand the uterus. For this purpose, media are introduced into the uterine cavity. Depending on the medium used, hysteroscopy is divided into:
- liquid (saline solution or 5% glucose is injected);
- gas (carbon dioxide is introduced).
Office hysteroscopy
Office endometrial hysteroscopy is one of the options for diagnostic hysteroscopy and is performed on an outpatient basis. This name for the procedure comes from Europe, where hysteroscopy for diagnostic purposes can be performed not only by a gynecologist, but by a general practitioner, and it is performed on an outpatient basis, in medical offices (by Western definition - in offices).
Office hysteroscopy is called simple hysteroscopy, mini-hysteroscopy, diagnostic video hysteroscopy. The latter term implies showing the patient a picture of the inner surface of the uterus during the manipulation. Advantages of minihysteroscopy:
- low traumatic procedure (a hysteroscope with the smallest diameter is used, without expanding the cervical canal);
- there is no need for general anesthesia, which reduces the cost of hysteroscopy and the risk of anesthetic complications;
- Possibility of outpatient implementation, does not require hospitalization and does not affect the ability to work;
- short period of the procedure (no more than half an hour);
- good tolerance to manipulation;
- It is possible to perform an endometrial biopsy.
Recommendations
Hysteroscopy is a micro-operation, and the recovery period after it is not much different from classical ones. It is necessary to follow a number of recommendations to promote a speedy recovery and carefully monitor your condition.
During the postoperative period, it is forbidden to lift heavy things, loads and physically strain - this can cause bleeding. Its intensity can be so great that the patient begins to lose consciousness. You shouldn't joke about this. It’s better to gain strength, and after a week, with new strength, you can get back to work.
Until the injured area has completely healed, it is forbidden to use tampons. Only gaskets. It is also worth waiting at least a week before starting sexual activity again. The consequences of such negligence can be unpredictable.
Indications
The decision on the need for hysteroscopy is made by the doctor based on the following indications:
- various disruptions in the menstrual cycle in girls, women of childbearing and premenopausal age;
- bleeding and spotting in postmenopause;
- suspicion and for confirmation: submucosal myomatous node;
- adenomyosis;
- endometrial cancer;
- malformations of the uterus;
- intrauterine synechiae;
- perforation of the uterus;
- remnants of the fertilized egg and membranes;
- cervical cancer;
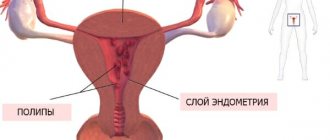
- polyposis and endometrial hyperplasia;
- foreign body in the uterine cavity;
Contraindications
Like any other intrauterine procedure, hysteroscopy is not performed in the following situations:
- acute infectious diseases (colds, sore throat, thrombophlebitis or pyelonephritis and others);
- exacerbation of chronic diseases;
- acute inflammation of the genital organs (colpitis, endometritis, adnexitis);
- intrauterine pregnancy (desired);
- ectopic pregnancy or suspicion of it;
- advanced cervical cancer;
- extragenital diseases in the stage of decompensation (cardiovascular pathology, liver, kidney diseases);
- profuse bleeding from the uterus;
- atresia of the cervical canal.
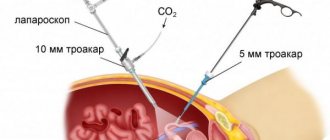
Progress of the operation
The hysteroscopy procedure for the removal of uterine polyps is carried out according to the following scheme:
- The woman is escorted to the operating room, where she removes her clothing and puts on a disposable gown.
- The patient lies down in the gynecological chair. Feet are protected with disposable shoe covers.
- The gynecologist begins treating the labia majora and inner thighs with an antiseptic.
- Then the patient receives intravenous anesthesia.
As soon as the patient falls asleep, the doctor begins work.
This type of study is carried out to study the general condition of the uterine cavity. The gynecologist examines:
- the fundus and lateral walls of the uterus;
- pipe angles;
- isthmus;
- cervical canal.
A physical examination allows you to identify the presence/absence of polyps, as well as assess the condition of the walls of the organ, the endometrial layer and the degree of patency of the fallopian tubes.
During surgical hysteroscopy, all detected polyps are removed.
- Removal of a tumor less than 1 cm in size is carried out using an electrode.
- Medium growths are cauterized or excised. In the latter case, scissors are used. Removal from the uterine cavity is carried out using surgical forceps.
- Parietal polyps and those identified at the mouth of the fallopian tubes are removed using a resectoscope loop.
- Large polyps are removed mechanically - using scissors, forceps - or electrosurgically using a resectoscope loop.
The exact duration of the operation cannot be given. On average it takes 30 – 45 minutes. If there are multiple polyps, it will take longer.
Recovery period
The recovery period after the manipulation is conventionally divided into 2 stages. The first stage consists of the primary restoration and normalization of the structure and functioning of damaged uterine tissue (mucous membrane and muscle layer). At the first stage, microdamages and surgical incisions are completely healed, and the cervical canal is restored and regenerated. This stage lasts about 2–3 weeks and ends with complete regeneration of surgical damage and the formation of scar-free tissue.
The second stage of recovery is aimed at the formation of new, newly formed tissue, that is, a new endometrium after hysteroscopy. The new uterine mucosa must have a normal structure and all its inherent functional properties (proliferation and rejection of the endometrium according to the phases of the menstrual cycle). The second stage of recovery requires more time and lasts up to 6 months.
Discharge after the procedure
Blood and moderate spotting will occur in the first 2 to 3 days after the procedure. This is explained by traumatic damage to the uterine mucosa by instruments. Subsequently, the discharge becomes bloody or yellow, which can last up to two weeks. The duration of ichor discharge is due to the expansion of the uterine cavity with liquid during hysteroscopy; the liquid penetrates into the vessels, damaging their walls, which leads to the release of “ichor”. But if heavy bleeding or blood clots appear, you should immediately consult a doctor.
Menstruation after hysteroscopy
When does your period come after hysteroscopy? It all depends on the purpose of the procedure. In the case of diagnostic, especially office hysteroscopy, menstruation occurs according to the usual cycle schedule, but slight delays are possible (2 - 3 days). This is explained by the fact that during the diagnostic procedure the endometrium is practically not injured, so a long time for its recovery is not required. But in the case of therapeutic hysteroscopy, especially after completion of the procedure by curettage of the uterine cavity, a longer delay in menstruation is possible. In this situation, the first day of the menstrual cycle should be considered the day of the operation and expect menstruation in about a month. It is important to monitor the nature of the first menstruation after the procedure. If there is a change in color or consistency, or an increase in the amount of bleeding, you should consult a gynecologist.
Pain after the procedure
Pain after hysteroscopy is considered absolutely normal if it is minor or moderate, localized in the lower abdomen or lower back/sacrum and lasts a couple of days. Painful sensations are explained, firstly, by the stretching of the uterine cavity during the procedure with gas or liquid, and secondly, by traumatization of the tissues of the cervix and uterus with instruments. Women with a low pain threshold complain of severe pain; in such cases, the doctor may recommend taking NSAIDs with a good analgesic effect (ketorol, indomethacin, Nise). But if the stomach hurts unbearably, the nature of the pain is cramping, dagger-like or shooting, the temperature rises significantly and the symptoms of intoxication increase, the pain radiates to the perineum or leg, then you must immediately seek medical help to eliminate possible complications.
General recommendations
In the early recovery period, it is necessary to strictly follow all the recommendations of the gynecologist:
- abstain from sexual activity for about 3–4 weeks (ideally, before your first period);
- It is prohibited to take a bath, visit a bathhouse and sauna, or swim in a pool or open water for at least 3 weeks;
- maintain personal hygiene (shower daily, wash twice a day using detergents with a pH-neutral reaction (intimate gels, baby soap);
- as a rule, the doctor prescribes anti-inflammatory treatment after hysteroscopy (prophylactically) with antibiotics (ciprofloxacin) and metronidazole for a course of 5–7 days;
- daily monitoring of body temperature (in the morning and before bedtime);
- stop taking aspirin as a pain reliever (the drug thins the blood, which will increase spotting and can cause bleeding);
- postpone intense physical activity, heavy physical labor and lifting weights of more than 3 kg for 1 - 1.5 months (health-improving sports exercises are allowed after 2 - 3 weeks);
- refusal of tampons during the period of bleeding, it is better to use pads;
- a ban on intravaginal administration of tablets, suppositories, gels and creams, as well as douching;
- after hysteroscopy, you should not use spermicides for a month;
- adhere to a balanced diet so as not to provoke constipation (refusal of spicy, salty, pickled foods, fried and fatty foods).
- Empty your bladder in a timely manner.
Diet - allowed and prohibited foods
In the vast majority of cases, the appearance of symptoms of thrush indicates the presence of serious problems in the patient’s body, the elimination of which requires the prescription of complex treatment. In addition to prescribing medications and taking measures aimed at restoring the normal immune status of the body, effective treatment of thrush is impossible without using an appropriate diet.
It must be remembered that yeast-like fungi of the genus Candida are opportunistic microorganisms that are always present on the skin and mucous membranes of the body. Their growth and excessive reproduction are controlled by normal microflora; accordingly, the symptoms of thrush clearly manifest themselves only when the composition of microorganisms changes and dysbacteriosis occurs.
Pregnancy after hysteroscopy
Most women who undergo a hysteroscopy procedure are concerned about when pregnancy will occur after it. If the procedure was performed for diagnostic purposes, and no surgical interventions were performed in the uterine cavity, for example, excision of a polyp, then conception is possible already in the next cycle. This is due to the rapid restoration of the uterine mucosa and hormonal levels. But doctors warn the patient that there is no need to rush, and when you can get pregnant depends on many other factors:
- the nature of the menstrual cycle (regular or not);
- the presence of other gynecological diseases (inflammation of the appendages, background processes of the cervix, external endometriosis and others);
- the presence of extragenital pathology (it is necessary to correct the condition and undergo treatment);
- preparation for pregnancy (healthy lifestyle, taking folic acid, moderate physical activity for at least 3 months);
- examination for sexually transmitted infections and treatment of both partners if they are detected (chlamydia, cytomegalovirus, human papillomavirus and others).
Antibiotics
Both after hysteroscopy and after histology of the uterus, at first the internal genital organs have an open wound. To protect against various infectious diseases and inflammatory processes, it is necessary to take antibiotics.
Many patients believe that infections enter the body during surgery. In fact, many specialists carefully monitor the sterility of the instruments and the room itself in which the procedure takes place. Therefore, the risk of getting an infection in the operating room is extremely low.
Most inflammatory processes are transferred from the patient’s own microflora. In the normal state, microbes located in the lower layers of the flora do not develop. Only when they are transferred from the vagina to the uterine cavity do they receive sufficient nutrition for further growth.
Taking penicillin drugs significantly reduces the likelihood of developing infections and inflammations. Thanks to well-chosen antibiotics, serious consequences can be avoided, and recovery occurs much faster.
If inflammatory processes have already appeared, antibiotics from the aminoglycoside group are prescribed in combination with antibacterial therapy.
Do not forget that long-term use of penicillin drugs has a negative effect on the intestinal microflora. Therefore, after completing a course of antibiotics, it is recommended to take probiotics.
For outpatient recovery, antibiotics should be taken for one week. In some cases, the deadline can be extended to two weeks.
Cost of hysteroscopy
The cost of hysteroscopy depends on the purpose for which it is performed. Diagnostic or office hysteroscopy, respectively, is cheaper since it does not include surgery. Prices for surgical hysteroscopy vary according to the level of complexity of the operation, the qualifications and experience of the doctor and the quality of the equipment. Increases the cost of the procedure and the need (in some cases) for hospital stay. But, of course, the price of the service depends on the region and the level of the clinic.
For example, in Moscow, diagnostic hysteroscopy will cost 15,000 - 35,000 rubles, and the price for an operating room reaches 60,000 - 65,000 rubles. In the provinces, the price of office hysteroscopy ranges from 2,500 to 9,000 rubles, and the procedure with surgical treatment of intrauterine pathology costs from 3,500 to 25,000 rubles. The average price for a hospital stay is 1,500 – 4,000 rubles.
Possible complications
Hysteroscopy, like any invasive procedure, is fraught with complications.
Early complications
Among the early postoperative complications, the following should be noted:
- inflammation of the uterus and peritoneum of the small pelvis (endometritis, pelvioperitonitis) – accounts for 90% of all complications;
- intravascular hemolysis caused by the duration of the operation and the use of distilled water or electrolyte-free media or increased intrauterine pressure;
- bleeding – no more than 5% of all complications (observed after resection of fibroids, resection or ablation of the endometrium).
Late complications
Late complications include:
- formation of pyometra in postmenopausal patients (in case of rough manipulation);
- formation of hydrosalpinxes, especially with chronic adnexitis;
- deformation of the uterine cavity (after resection of the endometrium or removal of large myomatous nodes);
- exacerbation of chronic inflammatory processes;
- incomplete removal of intrauterine formations.