Married couples who dream of children want them to be happy and healthy. Statistics, unfortunately, provide disappointing facts that a certain number of newborn babies have various pathologies that affect the quality of life not only of children, but also of their environment. Such cases are not isolated, and the reasons that lead to such undesirable results during pregnancy are explained by many circumstances. This includes the current state of the environment, the living and working conditions of parents, as well as the rhythm and way of life. The birth of children doomed to suffer can be prevented using intrauterine methods for determining abnormalities and the presence of various pathologies in fetal development.
One such method for determining abnormalities is alpha-fetoprotein testing. This test is recommended for every pregnant woman who wants to give birth to a healthy and strong baby. The examination is best carried out in the first trimester; 10, 11 and 12 obstetric weeks are considered optimal. The error of this type of testing is about 5 – 10%, subject to the rules for conducting the examination. However, the reliability of the results still needs to be confirmed, which is carried out using some additional analyzes. Only on the basis of a full and comprehensive examination can a final diagnosis be made and a decision on further action be made.
An AFP screening test is the initial step in the process of diagnosing fetal anomalies during pregnancy. It is premature to draw conclusions from one examination; a comprehensive, comprehensive examination is necessary.
Interpretation of the analysis and AFP norm
After taking the test, the result will be ready in two days, but if necessary, in emergency cases, it can be obtained after two hours. Often, in order to have reliable data, in the second trimester of pregnancy the analysis should be carried out in combination with ultrasound, testing for placental hormones and other diagnostic techniques.
Each laboratory uses its own methodology and reagents when analyzing the level of AFP content. But the units of measurement are designated the same in all cases: IU/ml or MoM. For example, if an AFP and hCG analysis is performed during pregnancy, the norm (MoM) is 0.5-2. However, if the laboratory uses other measurements (IU/ml), then the protein level, depending on the stage of pregnancy, will change as follows (see table below).
AFP norm depending on the stage of pregnancy
As mentioned above, in men the norm is no more than 10 IU/ml. The same applies to non-pregnant women.
What is MOM?
In serious, large laboratories, the analysis result is given not only in units per milliliter (IU/ml), but another, facilitating indicator is used. This is MoM - Multiple of Median, a multiple of the median.
How to calculate this value? To do this, the patient's alpha-fetoprotein concentration is divided by the average concentration that is normal for a given stage of pregnancy. Thus, the denominator is the median concentration. As a result, for each week of pregnancy there is a certain spread of values, but the norm in multiples of the median for any period should range from 0.5-2.0 MoM. Therefore, if a pregnant woman gets a result in any week, for example, 0.6 or 1.4, then this is the norm.
In specialized perinatal centers, as well as specialists in pregnancy pathology, there are special, corrected relative MoM units. They take into account not only the normal concentration of alpha-fetoprotein at different stages of pregnancy, but there are special adjustments for the pregnant woman’s body weight, age, the presence of risk factors and various diseases.
It must be remembered that if a pregnant woman takes monoclonal antibody drugs, this may also change the result and lead to unreliable indicators. Interestingly, in women of the Negroid race, the alpha-fetoprotein level at all stages of pregnancy is on average 15% higher than in white women, while in women of the Mongoloid race, on the contrary, the norm is lower. If a woman has type 1 diabetes, that is, insulin-dependent diabetes, then her alpha-fetoprotein concentration will be lower than that of a healthy pregnant woman at the same stage.
Under what conditions does alpha-fetoprotein change and when is it considered dangerous?
Decoding
The amount of alpha-fetoprotein in the blood may be higher or lower than normal. This shows that the fetus can have various pathologies.
Different norms of AFP during pregnancy are given in the MoM, which shows a specific value related to a certain period of pregnancy. Normal concentration is 0.6 – 2.4 MoM. If there is a deviation from the norm below or above the limit, then there is a possibility that the baby will not form correctly.
If you had AFP done during pregnancy, the rate is higher at times such as:
- carrying two or more babies;
- death of the baby's liver;
- neural tube defect (enlarged brain);
- umbilical hernia in a child;
- impaired kidney development;
- other fetal growth problems.
If AFP levels are low in a pregnant woman, the gynecologist may suspect problems such as:
- Down syndrome (after the eleventh week of conception);
- trisomy 18 pair of chromosomes;
- embryo death;
- unexpected pregnancy loss.
Also, a low protein concentration indicates an inaccurate determination of the date of conception, i.e., the actual conception occurred later.
In medicine, AFP analysis is considered the most important marker of genetic malfunctions in the chromosome itself and the normal development of the baby when carrying it.
Improper formation of the baby results in an increase in the AFP substance in the blood of a woman in labor, and different shifts in protein levels are most often closely intertwined with pathology in mothers.
This analysis should be done only in combination with an ultrasound, which will help remove from the list most of the defects and problems in the formation of your baby
It is also very important for a woman in labor to test for placental hormones and hCG. All these tests are called the “triple test” and help to approach the problem of identifying various syndromes and abnormalities in embryo development more responsibly
Most often, a woman gets a good response to an AFP test during pregnancy, but things can be different! If you receive a negative result, there is no need to panic. Firstly, the AFP test itself is not indicative and may not immediately indicate chromosomal abnormalities in the baby. Secondly, approximately 6% of all pregnant women do not get very good results, but 91% of them (according to statistics) give birth to healthy babies.
An increased protein level may indicate an incorrectly determined period of conception. After all the tests and ultrasounds have been completed, you may need to consult a geneticist. And after this, it is worth making a decision on immediate treatment of the fetus or on artificially interrupting its development.
According to reviews from pregnant women, most of them are satisfied with the AFP test and its result, because expectant mothers worry about the fitness and health of their babies. The analysis itself is not difficult to perform, and the price is also reasonable.
According to the recommendations of doctors, such an analysis should be carried out during pregnancy to diagnose the development of the unborn child. Since the analysis itself is not completely informative, if the result is negative, you will need to additionally perform an ultrasound and test placental hormones.
As expectant mothers say, many of them are dissuaded by friends and advice from forums on the Internet from carrying out such an analysis, but it is better to follow the recommendations of your gynecologist
The health of children, especially during their formation period, is very important
It is vital to carry out further treatment if the results are poor! Because the world and people need full-fledged, healthy heirs of future progress and life on planet Earth. Nobody wants to take responsibility for the lives of children with various syndromes and inhibition of fetal development. Therefore, carry out all the necessary manipulations in time for the future health of your child and his generation.
Health to you and your children!
Increased AFP concentration
- Often, excess of normal levels in pregnant women occurs more often than underestimated concentrations. Any deviation from normal indicators is fraught with the development of organ abnormalities of varying levels of severity in the child. To confirm the diagnosis, additional examinations are necessary.
- Developmental abnormalities can only be confirmed by a doctor after performing an ultrasound scan of the fetus. If suspicions remain after the ultrasound, to complete the picture, the level of human chorionic gonadotropin (hCG) in the blood is usually determined and an analysis of the amniotic fluid, called amniocentesis, is performed (the amniotic fluid is examined).
- List of reasons causing increased AFP during pregnancy:
- multiple births;
- viral infection that was transmitted to the child;
- large fruit;
- signs of fetal underdevelopment;
- the presence of an umbilical hernia in the fetus;
- gastroschisis (expressed as non-fusion of the abdominal wall);
- abnormal development of the child’s kidneys and urinary system (the fetus does not have one or both kidneys, polycystic kidney disease, incomplete process of formation of these organs);
- pathology of fetal brain development (the neural tube has developmental defects, absence of the brain or part of it, and other abnormalities);
- pathology of the development of the digestive organs (intestines or esophagus with a closed end or shortened, abnormalities in the development of the stomach);
- hydrocephalus;
- hydatidiform mole;
- chromosome pathology (signs of Down, Patau or Edwards syndrome);
- development of diabetes mellitus or hypertension in a pregnant woman;
- obesity during high-grade pregnancy;
- severe form of gestosis (late toxicosis);
- signs of threat of spontaneous abortion.
- The vast majority of the listed abnormal changes in the fetus are very severe pathologies leading to the non-viability of the unborn child. These forms of abnormalities are caused by an increase in the level of intrauterine protein.
- Minor deviations can be ignored; most often they are caused by inaccuracies in determining the number of complete obstetric weeks. In such a situation, nothing needs to be done. And if the indicators differ significantly from the norm, a clarifying ultrasound examination of the fetus and analysis of amniotic fluid should be carried out. When the diagnosis of a pregnant woman is confirmed, it is recommended to perform an artificial birth.
Negative test result for AFP protein concentration during pregnancy
International statistics indicate that in 5% of pregnant women, the analysis of AFP content has deviations in one direction or the other from the established norm. However, 90% of these women subsequently safely gave birth to absolutely healthy babies. It should be firmly understood that based only on the results of the analysis of AFP content, it is impossible to establish a final and accurate diagnosis. This analysis is carried out to identify abnormal development of the unborn child. A separate analysis for the concentration of alpha-fetoprotein protein is not able to provide complete and guaranteed accuracy of the results. To obtain the most objective information about the course of pregnancy, this analysis is recommended to be carried out in combination. To get a complete picture, you should undergo tests that determine the level of hCG, the level of free esthiol, as well as ultrasound.
The attending physician will accurately determine the most appropriate time for taking these tests, as well as determine their necessity. Blood is taken to determine the concentration of alpha-fetoprotein in it only from a vein. The procedure must be carried out on an empty stomach, between eating (even a light breakfast) and taking blood for this analysis, the time interval should be more than 4 hours. Therefore, the best time to conduct it is in the morning before breakfast.
In case of an unsatisfactory result, if it shows even minor deviations from the upper or lower norm, the attending physician is obliged to prescribe a repeat blood test. In addition, a pregnant woman must undergo a more detailed and complex ultrasound. To obtain the most accurate and detailed result, you will need to take an amniotic fluid test. Consultation and observation with a geneticist will also not be superfluous in case of unfavorable results of AFP tests.
https://youtube.com/watch?v=Tvl3dzY6oF8
Based on materials from nedeli-beremennosti.com
Reduced AFP concentration
- A decrease in AFP levels is much less common; such a deviation from normal values also indicates an anomaly in the development of the child’s body.
- Reasons causing a decrease in AFP concentration:
- the threat of miscarriage in the first third of the pregnancy process, and the threat of having a child born prematurely - from the 16th week;
- hydatidiform mole;
- the presence of intrauterine anomalies of fetal development;
- fetal freezing (intrauterine);
- chromosomal pathologies (Down, Patau or Edwards syndromes).
- Detection of a sharp drop in AFP concentration, confirmed by additional examinations, requires urgent intervention and comprehensive treatment aimed at maintaining pregnancy, or making a decision on the need for immediate artificial resolution of pregnancy.
- An unfavorable AFP test is not a death sentence. Only 5% of women in this case actually have serious problems with the development of the child in the womb. Almost 90% of the examined expectant mothers subsequently give birth to completely healthy children.
- An exceptionally unfavorable AFP test result is not sufficient for a definitive diagnosis. It is only a kind of signal that determines the possibility of risk. In this case, it is necessary to consult a specialist who will correctly interpret the test results and decide on further actions.
It is difficult to overestimate the importance of a pregnant woman undergoing a timely AFP examination. The results of the analysis can determine the future fate of the pregnancy. Do not expose yourself and your unborn child to the risk of irreparable situations. A timely examination will protect your child from an unfulfilling life and can prevent a tragedy in the family. An unfortunate combination of circumstances can have a detrimental effect on such a pregnancy, but this does not mean that you cannot have completely healthy and full-fledged children.
Treatment of hypertension during pregnancy
During pregnancy, hypertension is treated. The main treatment method is the use of antihypertensive drugs. The use of a number of them is limited due to adverse effects on the fetus; therefore, currently developed effective antihypertensive treatment regimens cannot always be used in pregnant women. Non-drug therapy (sedative physiotherapy, herbal medicine, nutritional adjustments, limiting the intake of table salt - less than 6 g per day) is of particular importance in pregnant women.
Medications used in pregnant women include diuretics, antispasmodics, calcium ion antagonists, adrenergic receptor stimulants, vasodilators, and ganglion blockers.
Among diuretics, preference should be given to potassium-sparing drugs: triamterene, spironolactone or the thiazide diuretic indapamide, which has a natriuretic effect and promotes peripheral vasodilation without reducing cardiac output and heart rate. Diuretics are used in courses of 1-3 days every 7-10 days.
According to modern concepts, antispasmodics (dibazole, papaverine, no-spa, aminophylline) provide a weak hypotensive effect compared to other newly proposed drugs. However, due to the lack of negative effects of antispasmodics on the fetus, they are indispensable for pregnant women. At the same time, antispasmodics work better when administered parenterally, especially when stopping hypertensive crises.
Currently, calcium ion antagonists of the dihydropyridine series are increasingly used as first-stage drugs. From this group of drugs during pregnancy, it is advisable to use second-generation drugs (Norvax, Lomir, Foridon), which have a highly specific effect, are characterized by a long half-life and a very small number of side effects. The first generation calcium ion antagonist nifedipine is contraindicated during pregnancy.
Adrenergic receptor stimulants (clonidine, methyldopa) are widely used during pregnancy due to their effectiveness and the absence of negative effects on the fetus.
Of the vasodilators during pregnancy, hydralazine (apressin) is most often used for hypertensive crisis or for diastolic pressure above 100-110 mm Hg.
Ganglion blockers (pentamine, benzohexonium) have side effects, affect intestinal function in the fetus and can cause intestinal obstruction in the newborn. These drugs are used only during labor to achieve a rapid, short-term reduction in blood pressure.
Treatment of hypertension in pregnant women follows the same principles as in non-pregnant women. In stage I hypertension, monotherapy is often used; in stage II, combinations of two or three antihypertensive drugs with different mechanisms of action are prescribed. At the same time, measures are taken to normalize microcirculation and prevent placental insufficiency. If gestosis or placental insufficiency develops against the background of hypertension, the entire treatment complex used for these complications of pregnancy is prescribed.
Delivery in women with hypertension is most often carried out through the vaginal birth canal against the background of anesthesia and antihypertensive therapy. Caesarean section is performed for obstetric indications or for conditions that threaten the health and life of the mother (retinal detachment, cerebrovascular accident, etc.).
Ed. G. Savelyeva
“Treatment of hypertension (hypertension) during pregnancy” - article from the Pregnancy section
Interpretation of results
Despite the early appearance of fetoprotein in the blood of the fetus, in a pregnant woman the protein begins to increase from the 10th week. In the serum of a child during intrauterine development, AFP increases at 12-16 weeks of development, remains at this level for a long time and begins to decrease at the end of the 2nd trimester. By the time of birth, it is already insufficient, and during the first year of life it reaches the level of an adult.
During pregnancy, the concentration of protein in the mother's blood differs from that in the child's blood. It begins to increase from the 10th week, and the maximum is reached only at 32-34 weeks of gestation. The optimal period for screening is 15-20 weeks. This time was chosen for the examination so that if developmental abnormalities are detected, treatment can be carried out. In severe cases, when, in addition to chromosomal abnormalities, severe malformations are determined, the woman is offered to terminate the pregnancy for medical reasons, which is allowed to be done up to 22 weeks.
The AFP norm by week of pregnancy changes as follows:
When dynamically assessing the level of AFP, if the analysis was carried out several times, attention is paid not only to absolute numbers, but also to the rate of their growth. After minimum values at week 10, AFP increases by 15% every 7 days until week 25. When studying the relationship with albumin, the concentration of alpha-fetoprotein reaches 10%.
AFP results are not considered separately from other indicators of the triple test or extended study. This can lead to incorrect diagnosis of pathology and the choice of incorrect pregnancy management tactics. Testing is aimed at identifying the following complications and defects:
- cleft neural tube;
- chromosomal abnormalities, more often Down syndrome and Shereshevsky-Turner syndrome;
- some congenital malformations of the digestive tract and kidneys;
- placental insufficiency;
- hemolytic disease of the fetus in late stages.
The analysis cannot determine such defects as hypospadias, cryptorchidism and hydrocele.
Why is the rate increased?
Fetal neural tube defects
High AFP during pregnancy suggests this pathology. The most common diagnosis is spina bifida, which is incomplete closure of the spinal canal. In this case, the meninges protrude and form a hernia. A congenital anomaly does not always lead to the death of a child, but it can cause disability and requires neurosurgical care immediately after birth.
Anencephaly - absence of the brain
If the diagnosis is confirmed by additional research, the fetus is considered nonviable, and the woman is advised to terminate the gestation. Neural tube defects are characterized by an increase in fetoprotein several times compared to the norm. This is due to the leakage of protein through defects in the spinal column directly into the amniotic fluid and further into the mother’s bloodstream.
Indicators are increased when:
- detection of increased echogenicity of the intestine on ultrasound, which cannot be associated with other diseases;
- Shereshevsky-Turner syndrome;
- pregnancy with twins - the concentration naturally increases by 2 times, but it cannot be used to judge the pathology or normal development of the fetus;
- possible Rh conflict between mother and fetus in the 2nd and 3rd trimester;
- severe form of hemolytic disease and intrauterine fetal death;
- lysis of liver cells and release of protein into the bloodstream (with necrosis of the fetal liver caused by a viral infection, an increase in concentration also occurs);
- in complicated pregnancy, in women with severe toxicosis in the 1st trimester, an increase in AFP concentration is associated with the characteristics of protein synthesis in the liver;
- the threat of miscarriage due to an increase in blood pressure in the fetal vessels, so the protein enters the mother’s bloodstream more actively.
A false increase in fetoprotein is associated with systemic pathologies of the mother: systemic lupus erythematosus, dermatitis or acute eczema.
Fetoprotein increases 3 times or more with the following anomalies:
- atresia of the esophagus or duodenum;
- defects of the anterior abdominal wall;
- omphalocele;
- congenital nephrosis;
- polycystic kidney disease;
- renal agenesis;
- epidermolysis bullosa involving the mucous membrane of the digestive tract.
But even in the absence of confirmation of malformations, pregnant women who experienced an increase in AFP at 15-20 weeks are at risk for the development of placental insufficiency and fetal malnutrition.
Causes of decreased alpha-fetoprotein
Down syndrome
Most often, a decrease in AFP is associated with Down syndrome. This is a genomic pathology in which instead of 46 chromosomes the fetus has 47. Analysis for fetoprotein is assessed in conjunction with ultrasound data at 10-12 weeks, the results of which may indicate an increase in the thickness of the cervical fold or abnormalities in the development of the nasal bone.
A low AFP confirms a high risk of Down syndrome in the fetus, but does not provide a 100% guarantee of the development of the disease. Sometimes there are false results in which children are born with a normal set of chromosomes. Therefore, after analysis, additional diagnostics are required. The score for a positive test may be as follows:
- triple test – risk 1:25;
- quadrotest – risk 1:13;
- integrated test – risk 1:3.
Edwards syndrome
Low AFP is observed with division of chromosome 18, or Edwards syndrome. This is a chromosomal pathology with severe developmental defects. Children are born with facial abnormalities, irregular skull shape and low weight. Multiple malformations of large vessels, heart and other organs are observed, which makes newborns non-viable.
Hydatidiform mole
This is an anomaly in which the embryo does not develop, and the chorionic villi form growths in the form of bubbles. A woman may feel all the symptoms of pregnancy, but if she is not registered and the first examination was carried out after 12 weeks, then there is a risk of complications in the form of increased blood pressure and the development of gestosis, proteinuria, and in severe cases, metastases to other organs.
Read more about pathology at the link.
If the gestational age is incorrectly determined, the AFP will be relatively low if the gestational age is overestimated. Therefore, it is important for women to know the day of their last menstruation when registering.
ENAP - use during pregnancy and lactation
The use of Enap, like other ACE inhibitors, is not recommended in the first trimester of pregnancy. The use of ACE inhibitors, incl. Enap is contraindicated in the second and third trimesters of pregnancy.
Epidemiological data on the risk of teratogenic effects of ACE inhibitors during pregnancy do not allow us to draw definitive conclusions. However, the possibility of teratogenic effects cannot be excluded. If it is necessary to use ACE inhibitors, the patient must be transferred to therapy with another antihypertensive drug with a proven safety profile for pregnant women.
If pregnancy is confirmed, Enap should be discontinued as soon as possible.
Taking ACE inhibitors in the second and third trimesters of pregnancy can cause fetotoxic effects (impaired renal function, oligohydramnios, delayed ossification of the skull bones) and neonatal toxic effects (renal failure, arterial hypotension, hyperkalemia).
If the patient took an ACE inhibitor in the second and third trimesters of pregnancy, it is recommended to perform an ultrasound scan of the fetal kidneys and skull bones.
In those rare cases where the use of an ACE inhibitor during pregnancy is considered necessary, periodic ultrasound should be performed to assess the amniotic fluid index. If oligohydramnios is detected during ultrasound, it is necessary to stop taking the drug. Patients and physicians should be aware that oligohydramnios occurs when there is irreversible damage to the fetus. If ACE inhibitors are used during pregnancy and the development of oligohydramnios is observed, then, depending on the stage of pregnancy, a stress test, a non-stress test or a fetal biophysical profile may be required to assess the functional status of the fetus.
Newborns whose mothers took ACE inhibitors during pregnancy should be monitored due to possible hypotension. Enalapril, which crosses the placenta, can be partially removed from the neonatal circulation by peritoneal dialysis, and theoretically it can be removed by exchange transfusion.
Enalapril and enaprilat are detected in breast milk in trace concentrations, therefore, if it is necessary to use the drug Enap during lactation, breastfeeding should be discontinued.
Norms and reduced results
The norms of alpha-fetoprotein in the blood during pregnancy are presented in the table:
| Gestation period in weeks | Protein concentration level in units/ml |
| First trimester up to twelve weeks | Up to 15 |
| 13-15 | 15-60 |
| 15-19 | 16-95 |
| 20-24 | 27-125 |
| 25-27 | 52-140 |
| 28-30 | 67-150 |
| 31-33 | 100-250 |
| C 33 | There is a gradual decline |
A decreased AFP may indicate the following chromosomal abnormalities.
Down syndrome
Low alpha-fetoprotein often indicates Down syndrome. This chromosomal pathology is characterized by the presence of one extra chromosome 47. The study material is analyzed together with data obtained from an ultrasound examination of the fetus. According to the results of ultrasound in such a situation, an abnormal structure of the collar fold or nasal bone is usually observed.
Edwards syndrome
Decreased fetoprotein levels may indicate Edwards syndrome. The pathology is characterized by serious chromosomal abnormalities. Children are born with abnormalities in the structure of the skull and low weight.
A large number of defects of large blood vessels and heart muscle are diagnosed. Because of this, newborns are initially born non-viable.
Hydatidiform mole
In this case, the fetus lags behind in development or does not develop at all, and the chorionic villi form formations in the form of bubbles. The girl feels signs of pregnancy.
There is a risk of increased blood pressure and the formation of toxicosis, and then gestosis. Organ metastases rarely develop.
Analysis of AFP during pregnancy and its norms by week
Not every expectant mother knows exactly what tests she undergoes as directed by a doctor while carrying a child. Yes, this is not always required. However, AFP testing is well known among pregnant women. What kind of study this is, what it says and what are the normative values of AFP during pregnancy, we will tell you in this article.
The abbreviation AFP stands for alpha-fetoprotein. This protein is formed in the maternal body during the development of the embryo and fetus. The substance was initially discovered as a marker for cancerous tumors, and only in the second half of the twentieth century did doctors and scientists notice a pattern - the protein appears in the blood of pregnant women who do not have any malignant tumors.
Alpha-fetoprotein is very similar to another protein, serum albumin.
In adults, it transports various low molecular weight substances into tissues. In a baby that develops in the mother's womb, AFP replaces albumin and performs its functions - it transports substances necessary for growth and development through all tissues with the blood.
All the functions of this amazing protein are not yet known to science. Therefore, in encyclopedias and scientific reference books there is the wording “probable functions”, “possible and hypothetical functions”.
Such probable functions of AFP include an immunosuppressive effect - the protein, through unknown mechanisms, affects a woman’s immunity, suppressing its activity and possible rejection of the fetus, which is only half “native” to her. AFP is also “suspected” of suppressing the fetal immunity. Otherwise, the baby could react negatively to the new compounds and proteins that it receives from the mother’s blood.
Early in pregnancy, the protein AFP is produced by the corpus luteum. However, already three weeks after conception, the baby embryo begins to produce the necessary protein compound on its own. The substance enters the amniotic fluid with the baby’s urine, and from there into the mother’s bloodstream to be excreted.
The amount of AFP gradually increases, and from 11-12 weeks it is well determined in the woman’s blood.
By 16-17 weeks, the concentration of the substance rises significantly.
The highest level of AFP in a woman’s blood is observed at 33-34 weeks, after which the amount of embryonic (fetal) protein begins to slowly decrease.
Protein has found wide use in the treatment of many diseases, including cancer. It is obtained from placental and abortion blood. During pregnancy, the level of AFP may indicate possible complications and genetic pathologies of the fetus.
The alpha-fetoprotein test is also called the Tatarinov-Abelev test. It is part of the so-called “triple test”, which is prescribed to all pregnant women as part of the second prenatal screening.
The best time for analysis is considered to be 16-17-18 weeks of pregnancy, since during this period the protein is well detected in a woman’s blood and has a reliable diagnostic value.
A fetus that has chromosomal abnormalities (Down syndrome, Turner syndrome, Patau syndrome and others, non-molar trisomies, as well as malformations of the neural tube - the brain and spinal cord) produces certain amounts of this protein.
Based on the level of AFP, one can indirectly judge a possible deviation in the development of the child.
To make the picture more complete, the concentration of fetal protein is compared with the level of hCG (chorionic gonadotropin hormone), as well as the level of free estriol.
Some clinics also determine the level of inhibin, a placental hormone, and then the analysis is called the “quadruple test.” The laboratory picture is complemented by ultrasound, which is mandatory as part of the screening examination.
Blood for analysis is taken from a vein. A woman should come to the laboratory or treatment room on an empty stomach, in the morning, having first stopped taking all hormonal drugs and antibiotics, if any were prescribed to her by the doctor.
A few days before donating blood for analysis, a pregnant woman should avoid eating fatty and sweet foods, large amounts of salt, carbonated drinks, and coffee. If the expectant mother smokes, despite the obvious harm of this habit, she should refrain from smoking for 3-4 hours before donating blood.
A nervous factor can also affect the results of the analysis, so the woman is advised not to be nervous.
The level of fetal AFP protein increases with the duration of pregnancy, this is easy to understand from the table:
Obstetric term
AFP concentration (in U/ml)
Preparation for research and collection of material
The doctor warns the pregnant woman in advance about the need to conduct an AFP test. The referral is given a few days before the expected date of the examination. If an ultrasound and PAPP-A analysis were performed at 10-13 weeks, then 3 weeks are counted from the date of the study and the appropriate day is determined.
How to prepare for an AFP test?
For research, venous blood is taken from the elbow. The test is taken in the morning strictly on an empty stomach. The concentration of proteins and the result can be affected by food intake or drinks, so you should not eat or drink tea, coffee or juices. But clean water is allowed. The last meal should be at least 8 hours ago.
There is no need to follow a special diet before the test, but fatty, spicy foods are not recommended in the evening. There are no restrictions on taking medications; they do not affect the results of the studies. If you need to take pills in the morning, do this after donating blood.
Before the treatment room, you need to calm down and not be nervous; it is believed that stress factors can cause biochemical changes and affect the result.
How long will it take for the analysis to be ready?
It all depends on the characteristics of the laboratory. In large research centers this requires 1 day. If the clinic does not have its own laboratory, and tests are performed in other medical centers under a contract, the results are ready in 1-2 days.
Analysis of AFP alpha-fetoprotein during pregnancy is normal in the blood
Alpha fetoprotein (AFP, AFP, α-fetoprotein) is a protein that is produced by the yolk sac and then in the liver and gastrointestinal tract of the embryo. AFP analysis during pregnancy is used to diagnose congenital malformations of the fetus. In most cases, changes in AFP are associated with the presence of obstetric pathology in the mother. In oncology - Alpha-fetoprotein is a marker of primary liver cancer.
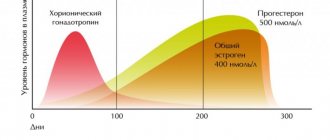
During pregnancy, α-fetoprotein penetrates from the fetus into the mother's blood from the sixth week of pregnancy and increases progressively, reaching a maximum at 32–33 weeks of pregnancy.
Pregnant women donate blood for AFP analysis at the beginning of the second trimester at 16-20 weeks (optimally 16-18 weeks) along with hCG analysis to screen for congenital malformations of the fetus.
The most accurate results can be obtained when blood testing is done between the 16th and 18th weeks of pregnancy; research before the 14th or after the 21st week does not provide accurate results.
The protein Alpha-fetoprotein is named from “fetus” (“fruit”) - fetal protein. AFP almost completely disappears from the blood within a year after a person is born. At the age of 1 year, the normal serum AFP level is the same as in adults, that is, less than 15 ng/ml. However, the protein appears in the blood of adults during the development of liver cancer and some tumors of the reproductive system.
In pregnant women, Alpha-fetoprotein is directly related to many processes occurring in a woman’s body. AFP protects the fetus from immune rejection by the mother's body.
The level of Alpha-fetoprotein is interrelated with gestational age, fetal weight, reflecting the degree of intrauterine maturation of the fetus and maturity at birth.
The normal level during pregnancy is considered to be an AFP level of 0.5 to 2.0 MoM. Therefore, if the conclusion states that the AFP level is 0.2, then we are talking about a reduced protein concentration, and if the Alpha-fetoprotein value exceeds 2 MoM, then we are talking about an increased protein level.
In the blood of women pregnant with a fetus with Down syndrome, the average level of AFP in the second trimester is reduced, and the level of hCG is increased. Based on this, a study of the serum of pregnant women for AFP and hCG is used as a method of mass prenatal examination of mothers, with the help of which it is possible to form a high-risk group among women for the presence of central nervous system malformations in the fetus (anencephaly, encephalocele, spina bifida) or Down syndrome.
What is alpha fetoprotein
- Alpha-fetoprotein is a special kind of protein that begins to be produced immediately after conception. The enzyme is initially produced by the mother's body, in particular by the corpus luteum of the ovaries. Then the formed embryo begins to produce it using the yolk sac of the embryo, and finally, as the fetus develops, the protein is synthesized by its liver cells.
- Alpha-fetoprotein, and in particular its certain concentration, plays a decisive role in the full development of the child in the womb and performs a number of important tasks. This:
- transfer of the constituent elements of maternal blood, which is performed by transport proteins that are also involved in the construction of the baby’s body, ensuring its growth and development;
- transportation of polyunsaturated fatty acids, which ensure the production of cell membranes of the fetus, and before birth, literally a month before their resolution, these cells participate in the production of surfactant (a substance that envelops the alveoli in the lungs), which ensure the independent breathing of the newborn baby;
- blocking the effect of the maternal hormone estrogen on the growing body of the unborn child;
- an obstacle to the influence of the immune system of the expectant mother, which tries to reject the embryo, perceiving it as a foreign body (reduces the formation of the woman’s immune cells that affect the developing fetus, which allows it to be carried to term and spontaneously rejected).
- AFP in the urine of the fetus is excreted into the amniotic fluid, and thus is absorbed into the blood of the pregnant woman. Some of the protein enters the mother's circulatory system through the placenta.
- In non-pregnant women, this type of protein is formed only when tumors occur. By the way, the same applies to male representatives. The synthesis of this complex biological substance in this case is provoked by the growth of cancer cells of the liver, testicles in men or ovaries in women. The test results confirm the presence of such a pathology in approximately 4–5% of such subjects.
- During pregnancy, an AFP examination helps monitor the development of the unborn child. Usually a normal pregnancy is confirmed by the results of an examination carried out in the second trimester. At a later stage, approximately at 32–34 obstetric weeks, AFP levels should normally increase to peak values, while closer to the resolution of labor they should gradually decrease. In a one-year-old child, AFP indicators do not differ from those of an adult.
- By week 12, the baby’s liver is able to independently synthesize AFP, supplying it to the circulatory system. The study of the mother's blood serum during this period allows us to monitor the state of intrauterine development of her unborn child.
What if the person is not pregnant?
It was stated above that in healthy adults and non-pregnant women, the content of alpha-fetoprotein in the blood is extremely low. In some cases, if liver disease exists, its concentration may increase. But in significant quantities it is found in liver tumors, in malignant neoplasms of the gonads, and in the diagnosis of metastases of various neoplasms in the liver tissue.
In the case of primary liver cancer not associated with metastases, the diagnostic value and interpretation of an increase in the level of this protein is very great. It is a tumor marker and appears in the peripheral blood much earlier than the first clinical signs of the disease that worry the patient. On average, alpha-fetoprotein in patients with primary hepatocellular carcinoma rises 2 months before pain, jaundice and other signs occur. This is important for timely diagnosis and treatment, and also gives a better chance of survival. But high levels of alpha-fetoprotein, as a tumor marker in adults, are described in detail in the article Alpha-fetoprotein (AFP) - a tumor marker.
Methods for studying AFP in the blood of a pregnant woman
Initially, after the discovery of fetoprotein, it was determined in the blood using paper electrophoresis, but currently an enzyme-linked immunosorbent assay (ELISA) is used. It is based on the ability of a protein acting as an antigen to bind to antibodies that contain an enzyme tag.
If the protein is present in the serum, the reaction will be positive. A special apparatus is used to determine the degree of serum dilution and the concentration of AFP in it. This is an important indicator that is relied upon when making a diagnosis. An alternative research method that can be used in some clinics is chemiluminescence.
ELISA is an immunochemical method that can give a false-positive result. The risk of incorrect analysis occurs when women have a large number of proteins similar in structure, as well as a large amount of immunoglobulin M. This is observed in pregnant women with elevated rheumatoid factor, autoimmune diseases, when using certain medications and systemic pathologies.
How to get tested for hCG
For maximum accuracy and reliability of analysis results, you must follow some rules
The doctor should inform you about the preparation, but it is important to remember that the hCG hormone test during pregnancy must be taken on an empty stomach. It is also recommended to do this in the morning; other times of day are acceptable, provided that nothing has been eaten before for at least 5 hours.
Blood for this test is taken from a vein. The day before donating blood, you should avoid any physical activity, since this is the only way the result will be reliable.
It is equally important to remember that if a woman took a course of hormonal drugs before taking the test, they will certainly affect its results, so there is a need to inform the laboratory employee about this
You should donate blood to test for hCG levels no earlier than two days after your period is missed or on the 12th day after the expected conception. At the same time, the presence of the hormone human chorionic gonadotropin in the blood can be noted a week after conception, but in this case, the accuracy of the analysis will be low. In order to track the dynamics of hCG growth, it is necessary to donate blood three times, the difference should be at least 2 days and, it is recommended, at the same time. To identify fetal pathologies, tests for human chorionic gonadotropin should be taken from 14 to 18 weeks of pregnancy.
HCG levels during pregnancy are one of the most important indicators, indicating, among other things, the normal course of pregnancy; it also contributes to the diagnosis of a variety of pregnancy disorders, even in the early stages of their development.
One way or another, if the result of the analysis for the content of human chorionic gonadotropin is alarming, do not panic and draw far-reaching conclusions - only a qualified doctor can reliably interpret the indicators, who will explain further actions and, perhaps, recommend taking the test again.
Alternative diagnostic methods
The principle of determining the degree of hCG concentration in the body is also included in the rapid diagnosis of pregnancy, in other words, in home pregnancy tests. The difference in this case will be that there is no need to donate blood, since urine will be diagnosed. Any modern tests are sufficiently sensitive and informative, starting from the first days of a missed period. At the same time, their diagnostic value is certainly somewhat lower than that of the same laboratory blood tests. Also, these methods are carried out for completely different purposes, so they can only complement each other and not replace.
The combination of methods should follow the following tactics: to confirm the presence of pregnancy, diagnosis begins with the use of a conventional rapid test, and then a laboratory one. It is also necessary to donate blood in cases where the test result is positive and there are signs of pregnancy disorders, or there is a suspicion of an ectopic pregnancy. It is possible, but not rational, to start diagnosing pregnancy by donating blood for analysis.
Blood test for progesterone to determine pregnancy
There are cases when, in addition to determining the level of human chorionic gonadotropin, doctors recommend donating blood to test for progesterone content. Progesterone is another pregnancy hormone; by its content, doctors determine how successful its development is.
It is generally accepted among most doctors that a progesterone level in early pregnancy above 25 ng/ml is evidence that the pregnancy is developing within normal limits. If the level of this hormone during pregnancy does not exceed 5 ng/ml, then this significantly reduces the chances of a successful pregnancy. An intermediate value of 5 to 25 ng/ml will require repeated measurement after some time.
How to pass the test correctly?
In order to avoid any random deviations in the test results, approximately two weeks before donating blood, that is, approximately at the 15th week of pregnancy, it is necessary to minimize the use of any medications, if possible. The fact is that some medications can distort the results of an alpha-fetoprotein test. Of course, pregnant women already try to take only those medications that are vital, and their prescription is strictly controlled.
The day before donating blood, it is necessary to limit spicy, salty, fatty and fried foods in your diet. Typically, the diet of pregnant women is balanced, and the very abuse of such products can lead to allergization of the baby, as well as metabolic disorders in the expectant mother and child, so this advice is also required to be followed at any stage of pregnancy.
It is also necessary to limit physical activity during the day, even if it is small, and the last meal should be no later than 20:00 in the evening on the eve of the morning blood donation. In the morning, after waking up, you can calmly drink a small amount of clean water, and then donate blood on an empty stomach. It is important that the visit to the laboratory should be early enough, since a later visit may distort the true concentration of alpha-fetoprotein in the blood plasma.
When is AFP determined during pregnancy?
The main indicators for determining AFP in the plasma of pregnant women are screening studies in women at risk, as well as suspicions of various prenatal pathologies in the fetus - chromosomal abnormalities, problems with fetal development, organ defects identified by ultrasound and other diagnostic procedures. Also, during pregnancy, tests to detect the level of AFP will be indicated as screening during the period when its level increases most actively - this is the period from the 15th to the 22nd week . If a woman underwent various types of invasive procedures in the initial stages of gestation (chorionic villus biopsy or amniocentesis), further monitoring of the AFP level over time is necessary.
There are a number of absolute indications for determining AFP in women during gestation. This may include reasons such as:
- Presence of a closely related marriage (spouses are cousins or other close relatives)
- there are genetically determined pathologies, chromosomal disorders, gene diseases, hereditary changes in metabolism in the family or in close relatives
- there are children in the family who were born earlier and have genetic or chromosomal pathologies
- pregnancy occurred after 35 years of age, or this is the first pregnancy after 30 years of age
- in the early stages of pregnancy, serious illnesses and infections were suffered, for which serious and potentially toxic drugs were taken
- the woman underwent early X-ray examinations.
For special indications, the doctor may prescribe an additional test if he considers it necessary.
Screening for the second trimester of pregnancy: transcript | My Gynecologist
Second trimester screening is a logical continuation of first trimester screening. This test helps identify the risk of having a baby with developmental abnormalities such as Down syndrome, anencephaly, spina bifida and others.
When is screening done?
Second trimester screening is performed between 14 and 20 weeks of pregnancy (it is best to screen at 16 to 18 weeks of pregnancy).
What tests are done in the 2nd trimester?
In the second trimester, you will take a biochemical blood test to determine the level of:
- hCG
- AFP
- Free estriol
- Inhibina A
At this stage, ultrasound data performed in the first trimester of pregnancy are also taken into account.
What are double, triple and quadruple tests?
Unfortunately, not all clinics and laboratories have the opportunity to determine the level of all 4 indicators at once. If only the level of hCG and AFP is measured in the second trimester screening, then this is a double test of the second trimester. The triple test is the determination of hCG, AFP and free estriol. The quadruple test is the determination of hCG, AFP, free estriol and inhibin A.
All of these tests can be considered in conjunction with first trimester ultrasound findings. This test is called combined.
HCG norm
The norm for hCG depends on the stage of pregnancy. You can find the rules for your term here.
Attention! HCG levels may vary from laboratory to laboratory, so the data provided is not conclusive and you should always consult your doctor. If the result is indicated in the MoM, then the standards are the same for all laboratories and for all analyses: from 0.5 to 2 MoM.
HCG: what if it is not normal?
If the hCG level is higher than normal for your stage of pregnancy, or exceeds 2 MoM, then the baby has an increased risk of Down syndrome and Klinefelter syndrome.
If hCG is below normal for your term, or less than 0.5 MoM, then the baby has an increased risk of Edwards syndrome.
AFP norm
AFP, or alpha fetoprotein, is a protein that is found in the blood of all pregnant women. AFP levels gradually increase from 14 weeks of pregnancy, and rise until 32-34 weeks, and then begin to decrease.
The norm for AFP depends on the stage of pregnancy:
- 13-15 weeks: 15-60 U/ml, or from 0.5 to 2 MoM
- 15-19 weeks: 15-95 U/ml, or 0.5 to 2 MoM
- 20-24 weeks: 27-125 U/ml, or from 0.5 to 2 MoM
Attention! The norms in U/ml may differ in different laboratories, so the data provided is not final, and in any case you should consult your doctor. If the result is indicated in the MoM, then the standards are the same for all laboratories and for all analyses: from 0.5 to 2 MoM.
AFP: What if he's not normal?
If AFP is higher than normal for your age, or exceeds 2 MoM, then your baby has an increased risk of developmental disorders of the spinal cord and brain (anencephaly and spina bifida). Elevated AFP levels also occur in multiple pregnancies.
If AFP is below normal for your age, or is less than 0.5 MoM, then the child has an increased risk of Down syndrome and Edwards syndrome.
Free estriol rate
Free estriol is a substance that is found in the blood of pregnant women and is an indicator of the well-being of her unborn child. The level of free estriol depends on how well the fetal adrenal glands are working.
The level of free estriol in the blood greatly depends on the laboratory in which you take the test. In this article I will not give standards for estriol, since they are too different for different laboratories and this can only mislead you.
Attention: when taking a blood test in the laboratory, always ask for the norm for each indicator. The laboratory is required to provide such information.
If the analysis result is given in MoM units, then the norm of free estriol for any stage of pregnancy is from 0.5 to 2 MoM.
Free estriol: what if it's not normal?
Some medications taken during pregnancy can affect the level of free estriol in the blood: Dexamethasone, Prednisolone, Metypred, antibiotics. If you are taking any medication, be sure to indicate this in the questionnaire that you will fill out before taking the test, or tell the specialist who takes your blood for analysis.
If your level of free estriol is below normal for your stage of pregnancy, or less than 0.5 MoM, then the unborn child has an increased risk of Down syndrome and Edwards syndrome. Reduced estriol may indicate feto-placental insufficiency, underdevelopment of the adrenal glands in the unborn child, the threat of premature birth and the absence of the brain (anencephaly) in the fetus.
Elevated estriol (more than 2 MoM) occurs in multiple pregnancies, liver diseases and large fetuses.
Norm Inhibin A
Inhibin A is a substance that is present in the blood both during pregnancy and in non-pregnant women. The norm for inhibin A may differ in different laboratories, so pay attention to the analysis result indicated in the MoM. The normal level of inhibin A should not exceed 2 MoM.
Inhibin A: What if it's not normal?
Increased levels of inhibin A are associated with an increased risk of Down syndrome in the unborn child. High inhibin A also occurs with other chromosomal abnormalities in the fetus.
And yet, many cases have been described where the level of inhibin A during pregnancy was increased several times, but other tests were normal, and the child was eventually born healthy.
This is explained by the following factors: your inhibin A level is affected by your age, weight, stage of pregnancy, whether you smoke, and some other characteristics of your body and your pregnancy. Therefore, the results of the quadruple test should be assessed in combination with all tests (together with tests for hCG, free estriol and AFP).
What to do if 2nd trimester screening is not normal?
If the results of your second trimester screening are not as good as you would like, then you need to see a geneticist. The geneticist will once again review all test data (including ultrasound results in the first trimester), and carefully question you about your health before pregnancy, the health of your husband and your relatives.
If the gynecologist concludes that there is an increased risk of Down syndrome or other abnormalities in your unborn child, he will recommend that you undergo amniocentesis. Amniocentesis will allow you to dot the i’s and find out whether the unborn child is really sick.
Source: https://www.mygynecologist.ru/content/%D1%81%D0%BA%D1%80%D0%B8%D0%BD%D0%B8%D0%BD%D0%B3-%D0% B2%D1%82%D0%BE%D1%80%D0%BE%D0%B3%D0%BE-%D1%82%D1%80%D0%B8%D0%BC%D0%B5%D1%81 %D1%82%D1%80%D0%B0-%D0%B1%D0%B5%D1%80%D0%B5%D0%BC%D0%B5%D0%BD%D0%BD%D0%BE% D1%81%D1%82%D0%B8-%D1%80%D0%B0%D1%81%D1%88%D0%B8%D1%84%D1%80%D0%BE%D0%B2%D0 %BA%D0%B0
When is AFP elevated?
An increase in the level of AFP in the blood of a pregnant woman is most often observed with fetal pathology, when a large amount of fetal AFP enters the amniotic fluid. Such pathologies include:
- spina bifida, anencephaly;
- hydrocephalus;
- threat of miscarriage;
- umbilical hernia;
- abnormalities in the development of the urinary system (polycystic kidney disease, absence of one kidney, etc.);
- illnesses of the expectant mother (diabetes mellitus, hypertension);
- gestosis (especially severe).
During normal pregnancy, AFP levels are elevated in multiple pregnancies.
What to do
Decoding the meanings is a matter for the doctor. When determining deviations in the analysis, you need to do an ultrasound examination to determine the exact gestational age. Ultrasound can also determine the presence of congenital defects in the fetus.
Deviation of AFP in any direction helps to establish the degree of risk of intrauterine pathologies. For an accurate diagnosis, it is recommended to undergo complex invasive methods to determine the chromosome makeup of the unborn child. For 100% diagnosis, amniocentesis is performed at 17-20 weeks.
If no pathologies have been identified, but the protein has deviations from the norm, an assessment of the risk of malnutrition of the child is made using a certain form. Amniocentesis is informative only up to the 24th week of pregnancy. For an accurate diagnosis, additional assessment of blood flow in the uterine arteries, the thickness of the placenta and blood flow in the baby’s aorta are used.
If the overall index is more than 7 points, doctors talk about placental insufficiency. Vitamins and medicines that improve beds are prescribed.