- About conception
- Surveys
Not every pregnancy ends with the happy birth of a baby. The number of cases where at some stage the fetus stops its development is constantly growing. This becomes a huge tragedy for the woman and her loved ones. After a while, the desire to try to have a child appears again, but the fear of loss and despair do not leave the expectant mother. In this article, we will talk about how and after what time to plan to conceive a child and what tests to take after a missed pregnancy in order to reduce the risk of its recurrence to a minimum.
A frozen pregnancy requires a serious check of the health status of both spouses.
Planning a pregnancy after a frozen one
We have already written about the causes and symptoms of regressive gestation. Many women do not want to stop in the face of difficulties and make new attempts to become a happy mother. Before planning a pregnancy after fetal death, it is necessary to find out the nature of the pathology that influenced what happened.
Among the main reasons for embryo freezing are:
- genetic disorders (heredity, chemical exposure, bad habits, ecology, age of the pregnant woman);
- viral diseases and other infectious processes that overcome the phytoplacental barrier;
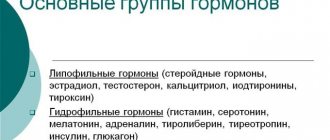
- hormonal imbalance caused by thyroid dysfunction, lack of estrogen and progesterone, excess testosterone;
- Rhesus conflict;
- teratozoospermia.
In order to get pregnant after a frozen pregnancy, you need to go through a certain path of preparation, which involves actively working on your mental and physical state. In 90% of cases, after pregnancy regression there is the possibility of reconception. To do this, the expectant mother’s body needs to equalize its hormonal levels, which will take at least six months.
Important criteria when planning are the factor of severe stress, self-flagellation, which results in worsening hormonal imbalance, withdrawal into oneself and lack of desire for re-fertilization. Another indicator of readiness for pregnancy is the physical component. The integrity of the uterine tissue, the absence of inflammation, and hormonal levels are important for this, because after the fetus has died, the procedure of curettage of the endometrium along with the embryo is most often carried out.
When planning to conceive again, you should contact a specialist who will prescribe the correct, safest treatment that will contribute to a more successful pregnancy experience.
Preparing for a new pregnancy
After an unsuccessful pregnancy, a woman wants to get pregnant again and finally realize herself as a mother. But doctors strongly recommend waiting at least six months before conceiving again. This is true, because in this situation you should not be guided by emotions, because a weakened body requires time to recover.
When planning a new pregnancy, approach carefully and follow two points:
- Talk to your gynecologist and consult with an endocrinologist to confirm the number of necessary tests that should be taken after fetal death.
- The upcoming pregnancy must be planned.
If the married couple has finally decided to expand their family, now all that’s left to do is find out what tests need to be taken in case of a missed pregnancy.
***
When can you plan a pregnancy after a frozen pregnancy?
You should plan your pregnancy during a period of stable self-confidence. However, it is not always possible to become pregnant after a frozen pregnancy, even with a normal mental state. Before you begin to prepare for conception, you should, under the supervision of a doctor, check the level of necessary hormones, as well as the thickness and functionality of the endometrium. We will tell you what tests to take a little later.
The endometrium is dependent on hormones, so sometimes it may take time, and sometimes a review of lifestyle. The thickness and functionality of the endometrium are two different things, so in some cases you can limit yourself to a number of measures to increase its thickness, and sometimes treatment with special drugs is necessary. Read about this in detail in the publication devoted to preparing the functional layer for conception.
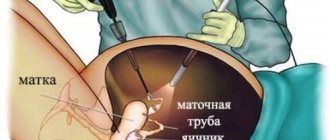
It is not recommended to conceive immediately after the healing of the uterine tissue, since rapid fertilization of an unrecovered organism can lead to repeated fetal death and more serious problems for the mother’s health. For example, synechiae can deform the uterus; if you do not complete the full course of treatment after curettage, adhesions may form in the fallopian tubes, and ectopic pregnancy is possible.
The risk after complete preparation of the hormonal background and restoration of the body does not exceed 10%. The risk decreases when the cause of fetal death is determined and eliminated, but it is reasonable to do expensive genetic tests only if a regressing pregnancy becomes habitual.
Doctors quite often prescribe contraception in order to restore the body for 10 and even 12 months, but planning a new pregnancy is possible after the resumption of ovulation and the endometrium, as well as hormonal levels. Progressive doctors recommend starting planning after 3-6 months, again, subject to the normal course of the recovery period.
When can you start planning for another pregnancy?
After an unsuccessful pregnancy, the body needs rehabilitation. Gynecologists suggest not to rush into conception, but to wait at least 6 months. This period is determined by the body’s need for recovery. Violation of this deadline may lead to a new failure. Although there have been cases when a woman successfully became pregnant after 3-4 months. After all, everything is individual. During this time, you can have time to undergo a full examination and, if necessary, treatment. You should know that about 85-90% of women who suffered a frozen pregnancy were able to become pregnant again and give birth.
Where should you start preparing for another pregnancy?
Before deciding to conceive again, you should undergo all the necessary tests, because infections disrupt the proper development of the fetus and cause various anomalies that provoke its death.
Pregnancy preparation includes:
- consultation and examination with a gynecologist;
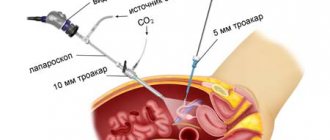
- Ultrasound of the pelvic organs;
- genetic testing;
- taking tests to determine a woman’s hormonal levels.
Preparing for conception involves not only passing all the necessary tests, but also strengthening the health of the expectant mother. You should exercise, eat right, take vitamin complexes, get enough sleep and avoid even minor stressful situations. After carrying out all the necessary preventive and medical procedures, the gynecologist will be able to choose the most favorable time for conception.
Hormonal status is the most important component of a successful pregnancy
Hormonal imbalance is far from a harmless phenomenon; behind it lies serious dysfunction of the body. To determine hormonal levels, blood tests are performed in laboratory conditions. Based on the data obtained, the doctor can determine the condition of the woman’s reproductive system and, if necessary, prescribe appropriate treatment.
It is mandatory to submit:
- follicle-stimulating hormone, which is responsible for ovulation. Its maximum level can be observed in the middle of the cycle.
- luteinizing hormone. It stimulates the production of prostegerone, which is considered the main hormone of pregnancy.
- prolactin. The hormone plays an important role in ovulation. Obstetrician-gynecologist about prolactin when planning pregnancy.
- estradiol Responsible for preparing the uterus for pregnancy.
- progesterone.
- testosterone.
- for 2 or more missed pregnancies - analysis for homocysteine. An obstetrician-gynecologist on the importance of homocysteine when planning pregnancy.
Not only the woman, but also the future father should undergo examination. He must undergo a consultation with a urologist, and also take a spermogram to determine fertilizing ability. Usually, during the recovery period after fetal death, a woman is prescribed hormonal medications to restore the balance of hormones.
Tests and examinations after
To the question: how to get pregnant after a frozen pregnancy? Doctors answer based on the cause of pregnancy regression. To clarify this circumstance, the attending physician is obliged to send the couple for examination.
It is necessary to take tests after a ST, if only because dangerous infections may be active in the blood, threatening the health of the couple. Among the necessary tests, there are three main ones:
- to identify a lack of thyroid hormones, excess testosterone, deficiency of estrogen and progesterone, which could cause pregnancy to end;
- for latent infectious diseases of the reproductive system;
- for TORCH infections;
- to identify genetic pathology during repeated embryonic death (karyotyping).
In addition to the general list of tests, the timing within which it is recommended to carry them out is also regulated. Hormone levels, for example, should be measured with the normalization of the menstrual cycle.
- Hormone testing is carried out according to the schedule recommended by the doctor after the first menstruation.
- During the first menstrual cycle, an examination is carried out for TORCH infections to identify antibodies to them.
- During the second cycle, it is recommended to undergo a full examination to identify disruptions in the homeostasis system and re-check hormonal parameters.
- A month after taking antibiotics, you can take the remaining tests for the microflora of the uterus.
Quite often, in about 50% of cases, pregnancy regression occurs due to untreated sexually transmitted infections, and if examinations were not carried out before conception, then tests should be taken. Among other indicators for determining the reasons for the freezing of the embryo, there is an analysis for the compatibility of blood groups, a genetic test (in case of repeated termination of pregnancy) and for identifying the number of chromosomes or other diseases transmitted by inheritance.
After identifying the causes, you should begin to restore the body to re-conception. If a spontaneous miscarriage does not occur when the fetus freezes, a procedure of curettage of the uterus with a vacuum or curette is performed, after which the woman is recommended to undergo a course of treatment. A month after the first natural menstruation, an ultrasound will be required to understand the condition of the endometrium.
What is a frozen pregnancy and its causes
A frozen pregnancy is understood as the cessation of embryo development for up to 20-27 weeks (most often this occurs in the first months) and its subsequent death. There can be many reasons for this condition.
In most cases, this is some kind of genetic anomaly that prevents the fetus from further developing and causes its death. Such a case can occur even in completely healthy spouses.
Other causes of missed abortion include viral infections (rubella, influenza), alcohol abuse, severe emotional stress, gynecological diseases and others.
Fetal freezing is detected either during a routine ultrasound or when a spontaneous miscarriage occurs. From a psychological point of view, a woman experiences a miscarriage more difficult, but from a health point of view, it is better for a non-viable fetus to leave the mother’s body than for it to begin to necrotize and endanger the woman’s health and life.
Frozen pregnancy is more common in the first trimester.
What vitamins to take
After a tragic event, a woman’s body requires thorough recovery, but due to severe stress, many lose their appetite, apathy sets in, and, naturally, depression sets in. This is a normal condition for any woman who has lost a pregnancy. In order to prevent the fetus from dying again, many gynecologists send their patients to a therapist to prescribe vitamins after a frozen pregnancy.
One of the most important vitamins in the first stage of gestation is folic acid or B9. Due to the lack of this micronutrient, the expectant mother may experience anemia, which results in defective development of the fetus. You should start taking folic acid while planning pregnancy, as severe deficiency can cause miscarriage or ST.
The vitamin that is recommended to be taken along with B9 is tocopherol or vitamin E. Its main feature when planning a child is its beneficial effect on the woman’s immune system, which in turn has a positive effect on the functional layer in the uterus, blood circulation and the functioning of the endocrine glands. The vitamin is found in fatty foods - meat, milk, vegetable and butter oils, eggs, herbs, and liver.
During the formation of the fetus, vitamins A, B, C and D play a role. Vitamins are prescribed by the doctor if he sees a need for it. Like a deficiency, an excess of vitamins negatively affects internal organs and the reproductive system as well.
Miscarriage
Infertility Research
If you have visited this page of ours, it means you are looking for answers to a painful question for you today - why did your unborn baby die in utero, why is this not the first time this has happened, who is to blame and, most importantly, what to do?
You may have already undergone expensive, lengthy additional medical examinations, but have not received an answer to your question. You may be currently preparing for curettage. In any case, we are ready to help you and your doctor solve the problem.
We will help you not only determine the reasons for what happened, but also answer the following questions together with your personal doctor:
— could this happen again in the future? - but what can you really do to avoid this? — what is the treatment route and will there be a result? — what is the way to plan and manage the next pregnancy?
Unfortunately, 90% of pregnancies that occur are spontaneous pregnancies, and, despite the couple’s belief that the pregnancy is supposedly planned, couples often do not undergo the required amount of previous planned examination. But many problems could have been avoided. Among the variety of reasons, genetic and often hereditary factors play the “first fiddle” in failures to conceive and carry a pregnancy to term.
Despite the rapid development of clinical genetics and the expansion of the information field in this area, neither patients nor doctors are still ready to take advantage of, and simply do not know about, modern and already absolutely accessible molecular laboratory methods for making a diagnosis.
Abortive material is not always subjected to at least classical cytogenetic analysis, and if this happens, then the method itself carries with it many ineffective failures.
What do couples facing miscarriage need to know?
Almost every fifth of all clinical pregnancies ends in spontaneous termination. The official language of statistics is that spontaneous miscarriages and missed pregnancies account for about 20% of all clinical pregnancies.
What actually stands behind such statistics? It is generally accepted that even under very good conditions for conception, the maximum probability of pregnancy in the menstrual cycle does not exceed 40%. 60 percent occur in preclinical losses (that is, even before pregnancy). After this primary filter has occurred, the chances of a successful pregnancy increase sharply and 80% of pregnancies progress, and 20% end in spontaneous termination of pregnancy. The pregnancy either stops or spontaneous miscarriage occurs. The majority of interrupted pregnancies - up to 80% - occur in the first trimester of gestation. And the most common reason for this is the pathological genetic status of the embryo, the presence of one or another defect in its genetic material that is incompatible with development and life.
Often, various genetic abnormalities of an embryo are random, and much less often they have a hereditary cause. And we are talking about the so-called “natural selection”, when nature itself gets rid of “defective” products of conception. Most often it is not possible to save such a pregnancy, but you can avoid a similar situation in the future by visiting a geneticist, especially for couples with a burdened reproductive history.
Miscarriage is considered to be the spontaneous termination of pregnancy at any time from the moment of conception to the full 37 weeks of pregnancy. Miscarriage can occur in two scenarios: spontaneous miscarriage and non-developing (frozen) pregnancy. What distinguishes a non-developing pregnancy from a spontaneous miscarriage is only the fact that in the first case there is no spontaneous emptying of the uterine cavity, and then the patient is referred for a medical abortion.
The worst thing is when miscarriage transforms into recurrent miscarriage (in 3% of couples who have lost a pregnancy at least once). And these statistics have only been increasing recently. The diagnosis of recurrent miscarriage is established if there are two or more spontaneous abortions in the anamnesis (in the past, in history).
The risk of miscarriage increases with a woman's age: from about 5% at age 20 to almost 50% for age groups of women beyond 35-40 years.
The most reliably proven connection between early pregnancy loss and two factors is the advanced and late reproductive age of the mother; a large number of previous miscarriages. And the more episodes of miscarriage, the worse the prognosis for subsequent conception: the risk of another loss after two previous losses reaches 29%, after three - 33%.
What genetic causes lead to missed pregnancies and spontaneous miscarriages?
One of the main causes of miscarriage is a chromosomal imbalance in the fetus. In most cases, such a chromosomal imbalance is a random event and no one is immune from it. However, the frequency of occurrence of chromosomal disorders is directly proportional to the age of the pregnant woman, exposure to harmful external factors, depends on the presence of any genetic pathology in the close family circle and a number of other factors.
We should not forget that the consequence of some forms of such chromosomal imbalance in the future can also be serious illnesses in the woman who lost the pregnancy, including cancer.
Chromosomal imbalance in the fetus can be represented either by quantitative chromosomal anomalies (when the number of chromosomes in the chromosome set is disrupted), or by structural chromosomal anomalies, aberrations (when part of the genetic material falls out in the chromosome structure or additional genetic material appears, or the genetic material is rearranged within the chromosome, between chromosomes), or a combination of quantitative and individual structural defects.
Quantitative anomalies:
Trisomy of autosomal chromosomes is the presence of three homologous chromosomes in the chromosome set instead of two. Most autosomal chromosome trisomies are lethal to the fetus. And examples of viable trisomies are Down, Edwards, and Patau syndromes.
Monosomy of autosomal or sex chromosomes is the absence of one of the paired chromosomes in the chromosome set. With monosomy for any of the autosomes, normal development of the embryo is impossible. The only monosomy compatible with life in humans is sex chromosome X monosomy, which leads to the development of Shereshevsky-Turner syndrome (45,X0).
Triploidy is the presence of an additional haploid set of chromosomes in the chromosome set. Triploidies are lethal to the fetus.
Polysomy of sex chromosomes is the presence of additional sex chromosomes in the chromosome set instead of two. An example is Klinefelter syndrome - the presence of one or more extra X or Y chromosomes in men.
Structural abnormalities:
Deletion is the loss of a DNA fragment within a specific locus, a gene on a chromosome.
Duplication is, on the contrary, an increase in chromosomal material, doubling a section of chromosomes.
The sizes of deletions and duplications can vary from large ones that are accessible to modern microscopes, to microdeletions and microduplications that can only be detected by modern high-resolution molecular methods.
Translocations are the exchange of regions between two pairs of homologous or non-homologous chromosomes.
Insertions are insertions of genetic material into a chromosome.
Inversions are a rotation of a chromosome section by 180 degrees within one chromosome.
The most common causes of pregnancy loss among quantitative abnormalities in the set of chromosomes are:
- complete autosomal trisomies (both one pair of chromosomes and double, triple trisomies). They account for about 60% of all known genetic causes of fetal death
- polyploidy (up to 15-20%%), most often - triploidy
— monosomy of the X chromosome (up to 15%).
Less commonly, the cause of a frozen pregnancy can be disturbances in the structure of chromosomes, a combination of various such aberrations:
— Translocations. An unbalanced chromosomal rearrangement (disproportionate exchange of sections between chromosomes with a violation of the quantitative and qualitative balance of chromosomal material) in the fetus can result in spontaneous abortion or lead to the appearance of a child with birth defects and/or mental retardation. This type of rearrangement occurs when the parents are carriers of a balanced chromosomal rearrangement (without changing the amount of chromosomal material). And then, following the study of fetal DNA, additional examination of the chromosomal material of the parents will be required in order to avoid pregnancy loss next time.
How to diagnose a genetic defect in case of pregnancy regression?
To do this, first of all, it is necessary to study the abortive material in a genetic laboratory.
Unfortunately, it is not always the case that a married couple faced with an unexplained miscarriage ends up in a geneticist’s office to receive professional “guidance” in a follow-up examination to try to establish these causes and receive recommendations for the next pregnancy.
However, if you are experiencing miscarriage, discuss genetic testing with your doctor. And you can do this in our center, where we will not only quickly and accurately carry out the laboratory analysis itself, but will accompany you and your doctor with consultation before it is carried out and after the results are obtained.
Indications for the study of abortifacient material
- there are already two or more episodes of spontaneous abortion or missed abortion in the anamnesis
- if a previous miscarriage or medical abortion has already revealed a chromosomal pathology in the fetus
- one of the spouses was previously identified as a carrier of a chromosomal imbalance or hereditary diseases
- if the family already has a child with a chromosomal pathology or congenital malformations
And even in the case of an unsuccessful first pregnancy, you can find out more about the causes of fetal death.
The essence of the study
Whichever of the known methods of laboratory analysis of abortive material is prescribed to you, its essence lies in assessing the karyotype of the deceased fetus for abnormalities in its chromosomal material. During subsequent evaluation of the karyotype map, the type of chromosomal defect, its location, and the association of this defect with the pathological effect of pregnancy loss are established.
The material for the study is any tissue belonging to the fetus - the fertilized egg during a spontaneous miscarriage, the membranes and tissue of abortive material obtained during a medical abortion. The only difference is that one method requires exclusively tissue with dividing cells, as in the case of a standard classical cytogenetic study (microscopy), while for other, more innovative, molecular cytogenetic, molecular genetic studies, this is not required and the study can be carried out in a much shorter time and with maximum accuracy, superior to the standard method of cytogenetic analysis.
Which laboratory method to choose?
We will select the optimal research method for you based on your specific clinical case. It doesn’t matter to us how far away you are from our laboratory, or in what region of Russia you live. Our logistics capabilities will allow you to deliver your biological material from any city and in the pre-analytical state that we need to carry out the research.
Currently, there are various methods of karyotype analysis: from those that appeared in laboratory practice a long time ago and have become standard routine analysis, to innovative molecular modern genetic tests that have incredibly high accuracy and speed of production.
The capabilities of our laboratory are the latest generation methods, which eliminate the shortcomings and inaccuracies of standardized routine methods. In one clinical case, we can limit ourselves to a targeted study of individual chromosomes, defects in which occur with the greatest frequency. In another case, we will recommend you a genome-wide molecular karyotyping method (that is, examining all chromosomes in full and for all defects known to be clinically significant, even the smallest ones, inaccessible to modern microscopes).
Why don't we study abortive material using the standard cytogenetic method?
Standard cytogenetic karyotype analysis is a method that has long been used in domestic cytogenetic laboratories. However, with the advent and rapid development of more modern methods of genetic diagnostics - molecular cytogenetic, molecular genetic, which are 100-1000 times superior in accuracy and diagnostic significance, standard karyotyping can be considered outdated in relation to more modern and popular technologies. Moreover, the cost of molecular methods is not much higher than classical cytogenetic methods.
Cytogenetic analysis of the karyotype is carried out by microscopy, that is, using various modifications of microscopes, various algorithms for processing and preparing preparations of abortive material to ensure visualization of chromosomal material, varying degrees of training and professionalism of cytogeneticists evaluating the results obtained. That is, one way or another there is a certain effect of subjectivity in the assessment and interpretation, and therefore the percentage of false results cannot be excluded.
Flaws
This karyotyping method is possible only if “living” cells of the material capable of dividing are delivered to the laboratory. Hence - difficulties in transportation under special conditions, difficulties in delivery from separate regions, increased cost of transport services due to special preanalytical requirements, long time for cell division (the study period will be from 15 to 26 days). Another question is possible and by no means rare cases of false results due to the inability of this method to exclude contamination of the test sample with maternal genetic material. Often the mother's karyotype is mistaken for the fetal karyotype. And since the mother’s karyotype is not abnormal, the cause will not be established. The sample may be contaminated with other biological material, it all depends on the conditions under which the abortive material sample was collected. If the above is unfavorable, the chance to establish the cause is lost, the abortive material is simply disposed of. And finally, the limitations of the diagnostic value of the method due to its low resolution (what the method can and cannot detect). The method will 100% detect aneuploidies (numerical deviations in the set of chromosomes), determine the sex of the fetus (if there is a Y chromosome in the karyotype, male), and can see that a large fragment/section of a chromosome has been lost, or an equally large additional fragment has appeared. A huge number of microreorganizations, which can also lead to serious consequences - loss of pregnancy, the birth of a child with a severe chromosomal disease, remain beyond the capabilities of this method. Our alternative is molecular karyotyping on microarrays - a chance to quickly, reliably, without misfires, either find the cause or rule it out in one study.
CREDO is a first-line test in diagnosing the causes of miscarriage - accelerated, automated, accurate, reliable, convenient, and affordable.
A test that eliminated the shortcomings of other methods. A test that combines the required diagnostic purposes. A test that has undergone many years of practice after its first clinical testing and has accumulated reliable statistics. A test that will eliminate unnecessary costs for diagnostics and sometimes ineffective treatment, and therefore is optimal in terms of cost savings. A test that won't make you worry about a possible "lab failure" or "lab error" A test that is accessible from any region. A test that suits your doctor with its diagnostic and useful capabilities will really help you in the fight against miscarriage. CREDO is a first-line test in diagnosing the causes of miscarriage.
Undeniable advantages
The test does not require a “living” dividing cell, which eliminates such strict requirements for samples of biological tissue of abortive material in the case of the cytogenetic method, their preservation, and transportation. We will isolate a small amount of DNA from any cell for research. For us, only the minimum preanalytical requirements are fundamental - place the abortifacient material in a sterile container, which we will provide you free of charge along with the shipping packaging, add saline solution, and store the material at a temperature of +2 - +8 until our courier arrives. The test algorithm completely eliminates subjectivity, due to standardization, automation and software of the entire laboratory process. Modern matrices and scanners, reagents that provide modern research design, access to constantly expanding bioinformatics databases - all this makes molecular karyotyping highly reproducible and has decent analytical value of the method. The resolution of the test is 100 to 1000 times higher than conventional cytogenetic karyotyping under a microscope, and therefore, much more information will be obtained about the genetic status of the deceased fetus. Depending on the resolution characteristics of microarrays/platforms for studying fetal DNA, diagnostic searches can be carried out simultaneously across more than 240 and up to 500 cytogenetically significant syndromic areas. The speed of analysis is from 7 to 14 days, depending on the tasks assigned to this study.
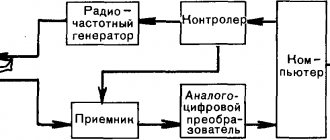
About molecular karyotyping technology
We carry out molecular analysis of chromosomal material based on aCGH technology - comparative genomic hybridization on microarrays. The use of several formats of such single-nucleotide microarrays allows us to provide genome-wide coverage (all chromosomes are examined simultaneously) and achieve certain research goals, focusing on the most significant syndromic regions and about 1000 functionally significant genes.
The method is based on automated analysis of CNVs/SNPs after hybridization of patient DNA samples and reference DNA on a microchip. A microchip is an industrially manufactured microarray with immobilized DNA containing genomic fragments with known nucleotide sequences. Each fragment is a probe/marker/varies in length and specificity. A certain type of microchip is used for certain tasks, depending on the markers present on the platform.
From the supplied sample of abortive material, fetal DNA is isolated, which undergoes special processing and preparation, and staining with fluorescent dyes. The test DNA and reference DNA are painted in different colors. DNA samples mixed in equal quantities are applied to the microchip, a hybridization process occurs, a modern scanner scans the result of this hybridization - the number of DNA fragments is determined by the intensity of the fluorescent glow at each point of the microarray, special software allows an automated analysis of the results obtained, based on which the geneticist , using the software capabilities of this study with access to international information databases on the correspondence of a particular chromosomal defect with a certain pathological condition, prepares its conclusion.
What can be revealed using CREDO tests:
100% all aneuploidies on all chromosomes All clinically significant known deletions/duplications within microarray resolution, including submicroscopic defects. Mother cell contamination
Tests have limitations
— Balanced structural rearrangements cannot be detected — Point mutations of genes — Low-level mosaicism <15%
The presence of SNP markers on the microchip will provide additional detection capabilities:
— Microdeletions/microduplications (only those that are within the resolution of the matrix) — Unbalanced translocations (within the resolution of the matrix) — Loss of heterozygosity (within the resolution of 5-10 Mb) — Uniparental disomies (within the resolution of 5-10 Mb) — Determinations of the level of mosaicism - Ability to differentiate triploidies.
If chromosomal abnormalities are detected
Of course, once you receive our conclusion, discuss it with your doctor.
In some cases, additional consultation with a geneticist may be required.
Call us on +7 499 551 7751, and our specialist will help you figure it out.
In some cases, additional genetic testing of spouses may be required, for example, if an unmatched translocation is detected. Remember that a number of chromosomal defects dramatically increase the risk of repeat pregnancy loss.
And all this in order to predict a future pregnancy, maintain it and avoid the birth of a sick child.
How to order a study in preparation for a medical abortion?
Contact us by phone +7 499 551 7751.
Our logistics specialist will accompany you:
— will place an order for the study, — will arrange the delivery by our courier of a specialized free kit for collecting abortifacient material by your doctor, along with instructions on how to do it, — will arrange and ensure the removal of biological material, — will instruct how to preserve the tissue sample until the courier arrives.
Eliminating the causes of disease
When planning conception after a frozen pregnancy, as mentioned above, it is necessary to undergo examination to identify possible pathologies. However, this is only the first step towards successful pregnancy. The second step will be the elimination of pathologies.
If the cause of ST is hormonal, then the gynecologist, based on individual indicators, prescribes special medications that correct the functioning of the thyroid gland, improve blood circulation in the pelvis, and help normalize the level of the endometrium.
Definitely, sexually transmitted infections must be destroyed for reconception. The cause of embryonic death may be influenza or other viral diseases, so the disease should be eliminated and immunity restored.
The situation with genetic damage that caused fading can be resolved if, during preparation for pregnancy, the body switches to the right lifestyle, gets rid of bad habits, changes the environment and protects itself from toxic chemicals. If the issue is the genetic inheritance of one of the partners, then you can turn to assisted reproductive technologies or surrogacy.
Psychological readiness for conception
In addition to all of the above related to the general preparation of the body, an equally important factor is the moral state of a woman. When planning a pregnancy after ST, it is necessary to understand that the fading of the fetus is the result of a combination of circumstances, and not a categorical “no” to conception.
After a loss, it seems that there is no hope, but the possibility of a normal subsequent pregnancy, provided that negative factors are eliminated, is 90% successful.
The loss of a child can result in deep depression, but if you want to have a baby, you need to psychologically prepare for a second attempt. It is quite difficult to look at the world optimistically after such a loss, but there is always a chance to give a new life, the main thing is to be prepared for it. In order to quickly restore your psychological health, it is recommended to consult a specialist. A stable psychological state will further contribute to the preservation of the fetus.
For a new conception, complete recovery from a previous unsuccessful experience is necessary, including psychological readiness and absence of fear of fetal death. You should also contact a psychologist if the expectant mother’s fear of losing the fetus has returned, because a woman becoming nervous can affect the further outcome.
Do I need hormonal contraceptives?
In the event of a miscarriage or missed pregnancy, gynecologists almost always prescribe hormonal contraceptives. Since both cases involve curettage of the endometrium of the uterus, this represents enormous stress for the female body. However, if a woman wants to have a child, these prescriptions are not entirely appropriate. In the post-Soviet space, after curettage, hormonal drugs are often prescribed for the following conditions:
- the danger of pregnancy for a woman’s body;
- prevention of cervical erosion;
- restoration of hormonal levels.
It’s worth stopping here and asking the question: who exactly might be at risk of pregnancy if a woman still wants to have a child? The physiological readiness for a second pregnancy is confirmed by the state of the endometrium and the restoration of ovulation. A woman can feel psychological readiness herself or after working with a psychologist.
A completely reasonable question for many girls is: “what if I can’t get pregnant after OK?” It is important to remember that hormonal contraception does not cure, but only masks menstrual problems, causing monthly bleeding.
If you want to conceive a child soon, you must use barrier methods of contraception until the menstrual cycle is completely restored and you are ready for a new pregnancy.
Diagnostics
Confirm that the pregnancy is frozen using the following methods:
- gynecological examination - the size of the uterus does not correspond to gestational age;
- laboratory examination - the hCG level does not increase or decreases;
- ultrasonography – anembryony (no embryo in the fertilized egg), no dynamics in embryonic development. Hemorrhages in the area of attachment. Fetal deformity is detected before 4 weeks of pregnancy;
- Dopplerography – heartbeat cannot be heard (measured from the 7th week).
In case of partial miscarriage, an ultrasound diagnostician visualizes the remains of the fetal place. If the diagnosis is unclear, ultrasound and tests are repeated after 3-5 days.
Bottom line
If you are interested in the question of how long it takes to get pregnant after a frozen pregnancy, then the answer will be strictly individual. In order to conceive again, it is necessary to find out the cause of the thyroid disorder and eliminate it:
- Hormones. Hormonal levels are leveled with the help of lifestyle correction, special medications and vitamins.
- Infections. As part of the preparation, all diseases must be cured, since weakened immunity affects the gestation of the fetus.
- Genetics. It is impossible to eliminate the genetic indicator, because it may be based on blood incompatibility or due to the age of the pregnant woman. The older the pregnant woman, the greater the likelihood of the appearance of the 47th chromosome. In such a situation, auxiliary methods are used.
- In most cases, when preparing for a repeat pregnancy, it is enough to eliminate all sorts of negatively influencing factors, restore the body, increase immunity, start eating right and look more positively into the future.
In the desire to conceive a child, it is very important not to harm yourself, take full responsibility for your health condition and, if necessary, undergo treatment. Have you encountered similar situations? Share your experience in the comments.
What to consider when planning your next pregnancy
A woman has a hard time bearing the death of a fetus, since she is already hormonally and morally determined to become a mother. The most common question women ask is when can they plan their next pregnancy and what measures to take to prevent a missed pregnancy from happening again.
You'll have to wait in any case. After a frozen pregnancy, a woman undergoes a diagnostic curettage to make sure that there are no pathological tissues left in the uterine cavity. In addition, the resulting material is sent for histological examination to study and establish the possible cause of the missed abortion.
After curettage, a woman needs about six months to restore the functional layer of the endometrium. During this period, the doctor prescribes the necessary tests to find out the cause of the problem.
After six months, the specialist examines the woman and checks the test results, and only after that gives an opinion on when the next pregnancy can be planned. Thus, before six months or a year, you should not think about a new pregnancy in order to protect your body and increase the chances of a normal course of the next attempt to become a mother.
Important! The next attempt at conception must be strictly planned. This is the only way to prepare and give birth to a healthy baby.
You can find out about fading pregnancy at a scheduled ultrasound.