Attacks of bronchitis
One of the fairly common diseases, which is often underestimated by many, is bronchitis. It is a pathology when inflammation of the bronchi, elements of the bronchial tree, develops. A virus or bacteria is enough to seriously worsen your health. Untreated throat infections, a runny nose, or ignoring ARVI can easily lead to severe inflammation in the lungs. In addition, bronchitis often develops due to inhalation of large amounts of dust or smoke. This pathology poses a particular danger to smokers, people with weakened immune systems, chronic heart and lung diseases, the elderly and young children.
Do not cough! How to act so that bronchitis causes minimal damage to the body Read more
The symptoms of bronchitis are quite typical. With it, a person develops :
- Feeling of sore throat
- Cough that starts as dry and becomes wet with sputum production
- Temperature increase
Do not underestimate pathology, because... if not properly treated, it can easily lead to pneumonia or chronic manifestations of the disease. Bronchitis is usually treated with symptomatic therapy, which relieves inflammation and fever, as well as expectorants, which promote more productive expectoration. As an additional recommendation, patients are offered to drink plenty of fluids. If the pathology is caused by bacteria, patients are prescribed antibiotics; if the pathology is caused by a virus, antiviral drugs are prescribed.
Prevention
To prevent increased formation of sputum in the lungs, you must follow simple rules:
- Strengthen the immune system - toughen up, eat right, exercise, get enough sleep,
- Don't get too cold
- No smoking,
- Humidify the indoor air
- Avoid exposure to allergens and aggressive irritants,
- Sanitize infectious foci - caries, otitis media, sinusitis,
- Optimize your drinking regime.
Phlegm in the lungs is an alarming sign and a dangerous symptom, and if it appears, you should go to the doctor. Without qualified medical care, the pathological process will continue to develop and lead to irreversible, deadly consequences.
Chronic emphysema
Chronic bronchitis as a systemic disorder of the lungs leads to the appearance of a pathology such as pulmonary emphysema. The disease is a violation of the processes of breathing and gas exchange in the lungs.
From bronchitis to emphysema and cancer. What does a smoker's cough mean? More details
Emphysema can be recognized by signs such as::
- Difficulty breathing, and in some cases, complete inability to breathe
- Blue skin
- Presence of shortness of breath
The pathology is characterized by slow development, when in the initial stages it is almost invisible. So, for example, the same shortness of breath first appears only after physical activity, but then begins to be observed constantly, even when the person is at rest. This pathology usually leads to disability. This means that treatment should be started as soon as possible to minimize the risk of complications. Standard therapy involves the use of antibiotics, drugs that dilate the bronchi and have an expectorant effect. Also among the recommendations you can often find breathing exercises and the use of oxygen therapy.
Koch stick
One of the most common diseases today is tuberculosis. Its cause is the entry of a specific microorganism - Koch's bacillus - into the lungs along with inhaled air when communicating with a carrier of the pathology. Tuberculosis is usually divided into 2 types: open and closed forms. Moreover, the second is the most common and indicates that a person is a carrier of the pathology, but does not transmit it to others. You can only become infected from a patient with an open form. The danger of tuberculosis is in its slow progression - at first (and this may be several months) it does not manifest itself in any way, but at the same time it is already carrying out its destructive activity in the human body. Later, as the pathology develops, a person may experience symptoms such as:
One on one with an invisible enemy. Robert Koch and his wand Read more
- General weakness
- Increasing indicators on the thermometer
- Weight loss (unreasonable)
- Cough
- Coughing up bloody sputum
Doctors say that the key to successful treatment of pathology is timely initiation of therapy and the use of several anti-tuberculosis drugs at once. Naturally, only a doctor should prescribe them. Treatment of tuberculosis is carried out in a hospital setting.
Interpretation of survey results
The conclusion based on the examination results is carried out by professional specialists. Among them are a radiologist, pulmonologist, oncologist, cardiologist, therapist, and surgeon.
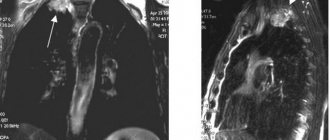
Based on an X-ray examination of the mediastinal shadow, careful study of hard photographs taken in several projections, artificial contrast, CT and MRI results, specialists make a conclusion about topographic changes in the anatomy of the mediastinum.
Detecting pathological changes in an image is an extremely difficult task. It requires the specialist to have extensive knowledge about the normal state of the contours of the mediastinal shadow. The algorithm of actions for describing the identified changes in this area is as follows:
- The initial diagnosis reveals the presence of neoplasms in the mediastinum. Less informative is the X-ray examination obtained by taking pictures in the direct projection of the anterior and posterior zones of the mediastinum. In this case, all organs of this area find themselves in the zone of the median shadow. The best conditions for examining the mediastinum are oblique and lateral projections. Detection of nodular thickening along the anterior connecting edge indicates the presence of a neoplasm in the anterior mediastinum. When the azygoesophageal recess is displaced, a tumor is expected to form in the middle mediastinum.
- Tumors of various etiologies and patterns of manifestation develop in the mediastinum. In the X-ray report, the specialist describes its morphological features. The formation under study may be isolated and manifest as a unilateral change in the outline of the mediastinum. With diffuse formation, bilateral expansion of the mediastinum is observed. The first case indicates the primary nature of the neoplasm, the second - lymphadenopathy due to the presence of metastases, or mediastinal lymphoma.
- Depending on which part of the mediastinum is examined, the affected area is determined from the image (lateral projection), and the differentiation of a number of suspected diseases is described. Based on this formulation, the further course of clarifying examination methods is selected, allowing one to choose effective therapeutic tactics.
- During interpretation of the results, accompanying pathological deviations from the norm are described. This allows you to reduce the number of possible pathologies. For example, the detection of an isolated neoplasm in the anterior mediastinum and the presence of nodules in the lung indicates the likelihood of developing a malignant epithelial tumor of the thymus. Detection of calcification indicates diseases such as mediastinal teratoma, goiter of the same type, granulomatous lymphadenopathy, aneurysm or neurogenic tumor.
- The final stage of describing changes in the mediastinum is drawing up a diagnosis. The type of pathological formation (diffuse or isolated), the area of mediastinal expansion is also indicated, and the presence of concomitant pathological changes is noted.
Interpretation of the examination results carries extremely important diagnostic information that characterizes the features of mediastinal expansion and determines the choice of treatment regimen for the patient. Identification of the exact localization of the pathological focus in various parts of the mediastinum determines the advisability of choosing other diagnostic techniques in order to clarify the diagnosis and select treatment methods for the patient - medicinal or surgical.
Constant inflammation
Many people know that pneumonia can be deadly. However, there are still those people who manage to make their condition chronic. With the development of a chronic course of pneumonia, an inflammatory component will always be present in a person. He will also regularly encounter bronchitis, chronic nonspecific lung diseases and other pathologies. Moreover, each exacerbation of chronic pneumonia will lead to the appearance of new foci of inflammation in the tissue and an increase in the area of sclerotic changes.
A disease that takes a year to cure. What is insidious about pneumonia? More details
Among the symptoms of this pathology are:
- Cough with mucopurulent sputum
- Presence of wheezing in the lungs
- Increased body temperature during periods of exacerbation
- Development of chest pain
- Respiratory failure
The pathology can be complicated by pulmonary heart failure, the development of abscesses and gangrene of lung tissue.
The Ministry of Health spoke about invisible pneumonia in patients with COVID-19
Doctors are increasingly noticing asymptomatic forms of pneumonia in patients with coronavirus, said Russia’s chief pulmonologist Sergei Avdeev. Some people may not even feel any major changes happening to their lungs.
“There are patients with COVID-19 who have absolutely no complaints, symptoms or signs of the disease. There is no fever, no cough, no shortness of breath. At the same time, when performing a computed tomography, patients show signs of pneumonia,” the doctor told Rossiyskaya Gazeta.
He emphasized that the new atypical types of pneumonia are indeed different from community-acquired pneumonia, which was previously known to medicine.
As Avdeev explained to Gazeta.Ru, some patients do not have pronounced symptoms, since the changes in their body are not very large-scale. “This happens when the problem is not global, and pneumonia does not yet occupy a very large area,” the doctor said.
The colleague’s words were confirmed by pulmonologist Rustem Nasretdinov.
“If pneumonia does not lead to symptoms, this means that only the lung tissue is damaged, and not their final sections - the alveoli,”
- the doctor explained to Gazeta.Ru.
According to him, it is precisely because of the asymptomatic course of coronavirus pneumonia that the official statistics of those infected in Russia may differ significantly from the real number of patients with COVID-19. “If we had taken biomaterial for tests for coronavirus using the bronchial lavage technique (a medical procedure for introducing a neutral solution into the bronchi and lungs and studying the condition of the respiratory tract - Gazeta.Ru), three times more cases would have been identified,” Nesretdinov noted.
Also, one of the reasons for the asymptomatic course of pneumonia with COVID-19 may be that the infection does not enter the blood, says a virologist at the Center for Epidemiology and Microbiology. Gamaleyi Viktor Larichev.
“Most often, a person notices changes when he develops fever and symptoms of intoxication - muscle pain, temperature. But in this case, changes occur in the lungs, but the virus does not enter the blood, and the cascade of enzymes does not start, so the person does not feel anything. And, strictly speaking, there is no bronchitis either, which means there is no cough either,” the doctor explained to Gazeta.Ru.
At the same time, he emphasized that the likelihood that new types of pneumonia will lead to serious consequences is low. “Most likely, a person with an asymptomatic form of pneumonia will simply get over the disease and recover. But this is the first time we have encountered this phenomenon on such a scale, so perhaps we still have something new to learn,” explained Larichev.
Sergey Avdeev also agrees with him - according to him, no one is immune from the transition of SARS into more serious forms, but most often people are still able to overcome the disease on their own.
“Just remember the case of the Diamond Princess cruise ship. There, 54% of those infected had no signs of the disease, and a computed tomography scan showed pneumonia, and nothing, everyone recovered. Most likely, in other asymptomatic patients, pneumonia will also go away without any consequences,”
- the pulmonologist told Gazeta.Ru.
At the same time, Rustem Nasretdinov is convinced that damage to the lung tissue can quite often “spread” to the alveoli. “And if the final sections of the lungs are affected, then this, as a rule, leads to serious symptoms and a severe course of pneumonia - even death,” the doctor concluded in a conversation with Gazeta.Ru.
Let us recall that earlier the head of Rospotrebnadzor Anna Popova said that in Russia from 45 to 50% of those infected with coronavirus do not feel any symptoms. However, scientists from Singapore also reported that worldwide, 50 to 70% of those infected with coronavirus are asymptomatic.
According to the chief pulmonologist of the Russian Federation, Sergei Avdeev, the course of COVID-19 without a clear clinical picture is the main problem of the spread of infection, since patients with asymptomatic disease still remain a source of infection for others.
Genetic heritage
Today, one can increasingly hear the name of a pulmonary pathology such as cystic fibrosis. It is a severe hereditary disease characterized by tissue damage and malfunction of the respiratory system. The cause of this problem is a genetic change in chromosome 7 - the gene responsible for protein synthesis is located here. Due to malfunctions in its operation, chlorine ions begin to accumulate in the cell, attracting sodium ions. All this causes the accumulation of water inside the cell, collecting from the intercellular space. And then the endocrine glands come into play, producing secretions - tears, mucus, sweat - with altered properties. All this leads to disturbances in the functioning of the body as a whole. The fluid is not removed, accumulates and causes tissue drying, development of cysts, sclerotic changes, fibrosis, etc. Purulent inflammations are also common.
The discharge of sputum and the patency of small bronchi are also impaired. Their glands become filled with mucus and pus and become enlarged, causing breathing problems. Often this stagnation is accompanied by a bacterial infection.
What is cystic fibrosis? Disease in questions and answers Read more
Cystic fibrosis can be recognized by:
- Thick sputum produced when coughing
- Frequent exacerbations of pulmonary pathologies
- Dehydration
- Increased appetite with insufficient weight and development
- Thickening of fingers, etc.
This disease is deadly and incurable. But still, to maintain a person’s life, they use a certain therapy that allows him to feel satisfactory. Doctors usually suggest mucolytics, long courses of antibiotics, inhalations, breathing exercises, pulmonary drainage and much more.
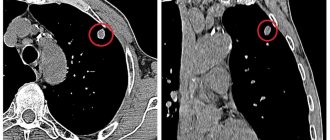
Indications for computed tomography
With radiography (X-ray) and CT, you can quickly find out the diagnosis and identify the causes of the disease. The choice of diagnosis depends on the symptoms of the disease, its characteristics, and the age of the patient. CT scan of the lungs is performed for:
- pleural studies;
- identifying the characteristics of pneumonia;
- diagnosis of tuberculosis;
- determination of benign and malignant tumors.
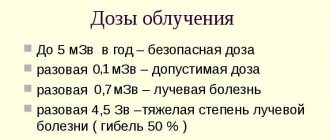
CT scanning is not recommended frequently for preventive purposes; this study is carried out according to medical indications. Fluorography can and should be done once a year for preventive purposes. This is an opportunity to identify pathologies. Cancer, tuberculosis, pneumonia are dangerous illnesses of our time. The radiation dose received during the procedure is minimal.
CT scan reveals diseases:
- mediastinitis;
- lymphogranulomatosis;
- abscess;
- tuberculosis;
- pleurisy;
- cancer;
- metastases;
- congenital and acquired anomalies;
- hernia;
- diaphragmatic paralysis;
- parasitic lung cyst;
- reduction of a lung segment;
- infarction pneumonia.
CT scan reveals enlarged thoracic lymph nodes, causes of pain in the chest and lungs. The study makes it possible to monitor the treatment of various lung diseases and bronchiectasis. The tomograph shows changes in the pleura and tissues and helps track the accumulation of fluid or blood in the lung. Using a tomograph, other organs, the inner ear, teeth, and brain are also examined.
Tomography is used by medical specialists to make an initial diagnosis or clarify a previously diagnosed disease of the respiratory organs. A study is prescribed if an oncological process is suspected.
Diagnosis CT scan of the lungs establishes early stage tuberculosis. A method is prescribed to determine the size of the pathological focus, the degree of damage, and monitor the effectiveness of drugs prescribed for tuberculosis. Indications include the detection of changes in organic tissues that were initially differentiated using x-ray or the Mantoux test. It is better to do the examination in a timely manner.
Initially, if tuberculosis is suspected, the doctor prescribes fluorography. This method is more accessible to the population and at a price. X-rays are present in every clinic. Buses with transportable X-ray units periodically arrive in remote rural areas. Research using a tomograph is more expensive and is available only in large cities. Therefore, the choice of lung examination method often depends on the patient’s area of residence. CT scans are often prescribed only in emergency situations, when the doctor needs more information about the course of the pathology.