FGDS of the stomach is, in official medical language, gastroscopy. This term is from the Greek γαστήρ - which means stomach and σκοπέω - which means I observe, look.
Let's imagine that a patient has a stomach problem. Diagnosing the problem of an internal organ is possible only with the help of tests. But this is an indirect diagnosis. But seeing and taking a piece of tissue from the source of the disease for analysis is more accurate.
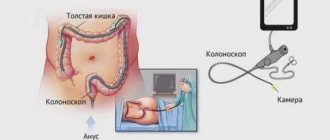
A special instrument, a gastroscope, helps with this. In its modern form, a gastroscope is a flexible tube with a fiber-optic system inside, which allows you to visually examine the gastric mucosa from the inside.
The FGDS method allows you to examine not only the stomach. It is also possible to examine the esophagus and duodenum. A modern gastroscope (fibrogastroscope) is also equipped with an instrument for taking material for biopsy .
FGDS of the stomach - what is it
FGDS of the stomach is a diagnostic method that allows you to examine the mucous membranes lining the stomach and duodenum using an endoscopic device - a gastroscope (the device is inserted into the stomach through the mouth).
The EGD procedure of the stomach is a type of gastroscopy. The entire complex of gastroscopy is divided into:
- FGS (conventional gastroscopy and fibrogastroscopy) – during this examination only the stomach is examined;
- VEGDS (videoesophagogastroduodenoscopy) – using a video gastroscope, the mucous membrane of the esophagus, stomach and duodenum is examined;
- EGDS (esophagogastroduodenoscopy procedure) - the EGDS technique involves examining the mucous membrane lining the esophagus, stomach and duodenum using a gastroscope (a flexible fiber-optic system).
For reference. All gastroscopy techniques are similar to each other, the fundamental difference is only in the scope of the study (stomach, stomach and duodenum, all parts of the gastrointestinal tract).
What is gastroscopy?
This diagnostic procedure is the most informative method of examining the stomach using an endoscope - a flexible tube with a diameter of up to 10 mm, which has a video camera at the tip. During gastroscopy, the monitor of the endoscopic apparatus shows a visual picture of changes in the mucous membranes (the presence of inflammatory foci, atrophic areas and erosions), which are assessed by a qualified specialist.
Gastroscopy of the stomach is done for:
- determination of acidity;
- removal of a foreign body;
- identifying the cause of gastric bleeding;
- cauterization of a bleeding artery;
- polyp excision;
- detecting the presence of bile in the stomach;
- applying the drug to the ulcerated surface;
- taking a biopsy of a suspicious area of the mucosa;
- expansion of the narrowed section of the esophagus (bougienage);
- selection of biological material for testing for Helicobacter pylori (a pathogenic bacterium that lives in the pylorus of the stomach).
In modern medical centers, gastroscopic equipment is combined with ultrasound equipment, which allows you to accurately study the thickness of the walls of the stomach and detect existing seals inside them
Why is fibrogastroduodenoscopy performed?
FGDS of the stomach is performed using a flexible probe with a built-in video camera. Examination of the gastric mucosa using FGDS allows us to identify even minimal changes affecting only the superficial layers of the mucosa.
When displaying an image on a screen, it can be enlarged, so the doctor can identify pathological lesions ranging in size from several millimeters.
Also, when performing FGDS of the stomach and duodenum, tissue can be taken ( stomach biopsy ) for further research using histological, cytological and immunochemical methods.
For reference. If necessary, during an FGDS, the doctor can remove small polyps or stop gastrointestinal bleeding.
The advantage of FGDS over other diagnostic techniques is:
- high degree of information content and security;
- the procedure is well tolerated and painless (modern endoscopic tubes are significantly different from the old thick hoses previously used for gastroduodenoscopy);
- the possibility of taking biopsy material, portions of gastric juice, bile or duodenal contents during the procedure;
- the ability to assess the degree of gastroesophageal reflux (with reflux, the gastric fluid is thrown into the esophagus);
- the ability to promptly identify various tumors, erosive and ulcerative damage to the mucous membrane, polyps, and find the cause of bleeding;
- the possibility of stopping bleeding and removing small polyps during FGDS.
Diagnostic capabilities of FGDS
In the process of deciphering the results of fibrogastroscopy, the doctor can evaluate in detail the functional and structural features of the organs being examined.
So, during diagnosis the following is determined:
- patency of the stomach, esophagus and duodenum;
- the presence of strictures (stenoses, narrowings), scars;
- the consistency of the cardiac sphincter separating the esophagus from the stomach;
- structural changes in the mucosa (inflammation, ulcers, erosion, atrophy, hypertrophy, metaplasia, areas of atypical epithelium);
- the presence of esophagogastric and duodenogastric reflux;
- hernial protrusions of the esophageal opening of the diaphragm;
- diverticulosis - protrusion of the muscular wall of organs;
- neoplasms of various types (polyps, papillomas, tumors);
- stages of gastritis, ulcers and others.
All these diagnostic capabilities of FGS allow us to consider the procedure indispensable in gastroenterology, surgery, oncology, and other branches of medicine related to the treatment of the gastrointestinal tract.
Therefore, when prescribing it, you should never refuse, but it is better to read reviews about the examination in order to prepare yourself mentally for visiting the diagnostic room.
What does the study show?
After the procedure is completed, the specialist makes a conclusion about the condition of the organs examined using an endoscope. This research allows:
characterize the condition of the mucous membrane lining one or another part of the digestive system (color, shine, surface, texture, presence of folds);- identify visible defects, injuries, scars, fistulas, tumor formations;
- assess the motor activity of the organ;
- describe its contents (stomach juice, mucus, blood, etc.);
- determine the source of bleeding.
With the help of endoscopy (EGD), a patient can be diagnosed with various diseases of the digestive system:
- oncological pathology;
- esophagitis;
- varicose veins of the esophagus;
- GERD;
- gastropathy or gastritis (only based on biopsy results);
- duodenitis;
- ulcerative lesions of the stomach and duodenum;
- bleeding.
Important The correct interpretation of the result obtained is of great importance. This article will help you understand the doctor’s conclusion.
Indications and contraindications
The fibrogastroduodenoscopy procedure is prescribed by a gastroenterologist, therapist, surgeon or oncologist if the patient has:
- abdominal pain of unspecified nature;
- vomiting coffee grounds or blood;
- bloody stools;
- frequent belching with a sour smell;
- constant bloating, flatulence;
- discomfort and pain when swallowing;
- polyps;
- suspected tumor of the stomach or duodenum;
- bleeding from the gastrointestinal tract.
FGDS can also be prescribed to take biopsy material from pathological areas in the stomach and duodenum, to collect gastric juice and determine acidity, to assess the effectiveness of therapy, and in the diagnosis of pyloroduodenal organic or functional stenoses.
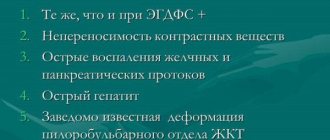
When you can’t perform FGDS of the stomach
Absolute contraindications to performing FGDS of the stomach include: agonal conditions, acute myocardial infarction and recent stroke, aortic aneurysm, as well as diseases in which it is impossible to insert an endoscope into the stomach (severe burn of the esophagus, severe cicatricial stricture of the esophagus).
Relative contraindications include:
- serious condition of the patient;
- post-stroke and post-infarction conditions;
- transient cerebrovascular accidents;
- the patient has a hypertensive crisis, exacerbation of asthma (bronchial asthma), mental illness, severe blood clotting disorders, severe diseases of the respiratory system, severe cardiovascular pathologies.
Contraindications
The procedure is contraindicated:
- with scoliosis of 4 degrees (when the internal organs are displaced);
- after a stroke;
- in acute myocardial infarction;
- patients with persistent increase in blood pressure;
- if there are congenital anomalies, tumors, due to which the anatomical position of the esophagus is disrupted;
- patients with mental disorders or epilepsy that cannot be treated with medication;
- with cicatricial narrowing of the esophagus.
How to prepare for FGDS of the stomach
Preparation for FGDS of the stomach is divided into general and local. The patient is prepared by an endoscopist who will perform FGDS. The doctor who referred the patient for examination (gastroenterologist, surgeon, oncologist) can also provide additional advice.
For reference. Poor preparation can significantly complicate or make it impossible to conduct an FGDS, so it is important to strictly follow all the doctor’s recommendations.
General preparation includes three stages:
- Conducting psychological preparation of the patient. The doctor explains to the patient the goals and objectives of the upcoming study, argues for the need to conduct an FGDS of the stomach, and explains why this study will be more informative than other methods. The doctor also explains how the procedure will be performed. Patients with increased emotional lability may be prescribed mild sedatives, sleeping pills or tranquilizers.
- Detection and correction of blood clotting disorders, diseases of the heart, blood vessels and respiratory organs. This stage is especially important, since diseases such as angina pectoris, asthma, arrhythmia, severe respiratory failure, heart failure, and arterial hypertension require special drug correction several days before the study.
- Identification of diseases that may affect the choice of drugs used in preparation for EGD of the stomach. This stage includes identifying individual intolerance to drugs used in endoscopic examinations (intolerance to some local anesthetics), the presence of glaucoma (atropine is contraindicated in such patients), gallstones (salt laxatives are contraindicated in patients). In women, it is also necessary to exclude pregnancy, since most drugs are contraindicated for pregnant women.
How is esophagogastroduodenoscopy performed?
Before the study, the main thing is not to be afraid and try to relax. If you follow all the doctor’s recommendations, the unpleasant procedure will quickly end, since a complete examination requires only a few minutes.
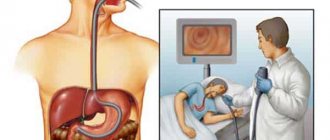
Gastroscopy is performed with the patient lying on his left side. In order to facilitate its implementation , the doctor treats the patient's throat with an anesthetic in the form of a spray (usually lidocaine is used for this). To prevent the device from biting, a mouthpiece is used. Under visual control, the specialist inserts the device into the oral cavity through the opening of the mouthpiece and then moves it along the digestive tube, examining its various parts and, if necessary, collecting tissue for analysis.
If necessary and after preliminary preparation, the patient may be given anesthesia or sedation . You can learn about the nuances of this procedure from this article. A special approach requires the administration of sedatives to a child. whether this will help make FGDS more comfortable and informative for the baby or whether it will expose it to unjustified risk.
Please note: During the examination,
you should not talk or touch the endoscope with your hands , as such actions make it difficult to carry out and may have undesirable consequences (damage to the mucous membrane of the gastrointestinal tract). It is recommended to breathe deeply and behave calmly.
How to do an FGDS of the stomach
The entire procedure for FGDS of the stomach is performed in a specialized endoscopic room. FGDS is performed by an endoscopist.
Patients wearing glasses or dentures will need to remove them before the procedure. Large earrings and chains are also removed from the neck.
After local anesthesia with lidocaine or dicaine, you need to wait five minutes until a feeling of numbness appears. Then the patient is placed on his left side and given a special mouthpiece (a plastic ring that acts as a mouthpiece). The mouthpiece must be held with your teeth and lips.
The endoscopic tube is inserted through the mouthpiece. During insertion of the endoscope, it is recommended to relax your throat as much as possible and breathe slowly deeply.
When the endoscope is inserted to the root of the tongue, the doctor asks the patient to swallow the tube. Free movement of the hose and absence of coughing indicate that the endoscope is in the esophagus. There is a slight resistance as the tube moves into the stomach.
After inserting the endoscope into the stomach, the doctor examines its mucous membrane on the monitor. If necessary, the study may be recorded.
If a pathological focus is identified, the doctor can perform a biopsy (take tissue for further research). Also, according to indications, chromoscopy, removal of polypous formations, stopping bleeding or administering medications can be performed.
If additional examination of the duodenum is necessary, after examining the stomach, a probe is inserted into the intestine. The inspection results are also displayed on the screen and, if necessary, recorded.
How long does FGS last?
The duration of the procedure refers to the time from the moment the endoscope is inserted until it is removed. FGS lasts from 5 to 15 minutes (FGDS will take a few minutes longer).
If complex medical procedures are additionally performed, then the endoscopy time can last, on average, up to 30–40 minutes.
For reference. After the usual FGDS, the patient is recommended to lie down or sit for a while (5-10 minutes). After this, the patient can go home or to his room.
If polyps were removed or a biopsy was performed during FGDS, the time the patient spent in the department will depend on the main diagnosis and the scope of the intervention performed.
Indications for research
To understand what such research methods are and what their differences are, it is necessary to understand the indications for their use. Esophagogastroduodenoscopy is indicated if there are suspected pathological foci of the esophagus, small intestine, or stomach. That is, if the patient has symptoms that indicate the presence of diseases of these organs:
- belching;
- heartburn;
- discomfort when swallowing food;
- sensation of cutting in the esophagus.
Using a probe, you can accurately determine the presence of scars, obstruction at the junction of the mouth into the stomach, fistulas, diverticula, and neoplasms. Further, as the probe passes through the digestive system, gastroscopy allows the detection of erosions, bleeding, ulcerative lesions, tumor processes, diverticula of the small intestine, and stomach. Fibrogastroduodenoscopy is carried out to determine pathological foci of the duodenum and stomach.
Most often this is:
- varicose veins;
- ulcerative lesions;
- gastritis;
- diverticula;
- duodenitis;
- esophagitis;
- reflux;
- neoplasms.
The most common symptomatology for which the study is carried out is the appearance of nausea after eating and pain in the stomach. As the disease progresses, the list of clinical pictures expands, adding:
- unexpected weight loss when eating a diet characterized by sufficient calorie content;
- loss of appetite;
- flatulence.
It turns out that the differences between these research methods lie in the advantage of endoscopy, which appears due to the diagnosis of the esophagus. Fibrogastroscopy does not provide this opportunity.
Is it painful to have a gastroscopy?
Most patients who have undergone FGDS in the traditional way, if asked to describe their feelings from the procedure, call it unpleasant.
To reduce the severity of these sensations, a local anesthetic is used, which is applied to the back wall of the oropharynx. However, it does not always save the patient from discomfort.
The most common complaints from patients:
- nausea;
- a feeling of discomfort in the neck, behind the sternum or in the abdomen;
- increased salivation;
- belching;
- feeling of lack of air;
- panic attacks;
- aching or cutting pain in the neck or abdomen.
For reference. Oddly enough, pain syndrome is relatively rare. It is possible in the presence of acute pathology (for example, exacerbation of peptic ulcer disease in young patients), complications (wall perforation) or careless examination, however, swallowing the intestine to check the stomach is unpleasant.
The main thing is to behave correctly during the procedure and listen to the doctor’s recommendations.
Choosing the right doctor
Choosing a qualified doctor with a friendly approach to his patients can significantly reduce anxiety before the procedure, as well as reduce the severity and frequency of side effects.
A good approach from a specialist relieves anxiety and helps the patient relax. This allows the procedure to be carried out without unnecessary trauma (for example, scratching the throat), since the probe advances more easily.
In clinical practice, there are situations when, due to low professionalism, the doctor applies the wrong or insufficient anesthetic. Also, some medical professionals do not explain the essence of the procedure, possible risks, and nuances of patient behavior.
Important. The doctor must carefully explain the nuances of preparing for the study, as well as select the most appropriate method of performing the procedure (nasal insertion of a probe, sedation or anesthesia) for a particular patient.
Breathing feature
Before starting the procedure, the doctor must explain to the patient how to breathe correctly during FGDS. Breathing should be through the nose, deep and smooth. In this case (despite popular belief) there is no need to swallow while moving the endoscope through the oropharynx and larynx.
Preparation
Preparation for these research methods does not have any differences, which is associated with the diagnosis according to the same scheme. For 3 days before the procedure, the patient should adhere to a special diet, which is aimed at eliminating the consumption of fried, fatty, smoked, spicy, and canned foods. It is important to focus on liquid, well-digested, crushed food. There is also an emphasis on small but frequent meals, in small portions at least 5 times a day. This will help improve the digestibility of foods.
If a patient has a digestive disorder, he is prescribed enzyme agents during the preparatory period. Because during the procedure the stomach must be empty. You must come for the examination on an empty stomach. The last meal should end at 19:00 with a light dinner. It is also forbidden to drink water in the morning. This will help avoid the appearance of a gag reflex during diagnosis.
Complications after the procedure
For reference. FGDS of the stomach is a safe procedure. Complications after the procedure are extremely rare and do not pose a threat to the patient’s health or life.
The main complications are sore throat and discomfort after removing the endoscope. There may also be discomfort in the abdomen due to the entry of air. After belching air, the discomfort disappears.
When a biopsy is taken, slight swelling and discomfort in the epigastric region may be observed for several days.
More serious complications are rare. Minor bleeding may be due to damage to the esophageal mucosa by the endoscope.
Perforation of the wall of a hollow organ (esophagus, stomach, duodenum) can be observed in patients with large ulcers of the mucous membrane and gastrointestinal tract.
Bleeding may also occur after endoscopic removal of polyps. Most often, bleeding stops on its own, or after drug or endoscopic hemostasis.
Decoding concepts
EGDS (gastroscopy, esophagogastroduodenoscopy) is a study of the upper parts of the digestive tract (esophagus, stomach, duodenum) using a special device called an endoscope. It allows you to examine this part of the digestive system from the inside and make a diagnosis with maximum accuracy. Moreover, modern endoscopy is not limited only to examination ; if necessary, it is accompanied by a biopsy (tissue sampling for morphological examination) and a urease test (detection of H. pylory).
If the complex name of this diagnostic procedure “esophagogastroduodenoscopy” is broken down into its component parts and translated from Greek and Latin, then it will not look so scary: oesophagus (esophagus) - esophagus, gaster - stomach, duodenum - duodenum, skopeo - look.
The essence of the research method
, endoscopes with different technical characteristics and resolution were used for endoscopy
- hard;
- semi-rigid;
- flexible;
- fibrogastroscopes;
- video endoscopes;
- Ultrasonic endoscopes.
Recently, only the last 3 have been used in medicine.
A fibrogastroscope is a flexible endoscope equipped with fiber optics. Translated from Latin: fibra is fiber, gastro is stomach, skopeo is to look. It is this device that is used for FGDS (FEGDS, fibroesophagogastroduodenoscopy).
FGDS is a gastroscopy method that provides the opportunity to examine the same upper parts of the gastrointestinal tract using a fibrogastroscope.
Alternative research methods
For reference. Only capsule endoscopy can be considered a direct analogue of FGDS, but this method is very expensive, and with capsule endoscopy it is not possible to take material for research.
This endoscopic research method involves the advancement of a special capsule that contains a microvideo camera through the gastrointestinal tract. The patient is asked to swallow it, after which an image appears on the monitor.
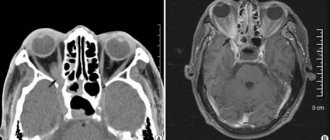
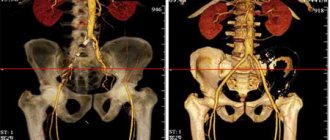
Alternative methods also include:
- Ultrasound of the abdominal organs;
- X-ray with contrast;
- tomography.
Contrast x-rays are the most popular. The risk of misdiagnosis is about 15%.
What determines?
The study allows us to study in detail the mucous membrane of the gastrointestinal tract, their anatomical features and identify pathological changes, such as:
- the presence of an inflammatory process;
- erosions, scar changes, ulcers;
Peptic ulcer is the most common gastrointestinal disease
- bleeding;
- neoplasms.
The study is also carried out to detect Helicobacter bacteria and to monitor the effectiveness of treatment of various pathologies.
Interpretation of gastroscopy results
To decipher the results of the examination, you need to decide what the normal indicators are and do a comparative analysis. Standards have been established for each digestive organ.
Indicators of the norm of the digestive organs of a healthy person:
- Esophageal mucosa. It is necessary to pay attention to color and structure. In a healthy person, the color of the esophagus should be pink or red, and the structure should be finely fibrous; the length of the esophagus should be 25-30 centimeters.
- Stomach. It has a brighter color than the esophagus, usually red. One side of the stomach is smooth, and a small amount of mucus is allowed. The other side has a folded appearance.
- Duodenal mucosa. This is a small tube with a circumference of up to 3.5 centimeters. The shell color is light pink. There is one fold, two ducts - bile and pancreatic. The ducts are connected to the gallbladder and the pancreatic gland.
Indicators of the stomach and intestines with pathology
Indicators are cause for concern if detected during examination.
- With gastritis, the gastric mucosa swells, pinpoint hemorrhages or erosions, a significant amount of mucous substance and an increase in the number of folds on the lining are detected.
- In case of a stomach ulcer, examination immediately reveals ulcerative formations, their shape and color characteristics. The ulcers usually have the shape of a convex ridge; the bottom of the ulcer contains a white coating.
- In the presence of a tumor or cancer of the stomach, smoothing of the longitudinal folds is observed, the color of the mucous membrane acquires a white or gray tint. During the examination, if there are neoplasms, they are immediately visible, even small ones up to 1 mm.
It is important to realize that the interpretation of gastroscopy results is done by a qualified specialist in order to avoid mistakes. There are many pathological changes that only the attending physician can see.
Indications for gastroscopy
Gastroscopy is one of the informative ways to diagnose pathologies of the digestive organs. If there is a need to confirm or refute the diagnosis of gastrointestinal diseases, an endoscopic procedure is prescribed. Indications for endoscopy:
- Feeling of discomfort in the stomach after eating;
- Frequent heartburn;
- Causeless nausea;
- The digestive tract is disrupted;
- Vomiting, unpleasant taste in the mouth;
- Sudden weight loss;
- The patient complains of acute abdominal pain;
- In case of swallowing dysfunction (dysphagia), esophagoscopy is recommended;
- To detect the presence of Helicobacter bacteria;
- Accurate diagnosis of gastritis;
- Suspicions of ulcers, inflammatory processes;
- Examination of the gastrointestinal tract for tumors and neoplasms;
- For internal bleeding of the stomach;
- For pancreatitis (inflammation of the pancreas), hepatitis (liver disease).
Endoscopy is useful for the prevention of diseases of the abdominal organs and timely detection of pathologies at the initial stage. The method used is esophagoscopy (the upper parts of the gastrointestinal tract are studied).
Preparing for the examination
Before a medical examination, consultation with a doctor is required. To ensure the reliability of the results, the patient prepares for the examination. Preparatory activities (for FGDS, EGDS, FGS):
- Ask a gastroenterologist about the rules and process of endoscopy, contraindications, what the consequences are, and whether there is a replacement method for diagnosis.
- Collect the necessary tests; it is recommended to undergo a blood clotting test.
- If there is one, take an ultrasound report of the abdominal cavity, MRI, or x-ray.
- Before the procedure, you need to inform your doctor about any allergies to medications and what medications you are currently taking.
- Two to three days before the examination, a diet plan is prescribed. The consumption of alcohol and medicinal tinctures containing alcohol is prohibited, and smoking should be stopped.
- Endoscopy is performed on an empty stomach. It is better not to drink liquid on the day of the examination.
- To eliminate pain when inserting a probe, use Lidocaine. This helps reduce gagging and discomfort during the procedure.
The patient must strictly follow the recommendations and prescriptions of the gastroenterologist.
How is gastroscopy done?
Before the medical examination, the nurse will numb your throat with lidocaine spray. The study is done in the morning. The treatment room is equipped with the necessary apparatus and instruments for research.
- Before the procedure, the patient must read and sign the hospital form. If the test results are normal, you can begin the examination.
- The procedure is carried out on a couch. The patient is placed on his left side.
- The doctor places an endoscope (gastroscopy device) into the mouth (or nose). Then it is carefully advanced into the esophagus for examination. The device has a microcamera that allows you to visualize internal organs for diagnostics. The procedure is painless, but it causes discomfort and may cause vomiting.
- It is recommended to relax and establish a calm breathing rhythm. This will make you feel better.
- You cannot talk, stand up, roll over, pull the probe with your hands or pull it out. There is a risk of damaging the mucous membrane and causing internal bleeding.
- Listen carefully to the doctor and follow the recommendations during the examination.
- After completing the examination, the gastroenterologist removes the probe. There may be unpleasant sensations in the throat after removing the device, discomfort in the abdomen.
- The sample study can be written to disk. The result is processed by a doctor, a protocol is drawn up, after which an accurate diagnosis is reported and appropriate treatment is prescribed.
- After the examination, the patient is advised not to eat food for 3-4 hours, on the first day to drink warm water, you can take a teaspoon of sea buckthorn oil.
- Possible complications after FGDS in the form of nausea, stomach pain, vomiting. Carrying out the procedure is not harmful to health.
If during the procedure the condition has deteriorated significantly, you should abandon gastroscopy and find alternative diagnostic methods (radiography, ultrasound examination).
How is EGDS done?
The EGDS procedure is performed in a gastroenterologist’s office in a clinic or day hospital. Before the examination begins, the doctor examines the patient’s mouth and throat, after which he performs premedication: he irrigates the throat and root of the tongue with local anesthetics to reduce their sensitivity and avoid the urge to vomit during insertion of the device. After this, the patient is placed on the couch on his side.
The examination is carried out according to a single algorithm:
- A mouthpiece is inserted into the patient's oral cavity - a tab that will prevent the jaws from completely closing. In the middle of it there is a hole into which the doctor inserts a gastroscope tube.
- After inserting the tube into the oral cavity, the patient is asked to relax the larynx and throat, lower the tongue so that the device can easily penetrate the esophagus. Sometimes the doctor asks the patient to make swallowing movements. If the urge to vomit occurs, the patient is asked to breathe slowly and as deeply as possible. This technique reduces nausea.
- After inserting the tube into the esophagus, the doctor begins supplying air to expand its cavity and thoroughly examine the mucous membranes. At this moment, the patient may feel fullness, and after moving the gastroscope deeper, a kind of belching may appear.
- After examining the esophagus, the doctor gradually inserts the gastroscope tube into the stomach, and then into the duodenum. All this time he turns the tube to examine all the surfaces of the organs. At the same time, photographs are taken or video is recorded.
If necessary, during esophagogastroduodenoscopy, the doctor measures the acidity of gastric juice and the contents of the duodenum, and takes a pinch of the mucous membrane for histology.
How long does esophagogastroduodenoscopy take?
A typical survey esophagogastroduodenoscopy lasts no more than 5 minutes. The procedure may take a little longer, during which the doctor will have to measure the acidity of the stomach. The longest diagnostic process awaits patients who require a biopsy. This study lasts up to 15-20 minutes.
Is it possible to use anesthesia for endoscopy?
Conducting studies with anesthesia during endoscopy is not widespread, since the procedure is generally painless and takes little time. The exception is children under 10 years of age. They always undergo esophagogastroduodenoscopy under sedation. This is a special type of anesthesia in which the patient is immersed in a short but deep sleep. Drugs that are used for endoscopy while the patient is asleep act more gently and have fewer side effects and contraindications.
Important! An examination under anesthesia is carried out for adult patients if they have a reduced pain threshold, an increased gag reflex, or severe mental instability.
Nausea during the procedure
To reduce nausea before EGDS, the doctor may prescribe prokinetics Motilium or Cerucal. If their effect is insufficient and when the tube is inserted there is a urge to vomit, interfering with a normal examination, the procedure may be postponed or esophagogastroduodenoscopy may be continued using general anesthesia.
What reveals
Esophagogastroduodenoscopy shows almost any changes in the condition of the mucous membranes of the digestive tract:
- changes in the structure of the mucous membranes - erosion, stomach ulcers, erosive bulbitis and others;
- foci of inflammation, irritation of the mucous membranes of the esophagus and stomach;
- protrusions on the walls of the esophagus (diverticula);
- varicose veins of the esophagus;
- inflammatory processes on the mucous membranes - cholecystitis, bulboduodenitis, antral gastritis and others;
- changes in the functioning of valves and sphincters - reflux and their consequences;
- neoplasms - polyps, malignant tumors;
- foreign objects;
- sources of bleeding.
In addition, the doctor can assess the functional state of individual parts of the digestive tract.
When are these diagnostic methods prescribed?
For the patient himself, there is no significant difference in which method the functional study is performed: fibrogastroduodenoscopy or esophagogastroduodenoscopy. Both methods require the same preparation steps:
- the patient must avoid eating at least 6 hours before insertion of the probe;
- 2 hours before gastroscopy, do not even drink clean water;
- if there is a need to take pharmaceutical drugs, it is better to choose a form of medication suitable for resorption.
The sensations during the procedure are also identical. The patient lies on his side, the doctor numbs the throat area using a special spray with lidocaine, and then inserts a flexible probe, controlling the depth of insertion and examining the tissues on the device monitor. Gastroscopy causes discomfort due to the gag reflex that occurs, but with proper breathing and emotional state, discomfort can be minimized.