Karyotype analysis can be done by people who would like to check the health of themselves and their future offspring. Modern medicine is able to detect many diseases, including genetic ones. Despite the fact that DNA tests are not mandatory, in some cases it is still advisable to take them. Timely diagnosis will allow the development of protective measures. In this article we will talk about one of the studies that is shown to couples at the stage of pregnancy planning to identify hereditary diseases.
What is this karyotyping procedure?
A person’s chromosome set affects his appearance, as well as the functioning of the body. It is called a karyotype. If it is not standard, a dangerous pathology may develop. Genetic diseases cannot be cured; their manifestation can only be somewhat reduced. To understand whether there are any damage to the DNA, a special analysis is done. Venous blood is taken for this. The results will show the compatibility of husband and wife, their ability to bear and give birth to children, and the likelihood of how healthy the offspring will be.
The study is not included in the list of mandatory, it is only recommended. Many couples decide to get tested themselves; others are advised by their doctor to do so. The cost of the procedure varies greatly in different medical institutions, the price also depends on the number of mutations that will be looked for in the laboratory.
What can and cannot be determined by this study?
Analysis of the patient's karyotype shows the presence of various chromosomal diseases, which are called chromosomal diseases. A variety of troubles can happen to chromosomes: the patient may have more or fewer chromosomes, their structure may be disrupted, and the karyotype may be duplicated, or there may be a completely extra chromosome set in each cell.
In some cases, at the earliest stage of embryo development, a “failure” occurs at the stage of egg fragmentation. As a result, such an organism, developed from an incorrectly developed zygote, will contain several cell clones, and even several different karyotypes. This rare condition is called mosaicism by geneticists.
Severe karyotype abnormalities are accompanied by very serious developmental defects and incompatibility with life. Spontaneous abortions or stillbirths usually occur under these conditions. But still, about 2% of children with chromosomal disorders are born, grow, develop and can live quite a long life and even give birth to children. Karyotype examination can show the presence of such diseases.
But with all this, a karyotype cannot show whether a person is sick or not with a disease that is associated with a defect in a single gene, as opposed to chromosome defects. Karyotyping shows only the most severe abnormalities at the chromosome level. This test cannot detect diseases such as phenylketonuria, galactosemia, Marfan syndrome, or severe diseases such as cystic fibrosis. This requires genetic studies (rather than cell microscopy), for which other techniques are used.
To put it in very simple words, we can compare the situation to a parade of troops. From a height you can clearly see individual battalions marching in the shape of even rectangles, and if any battalion has fewer people (gross defect), then either the rectangle will be smaller or its shape will be irregular, and this can be compared to a chromosomal pathology, if the battalion itself is taken as one chromosome. But the problems associated with an individual soldier (gene) cannot be seen from such a height. He may have a weapon taken differently, he may not have a collar or headdress, but in general the situation will look harmonious from afar. Therefore, problems associated with one soldier, or with one gene, are solved by other research methods, for example, genetic sequencing. Now you know what finger karyotyping is.
For whom is the procedure necessary?
The analysis is recommended for people who have an increased risk of problems. In particular, research can be of great help in various situations.
Who is prescribed
- If a couple over the age of 35 wants to have a child. The recommendation applies even if only one of the spouses has crossed the age threshold. After 35 years of age and beyond, people's health undergoes changes and can deteriorate significantly. Those genetic abnormalities that were previously dormant in the body are often activated and, accordingly, can affect pregnancy and gestation. A blood karyotype test shows whether this situation is likely in a particular case or not.
- For infertility, the causes of which cannot be determined. It happens that a couple works for many years to conceive, but does not get results. If everything is normal with hormones and the functionality of the genital organs, the reason may be genetic incompatibility. If this is so, then the couple will never be able to have children together. This does not mean that the spouses are infertile. Sometimes changing your partner can solve the problem. Sometimes only one of the spouses is genetically infertile. Then the couple is offered to use donor reproductive material to conceive.
- After repeated IVF, which was unsuccessful. In vitro fertilization never guarantees 100 percent success, but if it doesn't help a little, it means the couple has serious health problems. The likelihood that bad genetics is to blame is high.
- If the husband, wife or their relatives have a hereditary disease. The mutation that led to it could well be passed on to descendants, but not necessarily.
- If a woman has hormonal problems of unknown nature.
- Impaired sperm production due to unknown reasons.
- If the couple lives in a region with an unfavorable environmental situation.
- If the husband or wife works with hazardous chemicals.
- After radiation, beam exposure and chemotherapy.
- If there have been frozen pregnancies, miscarriages, or premature births in the past. This is caused by thrombosis in the vessels of the umbilical cord, which is a consequence of gene reversion. In this case, special medications will help save the baby.
- If the marriage was concluded between close blood relatives. A coincidence of chromosomal damage is very likely, which will lead to severe disorders in the offspring.
- The birth of children with congenital pathologies in a family. If this happened, it is important to find out the reasons for what happened. If they are related to DNA, then it is necessary to calculate the risks for the next child.
As a rule, a blood test for karyotype is carried out before pregnancy, at the planning stage. This allows you to calculate all risks in advance and decide on further actions.
If conception has already occurred, it is not too late to conduct research. For him, biological samples will be taken not only of the father and mother, but also of the embryo. This will allow you to find out the likelihood of successful pregnancy, as well as the health of the fetus.
To whom and why is karyotyping indicated?
The test is used to detect chromosomal abnormalities and is thus used to diagnose genetic diseases, some birth defects, and diseases of the blood or lymphatic system.
Prenatal period
Analysis of the fetal karyotype is carried out in the following cases:
- if one or more screening tests during pregnancy (in the first and second trimesters) showed abnormal results;
- if structural anomalies and/or pathologies of fetal development are detected during an ultrasound;
- if there are diagnosed chromosomal abnormalities among family members.
Karyotyping of spouses
Analysis of the karyotype of spouses during pregnancy planning is used under certain conditions:
- for couples with the same hereditary history of a genetic disease;
- when one partner has a genetic disease;
- if one partner is known to have an autosomal recessive mutation (one that can cause disease in an unborn child only if both partners carry the same mutation).
Couples who either fail to conceive or experience repeated miscarriages may also undergo karyotyping if all other causes have been examined and ruled out.
How is the procedure performed?
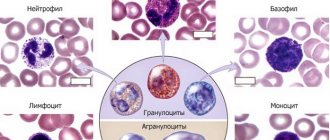
Blood is taken from both spouses, then it is processed in a special way. First, lymphocytes are separated. They are isolated at the stage of division (called mitosis). Next, the cells are treated with a special substance that stimulates their reproduction. This process will be observed by specialists, noting its correctness. This takes approximately 3–5 days.
During observations, chromosomes are stained. This is done in order to clearly see all fragments of the genome. When painted, they are clearly visible. The existing pairs are compared with the norm. Based on this, a map is drawn up, and genetic health is judged from it. For such a study, only 12 maximum 15 lymphocytes are sufficient. No more is needed, because the blood cells are then multiplied in artificial conditions.
Modern diagnostic capabilities in karyotype research. Research methods
Karyotyping involves determining and assessing the size, shape, and number of chromosomes in a sample of body cells to identify both numerical and structural defects.
Research stages
Sample collection
Theoretically, the test can be performed on any body fluid or tissue, but in clinical practice, samples are obtained in four ways:
- Amniocentesis involves inserting a needle into a pregnant woman's abdomen to obtain a small amount of amniotic fluid from the uterus; this is performed under ultrasound guidance to avoid harm to the fetus. The procedure is performed between 15 and 20 weeks of pregnancy. The procedure is relatively safe, but increases the risk of miscarriage.
- Chorionic villus sampling also uses an abdominal needle to extract a sample of cells from the placental tissues. The procedure is performed between 10 and 13 weeks of pregnancy and also increases the chance of miscarriage.
- Taking a blood sample. It is usually obtained from a vein in the arm. The blood is then exposed to ammonium chloride to separate white blood cells for testing.
- Bone marrow aspiration can be used to diagnose chronic myeloid leukemia. Under local anesthesia, a needle is inserted into the center of the femur and material is collected.
Photo: https://www.pexels.com/photo/person-getting-his-blood-check-1350560/
Cell separation
To study the karyotype, actively dividing cells are required, such as leukocytes and most embryonic cells. Using special chemicals in a cytogenetic laboratory, they are separated from non-dividing cells.
Growing Cells
The study requires a large number of cells. For this purpose, they are grown in a special medium containing hormones and chemical elements that favor cell division and reproduction. This process takes 3–4 days for blood cells and up to 7 days for embryonic cells.
Cell synchronization
Chromosomes are a long strand of DNA. To be seen under a microscope, they must be at their most compact shape during metaphase (division stage). For this purpose, cells are treated with a special substance that stops division at the moment when the chromosomes are most compact.
Extracting chromosomes from their cells
To examine chromosomes using a microscope, they must be removed from cells. A special solution is applied to the cells, leading to their destruction. This way, cell debris is washed away and the chromosomes remain stuck to the slide.
Coloring
Chromosomes have no color. To distinguish them from each other, a dye is applied to the glass slide. When stained, each chromosome has a specific pattern of light and dark bands, allowing chromosomes to be differentiated. Each dark or light stripe contains hundreds of different genes.
Analysis
After staining, the chromosomes are examined using a microscope. The specialist determines the number and structure of chromosomes, and the chromosomes are arranged by size.
Photo: https://pixabay.com/illustrations/mitosis-meiosis-cell-cell-division-3876669/
Methods for studying karyotype
Classical karyotype analysis
With this type of study, chromosomes are stained with various substances.
| Type of staining | Dye | Purpose of application | Peculiarities |
| Q | Akrikhin mustard | Analysis of genetic sex, identification of translocations between X and Y, Y and autosomes, screening for mosaicism with Y chromosomes | Gives a highly detailed image. Diagnosis is carried out under a fluorescent microscope |
| G | Giemsa dye solution | Detects minor abnormalities, marker chromosomes | Standard method of cytogenetic analysis. Highly sensitive compared to Q |
| R | Acridine orange dye | Used to determine G and Q negative sections | Parts of chromosomes that do not show sensitivity with G-staining are stained. |
| C | Alkali | Analysis of the central part of chromosomes | The dye affects only the centromeric and pericentromeric parts of all chromosomes and the long arm of the Y chromosome |
Spectral method
Chromosomes are stained with fluorescent dyes that are deposited in certain areas. The method makes it possible to identify translocations between chromosomes, since the translocated parts differ in spectrum from the other chromosome.
Carrying out the test
The control can be carried out on a couple or a child. These are different manipulations, we will consider them below.
For spouses
If a husband and wife have had the unfortunate experience of an unsuccessful pregnancy, it is logical that they want to be rechecked before the next conception. In case of long-term infertility, it is also worth undergoing karyotyping of blood cells; we will discuss what this will give in practice in one of the following sections. This type of study of biological fluid is traditional. There are also more modern techniques that allow you to determine genetic risks. This:
- SKY. In this analysis, chromosomes are stained in 24 colors at once. This allows you to determine even those pathologies that are not detected using the conventional method. The examination is done in a short time, which is also a plus.
- FISH. Captures a huge number of violations. The test is the most informative of the existing ones. During its implementation, fluorescent staining is used. Cell cultivation is not necessary to obtain results, thus the time required to obtain results is reduced. For people who don't want to wait, this is it. The procedure is also performed during pregnancy. For manipulation, maternal venous blood is collected or fetal genetic material is selected.
The first method is non-invasive, it is safer, since it does not directly affect the child in any way. The second involves puncture of the uterus (there is no other way to collect biological material). This is a dangerous procedure, the positive outcome of which is approximately 50 to 50. After such an intervention, the embryo may die right in the womb. There is also a chance that a spontaneous miscarriage will occur. How advisable such a risk is is for parents to decide.
Carrying out the test in newborns
The study is done in the maternity hospital. For this purpose, blood is taken from the baby. If deviations from the norm are detected, parents are notified. They are offered to undergo a full genetic examination. You can refuse examination in the maternity hospital. Before doing this, it is worth considering whether such a step is justified. Many DNA disorders clearly make themselves felt in early childhood.
For example, Down syndrome is already noticeable in the maternity hospital with the naked eye. It is recommended that older children also be examined if they have disturbing symptoms. In particular, you should be wary of the following:
- Mental retardation or physical impairment, the cause of which is not clear. It happens that not everything is all right with the baby, but tomograms, ultrasound of the brain, and all kinds of tests show that everything should be fine. In such a situation, there is a high probability that the cause of the condition is in the genome.
- Delayed or accelerated sexual development.
- An anomaly that makes you doubt your gender (This is called hermaphroditism).
You can check your DNA at any age; there are no contraindications to manipulation.
Recording karyotypes
The karyotype record carries a certain characteristic of it. First, the total number of chromosomes is indicated, then the set of sex chromosomes. If there are mutations, genomic ones are indicated first, then chromosomal ones. The most common ones are: + (extra chromosome), del (deletion), dup (duplication), inv (inversion), t (translocation), rob (Robertsonian translocation).
Examples of recording karyotypes:
48, XY - normal karyotype of a male chimpanzee;
44, XX, del (5)(p2) - karyotype of a female rabbit in which division of the second section of the short (p) arm of the fifth chromosome occurred.
Preparing for a karyotype test
Blood cells are needed for the study. It is important that they are in their normal condition at the time of collection. This will ensure that the result is informative. In order for the blood values to be as close to real as possible, it is important not to take any medications two weeks before the donation. Not only medications should be excluded, but also vitamins, dietary supplements, and nutritional supplements. A test done during chemotherapy will not be informative, because the heavy drugs used in this case tend to damage DNA.
It is also undesirable to get sick during this period. If one of the spouses catches the infection, the procedure should be postponed. There's nothing wrong with that. It is better to find out the exact results later than to rush and get a questionable answer. Biological fluid is collected on a full stomach. This feature should be remembered. Experts recommend eating something an hour or two before the procedure.
Reviews
Elena, 33 years old: “After two unsuccessful IVF attempts, a karyotype test was prescribed, we did it, everything seemed to be in order, without any anomalies. However, the doctor said that it was not the same, it was an aberration. Supposedly, only he can make pregnancy predictions.”
Anastasia, 30 years old: “The cause of infertility was found: karyotyping showed 46,X[delXp–] - suspicion of Shereshevsky-Turner syndrome. This means that without a donor egg there is no way. “At the same time, there are no external manifestations, I am healthy.”
Oleg, 41 years old: “Based on the results of karyotyping, the doctor immediately suggested IVF with preimplantation diagnosis of the fetus, since the disorders were serious. I have 45 chromosomes, with 13 and 14 intertwined. High risk of having a child with Down syndrome or frozen pregnancy.”
What does a karyotype analysis show: why is it taken?
There are 46 pairs of chromosomes in human DNA. Sexual factors are added to this amount - XY in women and XX in men. If a mutation occurs in the genome, various variations are possible. Scientists have studied many of them, which has allowed them to diagnose genetic diseases.
Data Decoding
A karyotype study (see what it is in the previous sections) can identify the following pathologies:
- Mosaicism. This is a phenomenon in which the cells of the human body are carriers of different genomes.
- Translocation. With it, fragments are exchanged.
- Deletion. This is the loss of a piece of the genome. Most often, it is with such a mutation that serious disorders occur.
- Monosomy. The loss of one whole couple.
- Trisomy. Adding an extra unit. With such a mutation, for example, the development of Down syndrome occurs.
- Inversion. With it, the molecules turn 180 degrees. In such a situation, they do not work as they should.
When drawing up an individual map, they take into account which pair the mutation occurred in. In particular, changes in 21 points indicate Down syndrome, in 18 - Edwards syndrome. If the sexual pairs are damaged, this usually means infertility (female or male). Each of the listed deviations comes in different types. A detailed interpretation of the karyotyping analysis can be done by a geneticist. A shortened fifth chromosome causes cry-the-cat syndrome.
In addition to severe disorders, it shows a predisposition to diseases such as hypertension, joint damage, diabetes mellitus and others. Such information will not be superfluous. Knowing what problems may await your baby in adulthood, you can adjust his lifestyle and reduce the risks accordingly. Sometimes the analysis shows that there is no pathology, but there is a risk of its occurrence in the offspring, especially if the husband and wife have the same tendency to some mutation. In this case, it is important to take responsibility for planning the birth of children.
Abnormal karyotype. Chromosomal diseases
Karyotype examination allows identification of both numerical and structural defects. While quantitative abnormalities involve either too few or too many chromosomes, structural abnormalities can cover a wide range of chromosomal deficiencies.
Structural anomalies
Changes in chromosomal structure can take several forms:
Translocation
Involves the transfer of material from one chromosome to another. Occurs in 1/500 live births. Translocations can be inherited from a carrier parent or occur de novo without other family members being affected.
There are two main types of translocations.
- Reciprocal - exchange of segments from two different chromosomes. Carriers of the reciprocal translocation are usually phenotypically normal, but they have an increased risk of miscarriage.
- Robertsonian translocation - the entire chromosome is attached to the central part of another chromosome. Carriers of Robertsonian translocations are usually phenotypically normal. However, they have an increased risk of miscarriage and having a child with a chromosomal abnormality.
Rarely, translocations may involve 3 or more chromosomes. Another, less common type is an insertional translocation , where a piece of chromosomal material is broken and then reinserted into the same chromosome at a different location or attached to a different chromosome.
Inversion
During inversion, one chromosome breaks at 2 points; the broken piece then flips over and attaches to the same chromosome. Inversions occur in 1 in 100 babies.
There are 2 types of inversions:
- pericentric - breaks are located on 2 opposite arms of the chromosome and include the central part. This type of inversion is usually detected because it changes the position of the centromere;
- paracentric - ruptures occur in only 1 shoulder.
Carriers of such structural abnormalities are usually phenotypically normal, but they are at increased risk of miscarriages, usually with paracentric inversions, and the birth of chromosomally abnormal offspring with pericentric inversions.
Deletion and duplication
Deletion involves the loss of chromosomal material and, depending on their location, they can be classified as terminal (at the ends of the chromosomes) or interstitial (at the arms of the chromosome). They can be isolated or occur together with a duplication of another segment of the chromosome. The deletion is usually associated with mental retardation and developmental defects.
Photo: https://pixabay.com/photos/puzzle-dna-research-genetic-piece-2500333/
Lejeune syndrome (LS)
The absence of the short arm of chromosome 5 is the cause of CS (cry-the-cat syndrome), with a characteristic cat-like cry in early childhood due to tracheal hypoplasia.
Other clinical signs include:
- low birth weight;
- postnatal failure to develop;
- hypotension;
- microcephaly (shrinkage of the skull);
- ocular hypertelorism (increased distance);
- epicanthal folds;
- downward tilt of the palpebral fissures;
- low-set, ugly ears;
- congenital heart defects and other developmental anomalies.
The clinical severity of the syndrome depends on the size of the chromosome deletion. Larger deletions are associated with more severe expression. The deletion is usually found on chromosome 5, inherited from the father.
Williams syndrome (WS)
SU is associated with a small deletion of chromosome 7. Congenital heart defects are observed in 80% of affected children. Although these children often have a normal birth weight, they have growth retardation. They have a characteristic facial appearance ("elf face"):
- broad forehead;
- short nose with a wide tip;
- full cheeks;
- wide mouth with full lips.
Many children have dental problems (small, widely spaced, crooked or missing teeth). In older children and adults, the face appears longer and more gaunt.
Mild mental retardation (average IQ ranging from 50 to 60) is common, but developmental testing reveals strengths in personal social skills and weaknesses in cognitive areas. Hypercalcemia is present in newborns. People with SU often have a vibrant personality (talkative and outgoing). However, approximately 10% of children with AS have features of autism spectrum disorder. Patients sometimes have unusual musical abilities (about 20% have absolute or ideal pitch).
Photo: https://ovp1.ru/genetic/vilyamsa
Chromosome 22 deletion syndromes
The absence of chromosome 22 is responsible for a group of conditions. Common signs include:
- dissection of the palate;
- insufficiency of the velopharyngeal ring;
- characteristic facial appearance (protruding nose and wide nasal root).
Speech and language difficulties are common, as is mild mental retardation. A wide range of mental disorders, including schizophrenia and bipolar disorder, were observed in more than 33% of affected adults.
Duplication of chromosome 15
Children with this disorder typically have varying degrees of developmental disabilities and autism spectrum disorder; seizures are common, as are behavioral problems. The phenotype demonstrates minimal dysmorphic features.
Isochromosomes
Isochromosomes consist of 2 copies of the same chromosome arm, connected through one central part and forming mirror images of each other.
Ring chromosomes
Ring chromosomes are rare. It is formed when both ends of a chromosome are removed and then joined to form a ring. Depending on the amount of chromosomal material that is missing or in excess (if the ring is in addition to normal chromosomes), a patient with a ring chromosome may appear normal or nearly normal, or may have mental retardation and multiple congenital anomalies.
Quantitative deviations (aneuplodia)
Abnormalities in the number of chromosomes occur due to random errors in cell division caused by rapid development and intensive division in the early stages after fertilization. In some cases, an extra copy of a chromosome is created (trisomy), or the cell may have only one chromosome (monosomy).
Trisomy
Trisomy has an extremely serious impact on the further development of the unborn child.
Trisomy can manifest itself in several ways:
- complete - a copy of the chromosome is present in all cells;
- mosaicism - an additional chromosome is present only in some cells;
- partial - cells have only part of the third chromosome.
Down syndrome (DS)
Photo: https://www.flickr.com/photos/shebalso/8130193355/
DS is the most common quantitative chromosome disorder, in which there are three copies of 21 chromosomes. The anomaly occurs in 1 out of every 1000 births.
DM is most often diagnosed during the newborn period. Children usually have normal weight and length at birth, but hypotonia is present. Characteristic facial appearance evident at birth:
- brachycephaly (short and wide head);
- flattened nape;
- flattened bridge of the nose;
- raised palpebral fissures;
- epicanthal (Mongolian) folds;
- large protruding tongue.
Babies also have short, wide hands, often with a single palmar crease, and a large gap between the first and second fingers. Severe hypotension can cause problems with eating and decreased activity.
Edwards syndrome (ES)
SE is the second most common trisomy, in which a third copy of chromosome 18 is present. It occurs in approximately 1 in 7,500 live births. More than 95% of pregnancies where the fetus has trisomy 18 abort spontaneously in the first trimester. SE is usually incompatible with life. Less than 10% of affected infants survive to their first birthday. Most children with SE are not suitable for gestational age.
Clinical signs include:
- convex nape;
- micrognathia (small jaw);
- low-set and malformed ears;
- short sternum;
- nail hypoplasia.
Photo: https://en.wikipedia.org/wiki/Edwards_syndrome
Patau syndrome (SP)
With SP, a third copy of chromosome 13 is present in cells. The anomaly occurs in 1 in 12,000 live births. Children usually die in the first year of life. Infants with SP have numerous developmental defects.
Common facial defects:
- cyclopia (fusion of eyeballs);
- cebocephaly (single nostril);
- cleft lip and palate;
- the forehead is usually sloping;
- the ears are often small and misshapen.
Hypospadia (pathology of the structure of the penis) and cryptorchidism (the testicle does not descend into the scrotum) are common in boys, while in girls, as a rule, hypoplasia of the labia minora. Most children with SP also have congenital heart defects.
Klinefelter syndrome (KS)
Occurring in 1 in 500 male births, KS is the most common genetic cause of hypogonadism (testicular failure) and infertility in men. The pathology is caused by the presence of an additional X chromosome.
Approximately 15% of boys with KS have mosaicism. Before puberty, boys with KS are phenotypically indistinguishable from the rest of the population. The diagnosis is often made when the boy is 15 or 16 years old.
Adolescents and young adults with KS tend to be tall and have long limbs. In adolescence or adulthood, gynecomastia (breast enlargement) occurs. Due to the failure of testicular growth and maturation, men with KS have a deficiency of testosterone and an inability to produce “viable” sperm.
Due to low testosterone production, the testes do not develop secondary sexual characteristics (facial hair, deepening of the voice and libido). In adulthood, osteopenia and osteoporosis develop (bones lose mineral density). Most men with KS are infertile because they produce few viable sperm.
By recovering viable sperm through testicular biopsy combined with in vitro fertilization and intracytoplasmic sperm injection, men with KS have a chance of paternity. All children born to these men using this technology had a normal karyotype.
Monosomy
Monosomy is a form of aneuploidy with the presence of only one chromosome of a pair. Partial monosomy occurs when only some cells have one copy and the rest have two copies.
Turner syndrome (TS)
TS is the only condition in which a monosomic fetus survives to term; however, 99% of pregnancies end in spontaneous miscarriage. Occurring in 1 in 3,200 live births of girls, TS is known for its spectrum of relatively mild physical and developmental findings. Affected women typically have normal intelligence and life expectancy.
Girls with TS typically have a characteristic appearance with low-set, slightly misshapen ears, a triangular face, a thickened nasal bridge, and epicanthal folds. Swelling of the arms and legs is characteristic.
Short stature is the main characteristic of this condition, and acquired hypothyroidism is estimated to be five times more common in women with TS than in the general population.
Underdevelopment of the ovaries leads to a deficiency of estrogen (the female hormone), which prevents the development of secondary sexual characteristics in these women and leads to amenorrhea (absence of menstruation). Although 10% of women with TS may experience normal pubertal development and are even fertile, most affected women require estrogen replacement to complete secondary sexual development.
Infertility in these women is not corrected by estrogen replacement therapy. Assisted reproductive technology using donor eggs has allowed women with TS to give birth to children. These women should be closely monitored during pregnancy.
Autosomal monosomies
Complete autosomal monosomies (not associated with sex chromosomes) are extremely rare. It is likely that most of them are so harmful that they are fatal at a very early stage of development and therefore lead to spontaneous abortions.
The only complete autosomal monosomy that has been reported is monosomy 21, although undetected mosaicism or partial monosomy resulting from a subtle translocation cannot be completely excluded. In contrast, reports of partial autosomal deletions are somewhat more common, with some of them recognized as specific clinical syndromes. In general, large deletions have a more significant impact on the limited survival phenotype.
What to do in case of deviations
If preparation for karyotyping analysis was done correctly, the result will be informative. If it turned out to be good, you can relax and start planning the crumbs. Unfortunately, it happens that pathologies are still discovered. In such a situation, parents reasonably ask themselves the question: “What should we do?” It all depends on the specific situation. Genetic defects cannot be treated or completely eliminated, but their manifestations can be corrected. In some cases, even infertility can be overcome. Both women and men are prescribed therapy that can help. (Representatives of the stronger sex are offered to drink drugs that normalize the sexual sphere. Among them, Prostatilen AC performed well).
If attempts to conceive a child are unsuccessful, the spouses are offered to use donor genetic material. In this situation, only one person will become the biological parent. Many couples agree to this. If a pathology was detected in the fetus of a pregnant woman, doctors advise what the consequences are. Further decisions are up to the parents. Only they decide whether or not to give birth to a defective child. No one has the right to persuade people to a certain decision.
If a deviation is detected
If chromosomal abnormalities are detected, do not panic. Even in such a situation, it is possible to carry and give birth to a healthy child, provided that all the recommendations of a specialist are followed.
Even after pregnancy, a woman should undergo a karyotype test to assess potential risks. This will help take timely measures to prevent involuntary termination of pregnancy.
If a deviation in the number or structure of chromosomes is detected in the fetus, then the decision to terminate the pregnancy is made by the spouses. The specialist only identifies potential consequences and provides recommendations.