Thrombocytosis is a hematological pathology characterized by an increase in the number of platelets in the blood.
The provoking factor is associated with dysfunction of bone marrow stem cells.
Such a disorder causes accelerated “production” of platelets, and becomes an obstacle to decay.
In addition, the distribution of “blood platelets” in the bloodstream, as platelets are secondarily called, changes upward. The numerical indicator for healthy hematopoiesis ranges from 200-400*109/l. A value falling below 200 indicates thrombocytopenia; an increase in values above 400 indicates thrombocytosis.
The list of tasks assigned to these blood cells:
- cellular hemostasis
- fight against blood clots - dissolving blockages
- nutrition, protection of blood vessel walls
Platelets in the circulatory system
Human blood consists of plasma and the so-called formed elements: red blood cells, leukocytes and platelets.
Blood consists of a liquid medium - plasma and cells suspended in it - formed elements
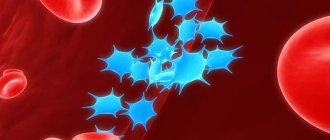
Platelets (blood platelets) are formed in the red bone marrow. These are anucleate cells of round or oval shape, their sizes are 2-5 microns. The average lifespan of blood platelets is 10 days; old and damaged platelets are destroyed in the spleen and bone marrow.
The main function of platelets is to prevent blood loss (for example, during injuries): they are deposited on the damaged surface due to their ability to adhere (glue) and participate in the formation of a blood clot that closes the lumen of the vessel. In addition, platelets take part in the regeneration of the vascular wall, releasing substances that stimulate cell division and growth (so-called growth factors).
Platelets stop bleeding by plugging damaged blood vessels
Functions of blood platelets - video
Norms of platelet content in the blood - table
| Normal platelet count in the blood | |
| For men over 18 years of age | 200–400*109/l |
| In women over 18 years of age | 150–320*109/l |
| In pregnant women | 150–380*109/l |
| In newborn children | 100–400*109/l |
| In infants up to 12 months | 160–390*109/l |
| In infants over 12 months | 180–320*109/l |
| In children from 10 to 15 years old | 180–450*109/l |
| In adolescents from 15 to 18 years of age | 180–420*109/l |
Total information
Diseases of the hematopoietic system are characterized by a comparatively sluggish course, except for some cases. For this reason, there is an insufficient clinical picture. Symptoms do not allow one to clearly differentiate the situation, or are even completely absent until the condition decompensates. Thrombocytosis is relatively rare. It accounts for up to 3-5% of the total number of disruptions to the operation of the corresponding system. At the same time, this is not always a disease. In children and older people, after physical exercise, the platelet concentration increases naturally and decreases just as quickly. The issue of belonging to deviations is controversial and requires a diagnostic assessment by a hematologist.
Platelets are small, colorless plates that do not contain a nucleus. They are formed in the bone marrow and are “fragments” of megakaryocytes - giant multinucleated cells. From the bone marrow, platelets enter the blood, and some of them are retained in the spleen. They exist for about 7-10 days and are then destroyed by liver and spleen cells. Platelets are responsible for blood clotting and stopping bleeding. Their normal amount in the blood is 150-450×109/l.
Symptoms are scant or completely absent. Therefore, it is impossible to speak unambiguously about the condition without a thorough examination. Restorative measures are aimed at correcting the disease or disorder that caused thrombocytosis. Primary forms are very difficult to influence. Symptomatic treatment is required.
What are the dangers of a platelet count disorder?
A change in platelet count can have serious consequences. When the level of blood platelets decreases, thrombocytopenia occurs, the risk of hemorrhages (including cerebral hemorrhages), bruises increases, and even minor bleeding becomes dangerous.
If the number of blood platelets increases, thrombocytosis is diagnosed. The main danger is the risk of blood clots (thrombi) forming in the circulatory system, which can lead to blockage of the vessel and death of the patient.
An increase in the number of platelets is detected in both women and men with the same frequency; the likelihood of getting sick increases significantly in people over 50 years of age, but infants can also encounter pathology. Also at risk are persons suffering from iron deficiency anemia, patients after operations and injuries, and patients with oncology.
Etiology
In medicine, a high level of platelets in the blood—hyperthrombocytosis—is classified as:
- The primary type is an independent disease, essential thrombocythemia;
- The secondary type is a pathology that develops as a complicated form of disease.
The primary type of the disease includes a pathology in the production of excess platelets by the bone marrow - a myeloproliferative disease, a malignant neoplasm (thrombocytopenia).
This disease in a complicated form develops into acute leukemia.
The etiology of thrombocythemia is not fully understood, but there are suggestions that a mutation of certain genes occurs in the patient’s body. Conducted research at the genetic and molecular level has revealed that the mutation occurs at a young age.
Gene mutation has a hereditary etiology, and gene changes can also occur under the influence of external irritant factors. In order to select therapy for essential thrombocytosis, it is necessary to know exactly in which gene the mutation occurred.
Primary thrombocytosis
The secondary type of thrombocytosis is a complicated form of pathologies in the body.
The following pathologies provoke symptomatic thrombocytosis:
- Malignant neoplasms in the lungs;
- Stomach cancer;
- Oncological disease lymphoma;
- Malignant neoplasms in the ovaries;
- Neuroblastoma;
- Infectious pathologies in organs;
- After surgery for pathology with large-scale necrosis in tissues;
- Fractures in bones;
- Surgical removal of an organ - the spleen;
- Frequent bleeding;
- Hemorrhagic vasculitis;
- Rheumatoid arthritis;
- Collagenosis;
- Drug therapy with drugs from the glucocorticosteroid group.
Among the infectious diseases that most often increase platelets are:
- Meningococci;
- Staphylococcus;
- Streptococci;
- Gram-positive and gram-negative bacteria;
- Viruses;
- Fungi.
With prolonged inflammation in the body, a pathology occurs - thrombocytosis, and often in parallel with thrombocytosis, leukocytosis also develops. This phenomenon is not typical for the primary type of pathology, but is a distinctive characteristic of secondary reactive thrombocytosis.
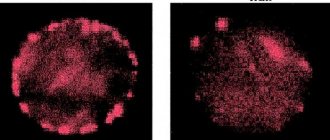
Manifestation of thrombocythemia: RIGHT - release of an excess number of platelets into the blood in any form of thrombocytosis, LEFT - normal.The development of pathology in a child’s body
Primary thrombocytosis is a very rare disease in children. It can develop due to leukemia or leukemia.
The secondary type is a disease that occurs more often in children than in adults.
In addition to anemia, the following pathologies of the child’s body can provoke reactive thrombocytosis:
- Asplenia is a disease in which the cells of the spleen atrophy;
- Osteomyelitis is an inflammatory process in the bone marrow;
- Pneumonia - inflammation in the lungs;
- Viral hepatitis;
- Flu;
- Encephalitis.
Also, the occurrence of thrombocytosis in a child can be a consequence of a fracture of a tubular bone.
In a child, thrombocytosis responds well to treatment if, with timely diagnosis, the exact etiology is established and a diagnosis is made.
Causes and development factors
Thrombocytosis can be clonal, or primary, i.e., occur regardless of the presence of other diseases, or secondary (acquired).
Primary thrombocytosis (essential thrombocythemia)
The clonal form occurs due to tumor damage to bone marrow stem cells. Sensitivity to thrombopoietin increases, and an uncontrolled process of formation of defective platelets begins.
Essential thrombocytosis is a consequence of increased production of megakaryocytes, from which platelets arise. Despite the normal life expectancy, the blood platelets become large and fill the vessels, forming clots. In addition to the formation of blood clots, the risk of bleeding increases, as platelets lose the ability to fully stick together and stop blood loss. Frequent complications are heart attacks, strokes, and gastric bleeding. Most often, the pathology is found in elderly people over 60 years of age and is extremely rarely detected in children and adolescents. Refers to myeloproliferative diseases that occur due to a violation of the hematopoietic functions of the bone marrow. Only 10% of all cases belong to the primary form.
The exact causes of the primary form of the disease are not fully understood. According to one version, a mutation in the V617F gene leads to disruption of platelet synthesis.
Secondary thrombocytosis: the role of oncology in the development of pathology
The secondary (reactive) type of disease is a consequence of a person’s lifestyle and diseases. Among the factors that provoke its occurrence are:
- oncological diseases. They are a common cause of reactive thrombocytosis. Cancer cells stimulate platelet production. Most often they lead to this pathology: oncological diseases of the gastrointestinal tract;
- lungs' cancer;
- neuroblastoma;
- lymphoma;
- polycythemia vera;
- hepatoblastoma;
- bacterial infection with meningococci;
- rheumatoid arthritis;
- corticosteroids;
Classification
The upper limit of normal platelet count varies from 350,000 to 400,000 per microliter depending on the reference intervals of the specific laboratory performing the analysis. According to the degree of increase, the following types of thrombocytosis are distinguished:
- Soft
: from 350-400 to 700 thousand. - Moderate
: from 700 to 900 thousand. - Heavy
: from 900 to 1000 thousand. - Extreme
: over 1,000,000.
The cause of extreme and severe thrombocytosis is oncohematological pathologies. According to the origin of thrombocytosis there are:
- Primary
(tumor, clonal). They account for approximately 10-15% of all cases of thrombocytosis. The cause is tumor diseases of the blood system. - Secondary
(reactive). The most common variety (about 85%). The cause is infectious, systemic inflammatory processes, and anemia. - False
(pseudothrombocytosis). The reason is an error in the hematology analyzer, which mistakes tumor cell fragments during treatment with chemotherapy drugs, small red blood cells, or red blood cells that have undergone hemolysis as platelets. Pseudothrombocytosis is also observed with cryoglobulinemia. - Hereditary
(family). This is a rare genetic disease, the cause of which lies in a mutation of the genes encoding the synthesis of thrombopoietin and its receptors (THPO, MPL).
Symptoms of the disease
The main symptom is an increased level of platelets in the blood. It is often discovered by chance during a routine examination. At the first stages, the patient may not feel any changes in his well-being, but over time the following symptoms appear:
- frequent headaches;
- nasal, uterine and stomach bleeding;
- weakness, decreased energy, drowsiness and irritability;
- blood clot formation;
- numbness of the limbs;
- pain in fingers and toes;
- decreased vision;
- bleeding gums;
- blue discoloration of the skin and mucous membranes;
- vegetative-vascular dystonia;
- the appearance of bruises from minor injuries;
- long wound healing;
- dyspnea;
- enlarged spleen;
- swelling.
Every year, up to 100 thousand Russians die due to blood clots.
Clinical picture of the child
In children, the manifestations of the pathology are similar to those in adults: bruises are often observed after light touches, hands and feet are cold, the child complains of headaches and itchy skin, blood pressure can vary from low to high, and the pulse increases.
Manifestations of thrombocythemia
on the right - the release of an excess number of platelets into the blood in any form of thrombocytosis, (on the left - normal)
Symptoms of thrombocytosis may be absent for a long time, then the disease is discovered either by chance or when complications occur. The most typical:
- Thrombosis and thromboembolism;
- Erythromelalgia (pain in the limbs);
- Neurological disorders associated with cerebral ischemia due to thrombosis and microcirculation pathology;
- Disorders of pregnancy, miscarriages in women;
- Hemorrhagic syndrome.
Manifestations of thrombosis can be myocardial infarction, acute cerebrovascular accident (cerebral infarction). Possible pulmonary embolism. Vascular accidents in young people are often associated precisely with thrombocytosis, which could be asymptomatic for a long time.
Erythromelalgia is another characteristic symptom of the disease, which is expressed in sharp, burning pain in the extremities, usually the feet. The pain intensifies with heat and physical activity; a feeling of heat and darkening of the skin may occur.
Thrombosis of small vessels leads to ischemic changes in soft tissues with severe pain in the fingertips, coldness and dry skin. In severe cases of pathology, thrombosis can cause complete disruption of blood flow, which is fraught with necrosis (gangrene) of the fingers and toes.
hemorrhages in DIC syndrome
Blockage of cerebral vessels by blood clots leads to a variety of neurological disorders: decreased intelligence, dizziness, focal neurological symptoms. When the retinal vessels are damaged, vision suffers.
Thrombocytosis can be very dangerous in pregnant women. In the early stages, it provokes miscarriages, in later stages – placental infarctions, developmental delay and even fetal death, complicated labor (placental abruption, massive bleeding).
Hemorrhagic syndrome occurs in half of patients with primary thrombocytosis and is associated with the development of chronic disseminated intravascular coagulation syndrome, when coagulation factors are consumed in the process of constant thrombus formation. Hemorrhagic manifestations are reduced to hemorrhages in the skin (petechiae, ecchymosis), bleeding of the gums, and gastrointestinal tract. Insufficient blood clotting poses a great danger during surgical operations due to the risk of severe bleeding.
With prolonged thrombocytosis, other symptoms may occur:
- Weakness, fever, weight loss, bone pain as a manifestation of tumor pathology (primary thrombocytosis);
- Pain in the hypochondrium due to enlargement of the liver and spleen;
- Tachycardia, pallor, shortness of breath with the development of anemia;
- Recurrent infectious diseases.
Secondary thrombocytosis does not have such characteristic manifestations as essential thrombocytosis, and the patient presents complaints related to the underlying disease. Thrombohemorrhagic manifestations are not typical, the spleen does not enlarge. Usually it is diagnosed in a timely manner and, with treatment of the underlying disease, quickly regresses without leading to blood clotting disorders.
Diagnostics: laboratory tests and instrumental studies
To make a diagnosis, the doctor will first collect the patient’s medical history and find out information about previous cases of blood clots and blood circulation disorders.
A blood test is most indicative in diagnosing thrombocytosis
Blood tests and leukocyte count are carried out to determine the level of platelets, biochemical analysis to detect markers of the inflammatory process, infectious and rheumatic diseases.
The composition of the blood depends greatly on the age of the patient
Using ultrasound, fibrocolonoscopy and x-rays, the patient is examined for the presence of tumor formations in the lungs, gastrointestinal tract and other organs.
A very important diagnostic method is a red bone marrow biopsy (trepanobiopsy). A 2 mm diameter needle is used with a small spiral that penetrates the bone. Under local anesthesia, a puncture is performed at the border of the lumbar and gluteal region, a tissue sample up to 10 cm long is removed. The structure and functioning of the bone marrow is studied, the structure of cells is examined to identify tumor formations.
Indicators for differential diagnosis of clonal and reactive thrombocytosis - table
| Medical indicators | Clonal thrombocytosis | Secondary thrombocytosis |
| Cause of the disease | Not identified | Often pronounced |
| Lack of oxygen | Is a common symptom | Rarely found |
| Blockage of large veins and arteries | Increased risk | No risk |
| Bleeding | Increased risk | No risk |
| Enlarged spleen | Found in almost half of patients | Rarely found |
| Platelet sizes | Significantly increased relative to normal | Normal size |
| Platelet Function | Violated | Fine |
| Megakaryocyte level | Overpriced | Overpriced |
| The structure of platelets | Enlarged with disturbed morphology and with remnants of old platelets | Fine |
Etiology
Elevated platelets in the blood are such if their concentration differs significantly from the norm in a larger direction. It is noteworthy that the acceptable values will differ slightly depending on the age and gender of the person. For example:
- newborns - 150–420 g/l;
- infants - 150–350 g/l;
- babies up to one year - from 180 to 400 g/l;
- women during pregnancy - 100–420 g/l;
- adult men - 180–320 g/l;
- adult women - 150–380 g/l;
- postmenopausal period - 100–350 g/l.
In most situations, elevated platelet levels in the blood of children develop due to the following factors:
- hereditary pathologies of the hematopoietic system - erythremia, myeloid leukemia and thrombocythemia;
- meningitis;
- inflammatory lung disease;
- parasitic infestation;
- polycythemia vera;
- chronic leukemia;
- fungal and viral infections;
- encephalitis;
- viral diseases of the gastrointestinal tract;
- cancer metastasis to the bone marrow;
- changes in hormonal levels;
- influence of stressful situations;
- surgical interventions;
- insufficient intake of iron into the body.
Unfavorable factors that answer the question of why small blood platelets are elevated in an adult:
- bacterial infections;
- penetration of pathological agents such as parasites, fungi and viruses;
- acute iron deficiency;
- surgical removal of the spleen;
- a wide range of inflammatory processes;
- rheumatoid arthritis;
- collagenosis;
- liver pathologies;
- spondyloarthritis;
- severe arthritis and polyarthritis;
- Kawasaki or Schonlein syndrome;
- malignant neoplasms, among which the most dangerous are neuroblastoma, hepatoblastoma and lymphoma;
- long-term use of certain groups of medications, in particular corticosteroids, sympathomimetics and antibacterial substances;
- various purulent processes;
- tuberculosis and anemia;
- various types of sepsis;
- enterocolitis and hepatitis;
- severe dehydration;
- sarcoidosis;
- infectious lesion of the pancreas;
- amyloidosis of internal organs.
In women while pregnant, thrombocytosis, in addition to the above factors, can occur against the background of:
- insufficient fluid intake;
- profuse vomiting;
- intense physical activity;
- antiphospholipid syndrome.
Platelet functions
Treatment
A hematologist is a specialist in blood diseases. Only he will be able to correctly select treatment methods for the patient based on the type of disease and individual data of the person. Under no circumstances should you self-medicate.
Drug therapy
The clonal form is often treated with antiplatelet drugs that help reduce blood viscosity. Such means include:
- Aspirin;
- Clopidogrel;
- Ticlopedin.
Aspirin is not prescribed if there are peptic ulcers of the stomach and intestines, gastritis. The drug is also contraindicated for children, including infants.
Treatment of primary thrombocytosis is based on the use of hydroxyurea and anticoagulants, which reduce the level of blood clotting and the ability of platelets and red blood cells to stick together. These include:
- Heparin;
- Livarudin;
- Argotoban.
To reduce platelet levels, alpha interferon may be prescribed, but it causes many adverse reactions in 25% of patients (liver dysfunction, anemia, depression, etc.), but is considered quite safe and is prescribed to pregnant women. The effect of treatment lasts only while taking medications.
Why is it undesirable to have a decrease in platelets during pregnancy?
The drug Anagrelide reduces the synthesis of megakaryocytes in the red bone marrow. The effect of taking it is not permanent and gradually disappears after discontinuation of the medication.
The reactive form of the pathology is often cured after treatment of the underlying disease that caused the increase in the number of platelets. At the same time, medications can be prescribed to reduce the level of blood platelets.
Only a doctor can decide how long the therapy will last and what medications will be prescribed. Self-medication is dangerous!
Photo gallery of medicines
Alpha interferon reduces the level of platelets Heparin reduces the level of blood clotting Aspirin is one of the most common drugs for the treatment of thrombocytosis Anagrelide reduces the synthesis of megakaryocytes
Diet
It is very important not only to start eating right, but also to eat B vitamins, magnesium and drink enough water (which cannot be said about coffee - you should avoid the drink).
The following products are recommended for use:
- tomatoes, cabbage, celery;
- sour berries and citrus fruits;
- garlic, onion;
- seaweed;
- peas, beans;
- oatmeal;
- seafood;
- sea fish, cod liver;
- fish fat;
- almonds, pine nuts;
- olive, flaxseed, amaranth and other vegetable oils;
- compotes, fruit drinks, green tea and clean drinking water.
During treatment, you should completely avoid fatty and fried foods, walnuts, bananas, buckwheat, nicotine and alcohol.
Folk remedies
The main purpose of using folk remedies is to thin the blood to prevent the formation of blood clots. It is worth remembering that this is only an auxiliary measure, but not the main one. The use of herbal preparations must be agreed with the attending physician, as there are many contraindications. You should not eat nettle, yarrow and chokeberry (chokeberry). Chokeberry stops bleeding by thickening the blood, which is contraindicated in thrombocytosis.
Ginger tea
Ginger tea can thin the blood.
- Take a tablespoon of crushed ginger root, pour 250 ml of clean drinking water.
- Cook over low heat for 5-10 minutes, adding a spoonful of cane sugar and honey.
- Cool and take in small portions throughout the day.
- Use for 3 days, then take a break for 2-3 days.
If desired, you can add lemon, honey and cinnamon to ginger tea.
Garlic tincture
Take a couple of heads of garlic, chop them and add 250 ml of vodka. Leave in a glass jar in a dark place for 30 days. Take half a teaspoon twice a day until the end of the tincture. Can be diluted with honey or orange juice.
Garlic dilates blood vessels and reduces blood pressure
Mulberry root decoction
This remedy is quite easy to prepare.
- Take mulberry roots and grind them using a blender or grater.
- Pour three liters of water into a saucepan, add 100 g of chopped roots and, after boiling, leave on low heat for 10–15 minutes.
- Let the broth cool and strain it.
Drink a glass before each meal for five days. Take a break for three days and repeat the dose. Store the broth in the refrigerator.
Mulberry has a second name - mulberry tree
Chestnut peel tincture
Pour 50 g of fresh green horse chestnut peel into 0.5 liters of vodka, place in a glass container and leave in a dark place for two weeks. Strain the resulting tincture and before each meal, mix 40 drops with two tablespoons of water and half a spoon of honey. The course of treatment is three weeks.
Chestnut peel increases antithrombin secretion
Orange juice
Drink 100 ml of freshly squeezed orange juice every day for two weeks. You can use a whole orange instead of juice. This method can help cope with increased blood viscosity and can be used even by young children.
If the patient does not have gastritis with high acidity of gastric juice, then oranges will be an excellent remedy for reducing blood viscosity
Thrombocytopheresis
Thrombocytopheresis is aimed at cleansing the blood of excess platelets using special medical equipment. This is an emergency method of therapy when the degree of thrombosis development threatens the patient’s life. Read more about the procedure.
Hirudotherapy
Hirudotherapy - treatment with leeches. It is necessary to find a highly qualified specialist. A special enzyme, hirudin, secreted by worms after a bite, reduces the concentration of blood, significantly thinning it and preventing the formation of blood clots.
For hirudotherapy sessions, only medicinal leeches are used, specially grown for this purpose in biological factories.
Correction
Conservative therapy
In most cases, to correct thrombocytosis, it is enough to eradicate the cause, i.e. treatment of the underlying disease. Short-term thrombocytosis that develops due to stress or drug administration does not require intervention. In case of persistent long-term thrombocytosis, consultation with a hematologist is necessary to identify the cause and prescribe appropriate treatment. Therapy for thrombocytosis has several areas, including:
- Fighting infection. To eliminate the infectious agent, antibacterial (amoxicillin), antifungal (fluconazole), and antiparasitic agents (mebendazole) are used. Treatment of viral hepatitis requires long-term use of peligated interferon in combination with antiviral drugs.
- Treatment of iron deficiency anemia. Correction of iron deficiency is carried out with tablet preparations (iron sulfate). For children, there are forms of syrup and drops for oral administration. The addition of ascorbic acid promotes better absorption.
- Therapy of autoimmune diseases. Treatment of autoimmune diseases is carried out using medications that suppress inflammation - glucocorticosteroids (prednisolone), immunosuppressants (cyclophosphamide).
- Targeted therapy. For myeloproliferative diseases, specific targeted treatment is prescribed to slow down the progressive growth of the malignant tumor. These drugs include Janus kinase inhibitors (ruxolitinib), tyrosine kinase inhibitors (imatinib, dasatinib).
- Symptomatic treatment. To relieve high thrombocytosis, medications are used that suppress the activity of the megakaryocyte lineage, and, consequently, the production of platelets - anagrelide, interferon-alpha, hydroxyurea. For polycythemia, regular bloodletting is successfully used as a treatment method to remove excess formed elements.
- Blood thinning. In case of high thrombocytosis, antiplatelet agents (acetylsalicylic acid) are prescribed to prevent thrombosis. In case of contraindications (peptic ulcer of the stomach, duodenum), platelet receptor blockers (clopidogrel, ticagrelor) are used. In people at high risk of thrombosis (elderly, patients with diabetes mellitus or atrial fibrillation), anticoagulants (warfarin, dabigatran) are used.
Specialized treatment
The only method that allows achieving complete recovery from a malignant hematological disease is allogeneic bone marrow transplantation. This requires HLA typing to select a compatible donor. However, due to the high risk of developing life-threatening complications, this method is used only if conservative treatment is ineffective.
Prognosis: life expectancy, impact on pregnancy and IVF
The prognosis for this disease is favorable. The life expectancy of patients remains virtually unchanged. However, the pathology can cause death due to the increased risk of blood clots. Only in 2% of cases the disease transforms into leukemia. Thrombocytosis increases the likelihood of a missed abortion and also reduces the chances of successful IVF.
Disability can be diagnosed based on certain criteria and the severity of the disease. It is necessary to undergo annual commissions to confirm the assigned group. If the condition is cured or improved, the disability may be removed.
Pathophysiology of essential thrombocytosis
Essential thrombocytosis usually results from pathology of a single pluripotent stem cell clone. However, some women who meet the criteria for the diagnosis of ET have polyclonal lesions. The age distribution of essential thrombocytosis is bimodal: one peak occurs at the age of 50-70 years, the other at a young age (in women).
The lifespan of platelets usually remains normal, but it may be reduced due to their sequestration in the spleen, as well as in patients with erythromelalgia accompanied by digital ischemia.
In older patients with atherosclerosis, high platelet levels can cause serious bleeding or, more commonly, thrombosis. Recent studies indicate that elevated white blood cell counts are an important independent risk factor for thrombosis. Although anecdotal reports (and logic) suggest that high platelet counts may increase the risk of thrombosis, one study showed an inverse relationship between platelet counts and thrombosis risk. Bleeding is a more likely complication of severe thrombocytosis (ie, >1.5 million platelets/μL).
Drug therapy in adults
Treatment of thrombocytosis with drugs helps reduce the number of flat blood cells in the blood and reduce the occurrence of complications. The following drugs are used for this:
- Anti-inflammatory non-steroidal drugs - Aspirin and many other drugs based on acetylsalicylic acid, but with few side effects.
- Warfarin is a new generation drug that helps eliminate blood clots.
- Anticoagulants - "Fragmin", "Fraxiparin" - slow down blood clotting.
- Hydroxyurea is an antitumor agent aimed at reducing the formation of excess platelets in the bone marrow.
- Antiplatelet agents - "Curantil", "Trental" - help thin the blood.
- Interferon is an immunostimulant that has a good therapeutic effect, but has side effects.
Doctors advise not to use hormonal and diuretic drugs during treatment. If there is no effect from drug therapy, thrombocytophoresis is used to remove blood clots from the circulating blood volume.