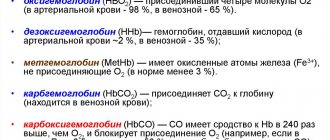
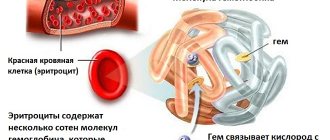
A complex iron-containing protein called hemoglobin is part of red blood cells and transports oxygen from the lungs to the tissues and also delivers carbon dioxide from the tissues back to the lungs.
Its norm is not the same for people of different genders and ages. On average, the following figures can be cited as the norm for an adult: from 120 to 160 g/l.
When hemoglobin decreases, a condition such as anemia occurs, popularly called anemia. Most often, treatment consists of following a special diet, taking iron supplements and vitamins. If hemoglobin is reduced due to any diseases, their treatment is required. Blood transfusions with low hemoglobin can be prescribed in exceptional cases if the cost of the issue is a person’s life. This happens when it drops to a critical level - below 60 g/l. After blood transfusion, as evidenced by reviews from doctors and patients themselves, hemoglobin levels quickly increase and well-being improves.
Indications for blood transfusion
Transfusion with low hemoglobin is not indicated for everyone. Typically, the procedure is performed only in the most severe cases, when the hemoglobin level falls below 60-65 g/l, depending on the clinical situation. What could cause such a strong decrease in hemoglobin content in the blood?
- Excessive blood loss;
- Surgical interventions;
- Oncological diseases;
- Chronic infectious diseases;
- Autoimmune diseases;
- Genetic predisposition.
In some cases, a transfusion may be prescribed when the hemoglobin level drops to 100 g/l , for example, in patients with cardiac or pulmonary pathologies. In each specific situation, before prescribing a transfusion, the doctor takes into account not only hemoglobin levels, but also other parameters of the patient’s condition.
Causes that lead to anemia
“There is no smoke without fire,” says the popular proverb. Every disease always has a root cause. And in the case of leukemia, there are a great many reasons.
Most often, anemia is caused by:
- Chronic infectious diseases.
- Inflammatory processes in the body.
- Unbalanced diet.
- Operations during which a large amount of blood was lost. Including childbirth.
- Due to hidden bleeding of internal organs or chronic bleeding hemorrhoids.
- Previously suffered jaundice.
- Phlebeurysm.
- Eating foods containing only carbohydrates. Protein food is necessary for the body and blood circulation.
- Transitional age.
- Genetic predisposition.
It happens that the body itself shows the presence of a disease in it. In this case, a person needs to refresh himself with clay or eat a piece of chalk. Some people observe themselves and notice that they begin to like the smell of oil paint and gasoline.
How does the procedure work?
For blood transfusion, not whole blood is used, but divided into components. In case of anemia (unless we are talking about anemia resulting from blood loss), only erythrocyte components of donor blood are used. The donor is selected based on blood type and Rh factor; they must match exactly. In addition, a number of compatibility tests are required.
The entire transfusion process takes place in several stages:
- Studying the patient's medical history: risks are assessed, contraindications are excluded.
- A laboratory determination of the patient’s blood type and Rh factor is carried out.
- Suitable donor blood is selected, after which it is assessed for suitability for use: the tightness of the packaging and the appearance of the contents are checked, the data and expiration date are checked.
- Individual compatibility is checked by mixing the patient's blood serum with elements of donor blood.
- Compatibility is assessed by Rh factor.
- Next, a biological compatibility test is carried out. To do this, the patient is injected with 25 ml of donor blood components three times under supervision. After which the patient's condition is assessed. If there is no deterioration in his health, then they proceed directly to a blood transfusion. The dosage is determined by the attending physician based on clinical data.
- Red blood cell mass is administered dropwise at a rate of 40 to 60 drops per minute. In this case, there must be constant monitoring of the patient’s condition. The remainder of the donor blood and serum sample of the patient is stored for 2 days from the moment of transfusion in order to be able to analyze them in case of complications.
- After the procedure, the patient must remain in a supine position for about 2 hours. Monitoring of the condition should be constant throughout the day.
A day after the transfusion, if hemoglobin is low, the success of the procedure is assessed by taking general urine and blood tests.
Types of red blood cells
Red blood cell mass is used to restore cells that carry oxygen molecules. It is the main component of blood, consists of 70-80% red blood cells, 20-30% plasma with an admixture of leukocytes and platelets, hematocrit = 70-80%. In terms of red blood cell content, a single dose of erythrocyte mass (270 ± 20 ml) is equivalent to one dose (510 ml) of blood.
Types of erythrocyte-containing components:
| View | Characteristic |
| EM | Concentrate prepared from whole donor blood. Comprises:
To improve quality, it is allowed to add saline solution before transfusion. |
| Erythrocyte suspension | A concentrate prepared from whole donor blood, in which a significant part of the plasma is removed and replaced with a biochemical solution. |
| Leukoreduced suspension | A concentrate of red blood cells obtained from blood in which the white cells of the donor have been removed. |
| Suspension with removed leukothrombolayer | Concentrated red blood cells made from whole donor blood with the subsequent elimination of maximum plasma and buffy platelet layer. |
| Washed red blood cells | They are made from the mass of red blood cells by washing them with sodium chloride. After which they are a red blood cell suspension from which most of the plasma has been removed. |
| Red blood cells thawed and washed | As a result of thawing and washing, part of the extracellular potassium, sodium and glucose is removed from the mixture, and a minimal amount of plasma proteins remains. |
Red blood cell mass
Each type of red blood cell mass contains a certain amount of hemoglobin, red blood cells, and has its own medical purpose.
Positive effect of transfusion
The main purpose of transfusion with low hemoglobin is to bring the patient's condition back to normal as soon as possible. Blood transfusion also helps restore the volume of blood lost during bleeding.
The red blood cell mass that enters the body replenishes missing blood elements, improves blood circulation, and normalizes blood pressure. It helps the body fight oxygen starvation, restoring the normal supply of tissues and cells with oxygen, resulting in improved functioning.
In addition, the procedure helps improve the body's protective functions and increases resistance to infections. Transfusion improves the metabolism and general condition of the patient.
Against this background, recovery from the underlying disease or pathology, which led to a strong decrease in hemoglobin levels, proceeds much faster and better.
Contraindications
In the presence of severe anemia, there are no absolute contraindications to red blood cell transfusion. Relative contraindications include the following pathological conditions:
- circulatory failure 2-3 degrees;
- chronic renal failure;
- severe liver dysfunction;
- acute septic endocarditis;
- acute glomerulonephritis;
- cerebrovascular disorders, etc.
Possible consequences and complications
Despite following basic safety rules when carrying out blood transfusion due to low hemoglobin, it is not always possible to avoid complications. Possible consequences of blood transfusion with low hemoglobin are divided into several groups, depending on the mechanism:
- Jet:
- Hyperthermia (increased body temperature);
- Massive blood transfusion syndrome (occurs due to the transfusion of large volumes of donor blood and manifests itself in the development of bleeding);
- Hemolytic shock (result of transfusion of incompatible blood);
- Post-transfusion shock (occurs due to the use of low-quality donor blood, when it is overheated, its sterility is impaired, etc.);
- Anaphylactic shock (manifestation of an allergic reaction to components of donor blood);
- Citrate shock (reaction to preservatives in donor blood).
- Mechanical:
- Sudden expansion of the heart due to too rapid supply of donor material through an IV;
- Embolism, which consists of air bubbles entering the blood vessels during transfusion;
- Blood clotting disorders and the formation of blood clots, which can clog blood vessels and disrupt the functioning of organs.
- Infectious – infection with blood-contact infections (syphilis, hepatitis, HIV, etc.) through donor blood elements. This becomes possible if the timing of the control of donor blood, which should be carried out six months after the donation of the material, is violated. This situation can happen in the event of an emergency need for transfusion, when there is no time to recheck the donor material.
The time for the development of complications is always different and depends on their causes. Some of them may appear instantly. For example, embolism, which leads to rapid death. Some - only after a few hours. That is why constant monitoring of the patient after a transfusion is important, because untimely provision of medical care in case of complications can cost life.
Warning signs of low hemoglobin levels
If the patient does not seek medical help for a long time and lives with the symptoms described above, oxygen starvation progresses in his body, the function of carbon dioxide exchange is disrupted and an incorrect acid-base balance is created.
However, this is not the worst thing - there are signs that indicate the seriousness of the process and pose a real threat to life and health. Among them, doctors highlight the following:
- Respiratory dysfunction.
- Constant diarrhea and vomiting.
- The skin loses its pink tint, becomes pale and rough.
- Hair stops growing and becomes dry and brittle.
- Spots and signs of fungal infection appear on the nails.
- There are cracks and ulcers in the corners of the mouth.
- Against the background of absent or excessively low immunity, the patient regularly suffers from colds.
- In the evening he experiences cramps in his leg muscles.
- Taste preferences change (you want something unusual: chalk, lime, clay or earth), your sense of smell also suffers, and a person comes to like the smell of acetone and gasoline.
Do you suspect that you have low hemoglobin? Symptoms, causes, consequences may vary slightly in each clinical case. Therefore, given this fact, it is recommended to immediately consult your doctor if at least one or more symptoms occur. The specialist will prescribe a full examination and necessary tests.
Not everyone can understand why this condition develops, which means it is necessary to consider the reasons in detail.
How to protect yourself from complications
The basis for successful transfusion with low hemoglobin is compliance with all the rules and safety measures provided for by this procedure. What are they?
- Careful study of the medical history : you need to know exactly whether similar procedures were performed in the patient’s history, whether there were operations or childbirth, how they went, what consequences appeared;
- Strict implementation of research techniques when determining blood group and Rh factor;
- Use of high-quality reagents and laboratory equipment;
- Mandatory individual compatibility test and biological test before blood transfusion;
- Careful observation and control of the patient's condition during the transfusion and within 24 hours after it (external assessment of the condition, pressure measurement, temperature control).
As statistics collected by leading institutions of the Blood Service show, negative consequences and complications arising from blood transfusions most often occur due to inattention and violation of the rules of the procedure.
Side effects
If all rules for transfusion of blood or its components are followed, there are no side effects from the procedure. In rare cases, the patient may experience allergic reactions, including anaphylactic shock. If insufficiently warmed blood components are used, ventricular arrhythmia may develop. To prevent problems, the temperature of the material during transfusion should be at least + 35°.
In cases where unwashed red blood cells are used, pyrogenic reactions may develop. In this case, a person’s temperature rises sharply to +39 o or +40°, headaches, fever and chest discomfort appear. These symptoms are not dangerous and go away on their own within a few hours after the procedure. Its appearance is associated with the body’s response to the introduction of a blood product along with pyrogens, which are specific proteins that are waste products of microorganisms.
source
Blood transfusion with low hemoglobin in oncology
In the presence of cancer, anemia becomes a frequent companion of the patient. There are several reasons for a decrease in hemoglobin levels in cancer:
- Radiation therapy leads to severe disruption of hematopoiesis;
- Surgical removal of tumors may be accompanied by large blood losses;
- Cancer in later stages can disrupt the hematopoietic system;
- The disintegration of a tumor under the influence of therapy can also lead to depletion of the body’s blood supply.
In all these cases, transfusion allows for a rapid increase in hemoglobin levels to normal values, which allows the patient to continue treatment. Indeed, during chemotherapy and radiation therapy, in the case of anemia, treatment often has to be postponed, and for cancer patients, delay can be fatal. Therefore, hemoglobin levels in cancer patients are constantly monitored, and if its level decreases, blood transfusion is prescribed according to established standards.