The most important sign of this disease is a change in the color of urine - the patient observes so-called “beer-colored urine.” The disease is also accompanied by pain on the left side of the abdominal cavity, an increase in the size of the spleen, and an increase in body temperature. In the most advanced cases, the urine not only darkens, but becomes dark brown and sometimes black, which indicates the death of too many red blood cells. Many people suffering from this disease experience increased fatigue, drowsiness and rapid heartbeat. This is due to a violation of the exchange of gases in the body and means further serious problems.
In cases where an increase in bilirubin concentration occurs due to the development of liver or gallbladder diseases, the symptoms are somewhat different. This situation is characterized by a very sharp increase in the size of the liver, the appearance of dull pain in the right side of the abdominal cavity, and after (and during) eating the patient feels a bitter taste in the mouth, which is also accompanied by nausea (the temperature may also rise). The feces become almost colorless (sometimes even milky), and the urine quickly darkens. Due to a disorder in the process of bile formation and its outflow (cholestasis), colic appears in the liver, also accompanied by pain under the ribs on the right side, severe itching of the skin, nausea, excessive formation of gases in the digestive system, leading to belching after eating, as well as loss of appetite. Also a characteristic sign of such a disease are problems with the digestive system, expressed, for example, in flatulence.
Bilirubin in urine: how it can get there
Bilirubin is normally found in urine in very low quantities that are not detectable. Therefore, the mark “0” is not a deviation, but it also does not allow us to exclude liver and biliary tract disease. This is explained by the mechanism of its entry into urine:
- First, red blood cells are destroyed, 110-120 days after formation, and hemoglobin is released from them.
- During the breakdown of hemoglobin, biliverdin appears and is reduced to bilirubin (unbound indirect fraction).
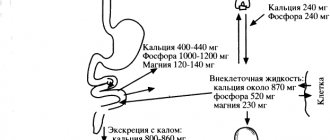
- From the blood, indirect bilirubin passes to the liver with the help of the transport protein albumin.
- In the liver tissue, albumin is detached, and a carbohydrate residue (glucuronic acid) is added to bilirubin, and the pigment becomes able to dissolve in water.
- The bilirubin-sugar complex enters the bile ducts and bile.
- With the flow of bile, the complexes end up in the intestine, where bacteria split off the glucuronide and urobilinogen is formed.
- Urobilinogen is reduced to stercobilinogen, which is excreted in the feces and is partially absorbed through the intestinal wall into the blood.
Thus, in the blood of a healthy person there are:
- indirect bilirubin,
- direct bilirubin,
- urobilinogen.
All of them enter the kidneys, but only urobilinogen and direct bilirubin can pass through the filter when its level increases to 33-35 µmol/l (renal threshold). Indirect bilirubin is combined with the protein albumin, which is retained by intact glomeruli. Urobilinogen, when exposed to air, becomes the yellow pigment urobilin, which gives a yellowish tint to urine.
In what cases do they decide to check bilirubin and protein?
Bilirubin crystals in the urine and protein may indicate increased permeability of the renal tubules, this happens when:
- nephritis (glomerulonephritis, pyelonephritis);
- nephropathy in diabetes, hypertension;
- inflammation of the kidneys in autoimmune diseases (periarteritis, systemic lupus erythematosus, vasculitis);
- severe toxicosis in the second half of pregnancy.
Also, an increased amount of proteins and bilirubin occurs with damage to muscle tissue, increased destruction of red blood cells, and tumor diseases of the bone marrow (multiple myeloma). The symptoms of these diseases are different; kidney pathology may be indicated by:
- swelling on the legs, under the eyes, pastiness (swelling) of the face;
- high blood pressure;
- severe weakness and fatigue;
- unexplained weight gain due to fluid retention;
- fever due to inflammation.
It is excreted in urine or feces
Normally, the bulk of bilirubin is excreted in feces (up to 300 mg per day), and only a very small amount (about 1-1.5 mg) leaves the body through the kidneys. The situation changes if there is a blockage of the bile ducts with a stone, tumor or destruction of the liver, then the urine becomes dark, with abundant foam (similar to beer) due to the increased entry of bilirubin into the bloodstream and its filtration by the kidneys.
Reasons for the increase
If, after the examination, an excess of the permissible norm of direct bilirubin was revealed, this indicates the presence of pathology. More often we have to deal with hereditary jaundice and liver tissue damage, including cirrhosis. This phenomenon can be caused by hepatitis, cholelithiasis and infection with worms.
When indirect bilirubin is increased, this may indicate that a man has a congenital pathology of red blood cells or acquired variants of systemic diseases, such as lupus and lymphogranulomatosis. Hemorrhage of internal organs, blood poisoning, and syphilis contribute to an increase in the level of this compound. This may be the result of taking certain medications. If a representative of the stronger sex takes insulin, or abuses aspirin and chloramphenicol, his bilirubin may increase as a side effect.
Why is bilirubin in urine increased, what does it mean?
In most cases, increased bilirubin in the urine means there is an obstruction to the flow of bile into the intestines or extensive destruction of liver cells. If the bile ducts are blocked, the patient experiences increased pressure in the liver ducts and bile pigment enters the blood instead of the intestines. When liver tissue is damaged by a virus, alcohol or toxic substances, the contents of the cells enter the bloodstream.
The presence of increased bilirubin in the urine helps in diagnosing jaundice, as it allows one to exclude a cause such as hemolysis (destruction of red blood cells). Since indirect pigment predominates in the blood of a patient with hemolytic anemia, it does not pass into the urine due to low solubility in water and binding to protein. The exception to this pattern is severe kidney damage.
Fluctuations are normal for physiological reasons
In order for bilirubin to appear in the urine, it must increase in the blood to at least 33 µmol/l when the norm is up to 21 µmol/l. Without diseases, such changes are rare; in isolated cases, the cause may be:
- long period of fasting;
- intense physical activity;
- use of medications (Paracetamol, anti-tuberculosis);
- numerous injuries with hematomas (accumulation of blood in soft tissues).
A distinctive feature of such conditions is that after eliminating the provoking factor, bilirubin disappears from the urine on its own, and there are no consequences for the liver and biliary system.
Diseases in adults
Bilirubin in the urine is higher than normal in adults with mechanical (subhepatic) jaundice due to:
- cholelithiasis with blockage of the common bile duct by a stone that has passed from the bladder;
- inflammation of the inner layer of the biliary tract with swelling and narrowing of the lumen (cholangitis) or its consequences - cicatricial stenosis (overgrowth of connective tissue that prevents expansion);
- pancreatic cysts or acute inflammation (pancreatitis), cancerous tumors in the head area;
- diverticulum (protrusion) of the duodenum at the exit of the bile duct;
- aneurysm (enlargement) of the hepatic artery.
Increased bilirubin in the urine in men can be one of the signs of alcoholic hepatitis; in patients of both sexes, pigment growth is also caused by:
- hepatitis (inflammation in the liver tissue): viral, drug-induced, parasitic, bacterial, toxic, in autoimmune diseases;
- replacement of normal liver cells with scar tissue (cirrhosis);
- hereditary metabolic diseases, Rotor and Dabin-Johnson syndromes.
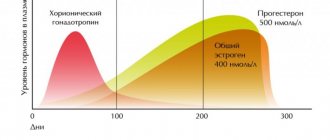
During pregnancy in women
During pregnancy, some women experience thickening of bile under the influence of hormones (high levels of estrogen and progesterone), therefore creating an obstacle to its outflow. Bilirubin first rises in the blood, then it is found in the urine. Yellowing of the skin and severe itching are typical.
It is difficult to exclude hepatitis (infectious or toxic) or liver damage due to toxicosis using a urine test alone, so an extensive examination is always prescribed.
Normal for men
A laboratory blood test for bilirubin provides information about the level of total bile pigment, direct and indirect. The relationship between the last two varieties is very important. This indicator makes it possible to make a correct diagnosis if there are deviations from normal values. The content of bile pigment should be as follows: 20% for bound and 78% for free.
As for the quantitative content, the norm of bilirubin is as follows:
- general: 8.40−19.80;
- straight: 0.10−8.10;
- indirect: up to 20.0.
These indicators are measured in µmol/l. Standards are provided for representatives of the fair sex. However, men have one characteristic feature. They can act as carriers of Gilbert's syndrome. This pathology occurs 10 times more often in them than in women. This is the designation for a hereditary variant of hepatosis. Unconjugated bilirubin increases with this disease, causing the sclera and the surface of the epidermis to become jaundiced. The disease is found in 5% of the world's population, 90% of whom are men.
A number of experts are of the opinion that Gilbert's syndrome is not a pathological condition, but a physiological feature. It was not possible to establish why he targets men more often. Many carriers of the syndrome do not know that they have it. TO
Clinical manifestations sometimes do not make themselves felt until the age of 19. The disease is often discovered by chance: during a standard doctor’s examination or after laboratory tests.
Causes of bilirubin in the urine of a child
The reason for the detection of bilirubin in the urine of a newborn baby is physiological (without disease) jaundice; this reaction is temporary and mild. This occurs due to the increased formation of pigment from destroyed red blood cells and its insufficient connection with blood proteins. If urine bilirubin is high in a year or in children of primary school age, then it is necessary first of all to exclude infectious hepatitis, low thyroid function (hypothyroidism), as well as abnormalities in the development of the biliary system.
In a teenager, abnormalities in tests are one of the first manifestations of hereditary metabolic diseases or congenital disorders of the binding and transport of bilirubin - Rotor, Dabin-Johnson syndromes. There is also a risk of viral hepatitis and biliary tract pathologies.
Other manifestations of bilirubinuria
Slightly increased bilirubin in the urine may not cause signs of deterioration in health. Only the color of urine changes - due to increased secretion of the bilirubin component.
Severe bilirubinuria, when the urine has a rich dark color, is accompanied by characteristic signs:
- yellowing of the sclera and mucous membranes,
- yellowness of the skin,
- dry and itchy skin,
- nausea,
- bitter taste on the tongue
- belching air,
- discomfort under the ribs on the right,
- increased fatigue,
- lightening of stool (up to complete discoloration),
- skin rashes,
- hepatic colic.
The appearance of these signs indicates that bilirubin, due to pathological abnormalities, cannot be excreted through the intestines and enters the urine in large quantities. The resulting condition requires medical examination.
How to properly prepare for a urine test for bilirubin
In order for a urine test for bilirubin to show the correct result, it is necessary:
- 5 days in advance, check with your doctor about the possibility of using the prescribed medications;
- stop taking diuretics and vitamins 3 days before;
- at least 2 days before the study, adhere to the usual drinking regime (there is no need to increase or decrease water and drinks), do not starve or overeat;
- the day before the urine test, alcohol and foods with coloring properties - pumpkin, beets, carrots, citrus fruits - are prohibited.
Women are not recommended to collect urine during menstruation.
Symptoms to watch out for
Bilirubinuria may be accompanied by the following symptoms:
- changes in the color of the skin and mucous membranes in children and adults (they become jaundiced);
- severe itching of the skin or the appearance of various rashes on it;
- general weakness, malaise, sweating, fatigue;
- pain appears in the right hypochondrium of varying severity, a feeling of heaviness or fullness;
- body temperature rises;
- patients are bothered by nausea or vomiting, and stool disturbances (diarrhea syndrome).
How to test urine for total bilirubin and other indicators
Urine for general analysis and bilirubin is taken in the morning; it must be collected during the first urination after sleep. First, the external genitalia is toileted with soap, and the perineal area is dried. Then the first drops fall into the toilet, and about 100 ml are collected in a sterile, dry container. It is immediately covered with a lid and sent to the laboratory within 1-2 hours. The collected urine should not be exposed to sunlight.
Reasons for deviation from the norm
Basically, pathological conditions leading to the growth of pigment in the body are acquired (hepatitis, oncology, cirrhosis, cholecystitis), but there are also disorders transmitted genetically - Gilbert's syndrome and Crigler-Najjar syndrome.
In addition to diseases that lead to dysfunction of the gallbladder and liver, there are factors that do not in any way affect the functioning of these organs, however, they contribute to the growth of bilirubin in the body.
These include:
- anemia of various etiologies;
- diseases associated with accelerated destruction of red blood cells - malaria, blood poisoning;
- taking certain medications (penicillin antibiotics, diazepam, furosemide);
- receiving serious soft tissue injuries, accompanied by hematomas and bone fractures.
As can be seen from the table, the level of bilirubin in newborns can increase on days 3–4 and reach its maximum – 256 µmol/l. In children born prematurely, this value should not exceed 170 µmol/l.
Test for self-determination of bilirubin in urine and its manifestations
Bilirubin in urine can be determined using test strips yourself. Their use is based on the reaction between bile pigment and an oxidizing agent. Depending on the quantity, the color saturation changes. Using the attached table, the bilirubin level in mmol/l is determined for each package.
Manufacturers and trade names of the most accurate test strips:
- "Bayer" Multistix,
- "Biosensor" Urigem,
- "Pliva" Hemofan.
Strips for determining bilirubin in urine are needed for:
- early detection of stone blockage of the common bile duct;
- detection of viral hepatitis at the pre-icteric stage (for example, after contact with a patient);
- excluding hemolysis of red blood cells as a cause of yellowing of the skin;
- control over the treatment of hepatitis and cirrhosis of the liver;
- examinations of people who come into contact with toxic substances during professional activities;
- assessing the condition of the liver when taking medications that damage the liver.
Test strips have sensitivity limits of 8.5-50 µmol/L, and bilirubin of 100 units or higher in urine can only be detected in a laboratory.
Diagnostic institutions use quantitative and semi-quantitative methods. The first show the concentration of bilirubin, and the semi-quantitative analysis reflects 4 options:
- no or traces (designation “0”, or not detected);
- slightly increased (indicated in the form “+”, Small);
- increased (“++”, Medium);
- high (“+++”, Large).
How accurate is the result?
Reagent strips do not always give absolutely accurate results. However, with their help there is a greater chance of identifying a dangerous increase in bilirubin than with a visual assessment of the color of urine. It is visually dark with a significant increase in pigment (from 17 µmol/l and above).
Clinical examples:
- bilirubin in urine 3 µmol/l is a variant of the norm, since an increase to 8.5-8.6 µmol/l is allowed;
- bilirubin in urine 50 µmol/l - most often this increase is caused by complete blockage of the bile duct or the active phase of hepatitis.
How to quickly detect bilirubin in urine
For emergency detection of bilirubin in urine, the following reagents are used:
- Harrison's test - trichloroacetic acid with ferric chloride; if pigment is present, the urine will be blue or greenish;
- Rosin's test - when adding 1% iodine or Lugol's solution, bilirubin will give a green color.
These tests are qualitative, that is, they give an immediate answer - whether there is bilirubin or not. Their technique is very simple:
- 5 ml of urine is poured into a sterile test tube.
- The reagent is pipetted down the wall.
- In the presence of bilirubin, a green ring appears at the border between urine and reagent.
Diagnostic algorithm
To establish bilirubinuria, several diagnostic procedures are performed:
- Fouche's test (based on the detection of bilirubin crystals, which precipitate if barium chloride and a special reagent are added to the urine being tested);
- Rozin's test (a few drops of an alcohol solution of iodine are added to the patient's urine, a green ring appears at the border of the liquids).
In addition to these diagnostic methods, the following studies are used:
- general and biochemical urine analysis;
- general and biochemical blood test;
- coagulogram;
- Ultrasound of the liver and other abdominal organs;
- SCT or MRI of the liver and biliary tract;
- additional studies according to indications (FGDS and others).
What does bilirubin and blood in urine indicate?
Bilirubin and blood in the urine are most often a sign of injury to the mucous membrane of the urinary tract with stones or sand, and the growth of bile pigment in this case may be associated with a false positive reaction to hemoglobin contained in red blood cells. An increased amount of bilirubin in the urine also results from an admixture of menstrual blood.
More rare causes of bloody discharge from the urinary tract include:
- urinary infections (for example, caused by E. coli or staphylococci);
- tumors: kidney, bladder, prostate;
- hemophilia (low blood clotting);
- catheter injury;
- congenital metabolic diseases.
Functions of bilirubin
Medicine understands this term as a breakdown product of heme-containing proteins: cytochrome, myoglobin, hemoglobin. The liver is responsible for the formation of this bile pigment. The whole process goes through several main stages:
- The protein albumin binds bilirubin tightly within the plasma and transports it to the liver. As a result, a protein-bilirubin complex is formed. It does not end up in urine.
- The separation of bile pigment occurs on the surface of liver cells - hepatocytes. Here, binding to glucuronic acid occurs, causing the toxicity of the enzyme to disappear. For this reason, it can be excreted from the body with bile and dissolved in water.
- The further path of the pigment lies to the intestine, where transformation into urobilinogen occurs. This substance is excreted from the body along with feces.
- The remaining pigment that enters the bloodstream is filtered by the liver, after which it is excreted along with the urine.
This bile pigment functions as a cellular antioxidant in relation to hydrogen peroxide, i.e. it binds free radicals and thereby slows down oxidative processes. It can be converted to biliverdin, an intermediate in the process of heme-containing proteins. Bilirubin also determines the functioning of the liver. In addition, it helps restore red blood cells. This bile pigment is divided into three types:
- Indirect. Also called free or unbound. This is a toxic compound that is formed directly during the breakdown of red blood cells. It can easily penetrate the cell membrane. Albumin is responsible for delivering bile pigment to the liver to neutralize the toxic compound.
- Straight. Otherwise called bound, because it combines with glucuronic acid in the liver. This pigment is no longer toxic. It is responsible for the process of bile formation.
- General. This is the sum of the two previous components.
We decipher the indicators of bilirubin in urine and other inclusions
The correct assessment of the level of bilirubin in the urine and other test indicators is given by the doctor, since laboratory diagnostics only confirm the clinical picture of the disease.
Bilirubin and urobilinogen in urine
Urobilinogen in the urine, along with bilirubin, helps to correctly determine the cause of pigment metabolism disorders:
- negative bilirubin in the urine (or traces) and urobilin up to 5-10 mg/l is normal;
- there is bilirubin and urobilin - liver disease;
- there is bilirubin, but there is no urobilin - blockage of the bile ducts;
- no bilirubin and high urobilin – destruction of red blood cells (hemolytic anemia);
- there is bilirubin and traces of urobilin with normal pigment in the blood - damage to the glomeruli of the kidneys (glomerulonephritis).
Bilirubin red blood cells in urine
Normally, red blood cells in the urine are present in the amount of 1-2 per field of view; in a child, a periodic increase to 3-4 cells is allowed. An increase in two indicators simultaneously occurs when:
- infectious diseases;
- tumor process;
- false reaction to hemoglobin (instead of bilirubin).
A blood test can help determine the cause. If the bile pigment in it is normal, then an ultrasound of the abdominal organs is required, and a kidney function test is prescribed.
Bilirubin in urine and jaundice
If there is increased bilirubin content in the urine and there is jaundice, then it is associated with blockage of the bile ducts or liver damage. In order to distinguish these two types (parenchymal from mechanical), data from a patient interview, examination and analysis are taken into account. The following evidence supports obstruction of bile outflow:
- intense attack of pain in the right hypochondrium with increasing intensity;
- nausea and vomiting;
- stool is almost white;
- severe skin itching;
- temperature due to infection, exhaustion due to tumor;
- increased total and direct bilirubin, alkaline phosphatase and cholesterol in the blood;
- there is no urobilin in the urine;
- Ultrasound, tomography show a stone, tumor or inflammation of the pancreas.
With parenchymal (hepatic) jaundice the following is found:
- reddish-yellow skin tone;
- urine is dark, feces are light;
- pain in the right hypochondrium of a pulling or aching nature;
- nausea and loss of appetite;
- the temperature is usually no higher than 37.5 degrees;
- general weakness and body aches are expressed (symptoms resemble the flu, but without a runny nose and cough);
- blood tests show an increase in: total, direct and indirect bilirubin, liver test activity;
- urobilin is increased in the urine;
- Ultrasound shows liver damage and increased blood flow in the portal vein.
Bilirubin and ketone bodies in urine
If ketone bodies in the urine (synonyms: ketones, acetone) are elevated and there is bilirubin, then this is most often a sign of fasting or following a low-carbohydrate diet. An increase in indicators means a lack of carbohydrates (the main source of energy), the breakdown of fats and thickening of bile.
During pregnancy, this combination occurs with late toxicosis.
Ketones and bilirubin increase with alcohol poisoning, and less often the cause is severe infections and tumors.
Hepatitis and bilirubin in urine
With viral hepatitis, the detection of bilirubin in the urine may be the earliest manifestation, since it is found already from the anicteric stage. An increase in concentration is considered a sign of active destruction of liver cells.
Glucose and bilirubin in urine
Detection of glucose and bilirubin in urine occurs when:
- acute inflammation of the head of the pancreas;
- damage to the kidney tubules;
- extensive trauma;
- poisoning with phosphorus, strychnine.
It is also possible that hepatitis may occur in a patient with diabetes. It can be infectious or toxic, medicinal.
Bilirubin and nitrites in urine
If nitrites, leukocytes and bilirubin are increased in the urine, then this is a sign of a severe urinary infection. In such cases, it is usually caused by gram-negative bacteria (for example, Pseudomonas aeruginosa or Escherichia coli), capable of converting nitrogenous compounds. If the content of white cells is normal (0-5 in the field of view), nitrate poisoning can be suspected.
False positive test for bilirubin in urine
A false-positive urine bilirubin test occurs due to the use of antipsychotics (for example, Aminazine), as well as the consumption of food coloring substances. Large doses of vitamin C lead to a false negative result. If you suspect improper preparation for the analysis, it must be repeated.
Ways to bring urine levels back to normal
Determination of bilirubin in urine and a sharp increase in its concentration indicates the need for urgent correction of indicators. Bringing values back to normal is carried out in stages and includes a number of medicinal manipulations.
First of all, this is infusion therapy. It involves intravenous infusion of glucose and detoxification drugs to remove the substance from the body. The technique is used for severe forms of bile enzyme poisoning. Phototherapy with special lamps is used to quickly reduce bilirubin concentrations in infants. From such a glow, indirect bilirubin is destroyed to direct bilirubin and is excreted from the body naturally.
The treatment regimen is developed strictly on an individual basis and is aimed at restoring liver activity. Treatment options vary and depend on the cause of bilirubinuria.
- If hepatitis of an infectious nature is detected, the patient is prescribed antiviral medications selected taking into account the clinical case. Most often these are interferon-type drugs.
- The list of mandatory medications includes medications that stimulate the production and excretion of bile. These are, first of all, choleretics - “Allohol”, “Cholenzim”. They are made using plant ingredients (pine, St. John's wort), so they are absolutely safe for the body. In case of congestion, cholekenetics can be prescribed - “Holosas”, “Mannitol”.
- In order to cleanse the body of toxic substances with their subsequent accelerated elimination, sorbents based on plant components are included in the treatment regimen. These are Smecta, Enterosgel, white and black activated carbon.
- To stimulate metabolic processes, drugs that have appropriate pharmacological effects are used. “Mezim” and “Festal” are considered common.
- In some cases, increased bilirubin is due to the presence of stones in the liver or gall bladder. If they are small in size, it is possible to gradually dissolve and remove them using litholytic drugs and lithotripsy methods. In severe cases, surgery is indicated.
Advice! Since bilirubinuria is a pathology in which the load on the liver reaches critical levels, maintaining a balanced diet is considered important. It assumes a physiologically normal content of proteins and carbohydrates while simultaneously limiting refractory fats, extractives and cholesterol.
The list of permitted products includes:
- lean meat, regardless of variety;
- poultry eggs (chicken, quail);
- fruits with a sweet taste;
- all types of cereals;
- lactic acid products.
All dishes should be consumed boiled or steamed. To stimulate liver activity, juices and herbal teas (chamomile, mint, milk thistle) are considered useful. For prevention purposes, you should adhere to the principles of a healthy and balanced diet and give up bad habits - drinking alcohol and smoking.
Deviation Detection
Causes of impaired bilirubin metabolism
The absence of urobilinogen in urine indicates the cessation of bile flow into the intestines.
Normal urine contains traces of urobilinogen. Urobilinogen arises from direct bilirubin, which is excreted along with bile. If it is absent, then this is a clear sign of a cessation of bile flow into the intestines. The accumulation of the enzyme in the body provokes jaundice syndrome. When the level of bilirubin is elevated, a visible yellow tint to the body and a noticeable darkening of the urine appear. The appearance of jaundice due to impaired bilirubin metabolism is characterized by the following types of disorders:
- When red blood cells are rapidly destroyed, suprahepatic jaundice appears.
- If observed with liver failure - hepatic.
- If there is a complication of bile outflow - subhepatic.
With hepatitis and cirrhosis, enzyme metabolism decreases. Why is this happening? Because liver cells are damaged and new ducts appear through which bile enters the blood. The process causes destruction of hepatocytes, compression of the bile ducts with the appearance of jaundice. Also, when the body is intoxicated or poisoned, disturbances in the metabolic process are observed.
Reasons that cause changes in urine
An increase in urobilinogen occurs when the kidneys fail.
With an increase in pigment in the urine, malfunctions of the liver are observed. All causes are caused by metabolic disorders, inflammation of the liver and pancreas, or intoxication of the body. Urinalysis will show direct bilirubin
Additionally, attention is drawn to traces of increased urobilinogen, which also requires a comprehensive examination of the body to identify the causes
Serious changes in the body occur if:
- jaundice;
- increased body temperature;
- unpleasant belching with bitterness;
- feeling of heaviness and discomfort in the right hypochondrium.
It's suspicious when:
- urine becomes dark in color, and feces, on the contrary, become light;
- the skin begins to itch;
- severe hepatic colic appears.