The importance of timely diagnosis
Recognizing dysentery in practice is not so easy because there are infectious and non-infectious diseases with similar clinical manifestations. A characteristic feature of dysentery pathogens (Shigella) is the ability to change resistance to antibacterial drugs. An untimely diagnosis of the disease will lead to infection of a large number of people. Improper use of antibiotics is the cause of bacterial resistance, leading to mass infections and epidemics with fatal outcomes. The source of infection is patients and carriers of bacteria who secrete pathogenic microorganisms with fecal matter. The incubation period of dysentery is 2-3 days.
Diagnostic procedures
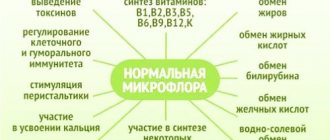
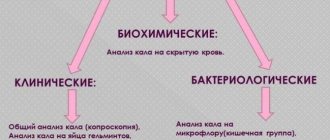
Coprological examination is a simple and accessible clinical method that detects mucus, blood streaks, red blood cells, neutrophils (up to 50 in the field of view) and altered epithelial cells. Diagnosis of the disease includes generally accepted and special methods that establish not only the final diagnosis, but also assess the level of disorders of the digestive system.
Stool analysis for dysentery. With dysentery, the diagnosis is made on the basis of the epidemiological picture of the disease, clinical symptoms and research. The main laboratory diagnostic is stool microbiology analysis, which identifies up to 80% of pathogens. The serological method is carried out no earlier than the 5th day of the disease; this type of study complements, but does not replace, microbiological analysis. Other methods:
- Sigmoidoscopy - allows you to monitor the healing process. Not for use in children.
- The allergy test method is an auxiliary method based on taking a skin allergy test with dysenterine (Tsuverkalov method).
Signs of dysentery
Dysentery symptoms in adults. The latent period of illness can last up to a week. As was already written above, ulcers, erosions and bruises appear on the intestines. Pain appears on the left side of the abdomen, the person’s temperature rises, he experiences headaches, and his appetite disappears. When defecating, pain appears; defecation itself can be up to 10 times a day. Sometimes the urge to go to the toilet turns out to be false. Calla lilies themselves consist of mucus and some blood. If dysentery is severe, then a person’s blood pressure drops and the temperature drops, followed by a rapid heartbeat. Since damage to the digestive system occurs, the patient experiences nausea and sometimes vomiting. In acute dysentery, the symptoms are more pronounced than in chronic dysentery. The disease lasts up to three months with remissions.
Dysentery symptoms in children. Symptoms in children may depend on the type of pathogen, the course of the disease, the severity of manifestations and the immunity of the child himself. The incubation period in children lasts up to 3 days. On the first day the temperature rises, which can reach 40! The child feels bad, overwhelmed and tired, nausea appears, and sometimes vomiting. In more severe cases, the child’s consciousness becomes clouded, a rapid heartbeat and low blood pressure appear. Stools can be very frequent from 10 to 25 times a day and contain mucus and blood. The child experiences a false urge to defecate. In children under one year of age, dysentery can appear with artificial feeding, as well as with rickets, anemia and diathesis. Symptoms appear gradually. Infants may also develop a secondary infection. If dysentery in children was not complicated, then it goes away within two or three weeks. But the restoration of the gastrointestinal tract itself takes about 2-3 months. There may be an exacerbation again if you do not follow the diet.
Stool analysis for dysentery - bacteriological culture (bacteriological culture)
Bacteriological seeding (bacteriological seeding) is a microbiological laboratory study of human biological material by seeding it on certain nutrient media at a certain temperature in order to identify the presence of any number of pathogenic and opportunistic microorganisms in it and further solve the problems of specific treatment.
When certain microorganisms are isolated, a second important analysis is performed - an antibiogram - determining the sensitivity of the detected pathogens to antibacterial drugs and bacteriophages.
Bacteriological culture varies depending on the biological materials used:
- A tank blood culture (or a complete bacteriological blood culture) is indicated for patients with fever and chills. Doctors also prescribe blood cultures to persons with suspected endocarditis, immunosuppression, or intravascular infection. Blood culture for sterility is also used.
- Stool culture tank to detect dysbacteriosis. As a rule, stool culture is prescribed to a patient when conventional tests are unable to identify the causative agent of a particular infection. The doctor and laboratory assistant should tell you how to donate a stool culture tank.
- A tank of culture from the nose and pharynx, indicated for sore throats, sinusitis and rhinitis. Throat culture allows you to identify viruses and bacteria that are not detected by conventional tests. And, for example, bacterial culture from the nose in some cases helps to begin effective treatment without the use of antibiotics.
- A tank of seeding from the eye, indispensable for purulent-inflammatory processes of the eyes. A tank culture of the eye, like similar cultures from other organs, makes it possible to detect an infection that does not manifest itself in other tests.
- Sputum culture tank used in the diagnosis of lower respiratory tract infections and pulmonary tuberculosis. Sputum culture is simply irreplaceable in many cases. Collection of sputum for culture tank should be carried out under the supervision of a laboratory assistant.
- The secretion seeding tank includes the seeding of all biological fluids that are secreted by a person in the process of his life.
- Bile inoculation tank is used for inflammatory diseases of the liver and gallbladder, such as cholecystitis, cholangitis, cholelithiasis. It is used to identify microflora and select the best treatment tactics. The normal result is the absence of flora. If any microorganism is isolated as a result of culture, it is positive. Enterococcus is most often cultured. If Staphylococcus aureus is detected, we can conclude that there is a hepatic or diaphragmatic abscess. Bile is collected during probing or surgery and placed in a 3-4 ml container.
- A culture from the urethra in men can detect sexually transmitted diseases. A tank culture from the urethra is indispensable in the diagnosis of STIs. Just like in men, urethral culture in women is used after routine tests have not identified the causative agent of the present disease.
- Bacteriological culture from the skin of the face will help identify Staphylococcus aureus and other representatives of pathogenic microflora, as well as fungi. A tank culture of the facial skin is carried out with the removal of sebum and epithelium.
- Decoding of the smear culture tank is carried out in the laboratory. The smear culture contains the number of representatives of normal, opportunistic and pathogenic microflora, and therefore it is very informative. The patient can find out what the smear culture shows from his doctor.
Microbiological examination
Dysentery is a disease that can be transmitted through the fecal-oral route. To identify the pathogen, bacteriological and serological research methods are used.
Shigella can be detected in fecal matter using the bacteriological method. Most often, the analysis is carried out several times in order not only to identify the pathogen, but also to distinguish the disease from other intestinal pathologies accompanied by acute diarrhea. That is why preparation for analysis is of great importance to obtain correct results.
Microbiological diagnosis of dysentery includes examination of blood, feces, urine, bone marrow, bile.
Sowing is carried out as quickly as possible after collecting the biomaterial. If this is not possible, the feces are placed in a container with a glycerin mixture, in which they can be stored for 12-24 hours. You can also take the material using a rectal tube, which is inserted into the rectum.
What microorganisms can be detected by bacterial culture?
Stool analysis for dysentery. In the mucus of the nose and throat one can detect hemolytic streptococci (Streptococcuc pyogenes, Streptococcuc agalactiae), pneumococci (Streptococcuc pneumoniae), Staphylococcus aureus (Staphylococcus auereus), Corynebacterium diphtheriae, Haemophilus influenzae type b, meningococcus okk (Neisseria meningitidis ), listeria (Listeria).
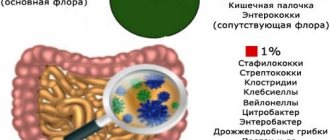
In feces, they try to identify the intestinal group of bacteria - salmonella and shigella (Salmonella spp., Shigella spp.), yersinia (Iersiniae spp.), typhoid-paratyphoid group of bacteria (Salmonella typhi, Salmonella paratyphi A, Salmonella paratyphi B), opportunistic pathogens of intestinal infections, anaerobic microbes, pathogens of foodborne toxic infections, and also examine stool for intestinal dysbiosis.
Pseudomonas or Pseudomonas aeruginosa can be detected in the contents of wounds, biopuncture, and purulent discharge.
The mucus of the urogenital tract is examined for the presence of pathogens of sexually transmitted infections - gonococcus, trichomonas, fungi (Neisseria gonorrhoeae, Trichomonas vaginalis, fungi of the genus Candida), ureaplasma (Ureaplasma urealyticum), mycoplasma (Mycoplasma hominis), listeria (Listeria), You can also examine a smear for bacterial flora.
Blood can be cultured (examined) for sterility.
Materials such as breast milk, urine, prostate secretion, scraping, smear, wound contents, joint fluid, bile are examined for general contamination (bacterial flora).
What is bacteriological culture
Stool analysis for dysentery. The material for research in a bacteriological laboratory is placed (inoculated) on special nutrient media. Depending on the desired search for a particular pathogen or group of pathogens, seeding is carried out on different media.
For example, this could be a selective or elective nutrient medium (for the growth of a single pathogen, while the growth of other microbes is inhibited), an example of which could be coagulated horse serum for identifying diphtheria pathogens or a medium with selenite or with bile salts for detecting intestinal pathogens.
Another example would be differential diagnostic media (Hiss medium), which are used to decipher bacterial cultures. If necessary, transfer from liquid nutrient media to solid media in order to better identify colonies.
Then the nutrient media are placed in a thermostat (a special device), in which favorable conditions (temperature, humidity, etc.) are created for the growth and reproduction of pathogens; the media are kept in the thermostat for a certain time.
Next, a control examination of the grown colonies of microorganisms, which are called a “culture of microorganisms,” is carried out. If necessary, microscopy of colony material is carried out with preliminary staining with special dyes.
What is assessed during a follow-up examination? These are the shape, color, density of colonies, and after additional research - the ability to decompose some inorganic and organic compounds.
Next, pathogens are counted. Microbiological research takes into account such a concept as a colony-forming unit (CFU) - one microbial cell capable of forming a colony, or a visible colony of microbes. Using CFU, it is possible to determine the concentration or number of microorganisms in the test sample. CFU counting is carried out using different methods: counting colonies under a microscope, the serial dilution method, and the sector method.
Coprogram results
The laboratory worker, having received the necessary material for the study, conducts a comprehensive diagnosis, assessing the main parameters of the feces.
| Characteristic | Norm | Deviations from the norm for dysentery |
| Epithelial cell structures | May be observed in small, trace amounts | Determined in high concentrations |
| Leukocytes | Not detected | Predominantly neutrophils are detected, from 35 to 50 cells within visibility |
| Blood | Not detected | May be present in feces starting 2 or 3 days after the onset of the disease |
| Slime | Not detected | In stock |
| Color or shade | Brown, rarely with gradation to halftone | Discoloration of stool is observed, up to partial transparency. In the presence of blood, the test material acquires a pink or reddish tint. |
| Form | Structured, decorated | Unstructured, only partially formalized |
| Consistency filling | Dense, homogeneous | Thick, mushy in the first 2 days after the onset of the disease and liquid in the subsequent acute period of development of dysentery |
The time frame for studying stool analysis during coprogram and obtaining the main results, which will later be interpreted by a medical professional, varies widely and depends on the workload of a particular laboratory, the availability of modern research equipment, the qualifications of personnel, the quality of the material and other factors.
In domestic state or municipal clinics, you can wait up to one week for an answer. Frequent laboratories provide analysis results within 3-4 days, not counting the day the material is submitted for testing. If there is an urgent need, additional payment and increased motivation of staff for a specific sample, an analysis with a conclusion can be ready in 1-2 days.
How long does the analysis take?
Stool analysis for dysentery. In most cases, the answers to the question of how long it takes to seed a tank will be as follows:
- 5-7 days when examining mucus from the nasopharynx;
- 4-7 days when examining urine and feces (in this case, the timing of bacterial culture is specified by a laboratory assistant) ( Main article: “Bacterial culture of urine“
); - 7 days when examining scrapings of the urogenital tract;
- 4-7 days when examining general flora;
- 10 days when testing blood for sterility.
One way or another, you need to find out how many days it takes to prepare a culture tank from a particular organ in the laboratory where you submit it.
How to properly prepare for analysis
Stool analysis for dysentery. The use of certain medications may affect the results of a stool test. Therefore, their use should be suspended or discontinued while preparing for a stool test after consultation with your doctor.
- Stop taking medications (after personal consultation with your doctor). Drugs that may affect stool test results include the following:
- Antidiarrheal drugs (Smecta, Neosmectin, Polifan, Imodium, Enterol)
- Anthelminthic drugs (Nemozol, Dekaris, Vermox, Helmintox)
- Antibiotics - any kind
- Therapeutic and cleansing enemas
- Laxatives (Bisacodyl, Senna extract, Forlax, Portalac)
- NSAIDs – non-steroidal anti-inflammatory drugs (Aspirin, Paracetamol, Ibuprofen)
- Also, be sure to warn your doctor about all medications that you are taking or took shortly before the test.
- If you have been outside the country over the past few months, you should tell your doctor about the places you have been. Parasites, fungal infections, viruses and bacteria that are found in specific countries can affect test results.
- Also, do not use feces that have been in contact with cleaning agents or disinfectants used to clean the toilet, water or urine.
Treatment and prevention
When diagnosing dysentery, it is strictly forbidden to use antidiarrheal drugs that prevent the excretion of the pathogen from the intestines. Symptomatic therapy boils down to taking rehydration agents to eliminate the symptoms of dehydration. Constant intake of sorbents reduces diarrhea and removes toxins from the body. Mild forms of dysentery do not require antibiotics. In severe forms, treatment is carried out with the drug "Ciprofloxacin" and antibiotics from the group of ampicillins and tetracyclines. Insufficient treatment leads to carrier state or transition of the disease to a chronic course.
Prevention of the disease - compliance with hygiene rules, thorough hand washing using antibacterial agents. Purchase only those products that have passed sanitary and hygienic examination. Among the national methods, they include control over drinking water supply, treatment facilities and sanitary improvement of school and preschool institutions.
How to properly collect stool for analysis
- Urinate before collecting material to prevent urine from getting into the stool.
- It is necessary to take a clean, dry container where defecation will be carried out.
- From the resulting material you need to take 8-10 cm3 (~2 teaspoons). Feces are collected using a special “spoon” that is built into the lid of a special container that you should be given to collect feces.
- Feces for analysis are collected from different parts of the stool (top, sides, inside)
- The material (feces) is placed in the container given to you and closed tightly.
- You must sign the container (your first and last name, date of analysis collection)