Gut microbiome
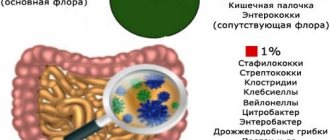
It is known that the human intestine contains about 500 species of different microbes. They are divided into three groups:
- Useful. These include bacteroids, bifidobacteria, lactobacilli and others.
- Opportunistic. With good immunity and the absence of gastrointestinal pathologies, their presence does not manifest itself in any way. However, with deteriorating health and various negative factors, they can cause significant damage to the body. These are clostridia, staphylococci, enterococci, Candida fungi, E. coli and others.
- Pathogenic. These are the causative agents of many infectious diseases that normally should not be present in humans. These include: dysenteric amoeba, salmonella, trichomonas intestinalis, vibrio cholerae, balantidium and others.
What does the analysis reveal?
The analysis allows us to determine the presence of up to 15 types of bacteria in the patient’s biomaterial, which can be normal, opportunistic or pathogenic inhabitants of the intestine. Normally, there are more than 500 species of microorganisms in the human intestine.
The balance of intestinal microorganisms is called microflora. Bacteria that inhabit the intestines belong to one of three groups:
- Opportunistic pathogenic microorganisms . With normal immunity they do not cause harm, but with any risk factors (poisoning, decreased immunity) they begin to multiply and cause infectious processes in the body. Opportunistic microorganisms include the entire family of Enterobacteriaceae (see table below).
- Pathogenic microorganisms . This is a group of bacteria that are dangerous to human health. They can cause acute intestinal infections, including dehydration. These include bacteria such as salmonella, shigella, and vibrio cholerae. Normally, these microorganisms are not contained in the intestinal microflora. Once inside the body, pathogenic bacteria begin to multiply intensively, displacing normal flora and releasing toxins into the bloodstream. This condition requires immediate hospitalization in the infectious diseases department.
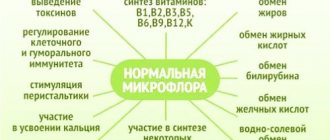
- Normal microorganisms. The main function of normal intestinal flora is to protect the body from colonization by foreign bacteria. Bifidobacteria and lactobacilli secrete acids (lactic and acetic), which destroy the shell of harmful microorganisms. In addition to protection, normal flora supports and stimulates the immune system and removes toxins from the intestines. “Good” bacteria regulate the gas and water-salt composition and produce some vitamins. The normal flora consists of lacto- and bifidobacteria, Escherichia coli, and cocci.
Be sure to read: Symbiotics: concept, list of drugs and products
Table 1. Representatives of 3 groups of intestinal microorganisms.
| Normal | Opportunistic | Pathogenic |
|
|
|
In order to determine the number of certain representatives of the microflora, feces are sown on specialized nutrient media, that is, favorable conditions are created for the life of microorganisms. There are individual nutrient media for each type of bacteria. Bacteria are first grown in liquid media or broths, then they are transferred to solid nutrient media for species differentiation. To accurately determine the genus and type of microorganisms, additional biochemical tests are performed and microscopy is performed.
Read on the topic: Basic “parameters” of feces for self-diagnosis at home
What is included in a stool test for the intestinal group and what microorganisms are detected most often?
Among the most detected bacteria are the following:
- Bacteria of the dysentery group that cause shigellosis (dysentery) is an acute infectious disease that has a fecal-oral route of infection. It affects the large intestine and causes symptoms such as diarrhea, abdominal pain, fever, blood and pus in the stool.
- No less dangerous are bacteria of the typhoid-paratyphoid group. These include the causative agent of typhoid fever - Salmonella typhi and the causative agent of paratyphoid fever - Salmonella paratyphi A, B, C, as well as causative agents of other salmonellosis. The pathogen is transmitted fecal-orally and mainly affects the gastrointestinal tract. Observed symptoms: vomiting, nausea, cramps, bowel dysfunction, fever. With typhoid fever, damage to the central nervous system may occur in the form of lethargy and impaired consciousness.
- Pathogenic E. coli are the cause of escherichiosis, an acute infectious intestinal disease that mainly affects children. Among pathogenic Escherichia coli, those leading to cholera-like diarrhea are distinguished, causing diarrhea mainly in children, leading to dysentery-like diarrhea and the presence of blood in the stool.
The presence of pathogenic microorganisms and their sensitivity to antibacterial therapy can be determined using a microbiology method such as cultivation on nutrient media.
Indications for testing
The main reason for submitting a stool culture to the intestinal group is the suspicion of the presence of pathogenic or opportunistic microorganisms in an active form in the intestine. In addition, the analysis is prescribed during routine checks and when searching for hidden asymptomatic infections during various medical examinations, including for obtaining a health certificate for persons at high risk of being spreaders of intestinal diseases (for example, employees in the catering industry). When identifying pathological processes, stool analysis of the intestinal group plays an important role. If harmful microorganisms are detected, their sensitivity to antibiotics is determined, and the analysis allows doctors to carry out effective treatment. Analysis for intestinal group, what is it? This analysis is the most important part of laboratory testing of feces. Stool analysis helps identify various pathological processes occurring in the body. Analysis of stool for the intestinal group makes it possible to monitor the effectiveness of the treatment. In addition, stool analysis is crucial when examining for the presence of parasites (helminths, giardia and others).
Biochemical analysis of stool
In foreign practice, they realized that waiting 5 days is dangerous, given the percentage of deaths (up to 40%). Scientists are looking for Shiga toxins. Even an atypical strain of Escherichia coli produces poisons. For dysentery, the stool is examined for signs of the toxin.
The strain of E. coli STEC - scientifically O157 - is responsible for most epidemic outbreaks. In 2011, it led to the death of 32 Germans. STEC accounts for up to a third of intestinal infections. Routes of infection and clinical signs resemble dysentery. Atypical strains of E. coli matter.
You need to donate stool at the beginning of the disease. Subsequently, it becomes difficult to detect the toxin. The research method is complemented by bacterial culture and serological analysis for antibodies. Electrophoresis is used for differentiation from Escherichia coli. To identify Shiga toxins 1 and 2, the gene copying PCR method is used.
How to donate stool for the intestinal group?
Before collecting biomaterial for analysis, it is necessary to carry out appropriate preparation. Important points when preparing for the test:
- Nutrition. 3-5 days before the analysis, exclude food containing fish and meat in any form. In addition, before taking a stool test for the intestinal group, you should refrain from drinking alcohol. You should also exclude flour and bakery products, dairy products, as well as potatoes and dishes based on them from your diet. It would also be a good idea to significantly limit the consumption of various sauces, marinades and dishes containing legumes, mushrooms, green vegetables, tomatoes, and fruits.
- Medicines. Three days before the intestinal group test procedure, you should stop taking medications that can have a significant effect on the characteristics of stool. Such drugs include antibacterial drugs, medications that affect peristalsis (laxatives), as well as drugs containing iron and bismuth. In addition, rectal suppositories (suppositories) should be excluded from topical use.
- Habits. When analyzing feces for the intestinal group, there are no restrictions regarding smoking. In addition, the material collection itself may not be carried out on an empty stomach, therefore, you can adhere to the usual daily diet and drinking regime, taking into account the restrictions listed above.
Stool collection for analysis of the intestinal group can be carried out both in a hospital facility and at home. When taking a test in a medical facility, the patient comes to the department, where he lies down on the couch and turns on his side. The laboratory technician performs a standard smear using a regular sterile swab, inserted into the patient's rectum a few centimeters, while at the same time twisting it to better collect biological material. Next, the tampon must be removed and placed in a special test tube with the prepared medium. The biomaterial is then analyzed in accordance with existing protocols. In order to collect feces for analysis of the intestinal group at home, you need to purchase a sterile, hermetically sealed container with a lid from the pharmacy. In the case where feces need to be collected from a small child using disposable diapers, the necessary feces can be collected directly from them immediately after bowel movement (a layer of biomaterial that does not come into contact with the absorbent surface of the diapers).
How to test for dysentery. How to analyze a disgroup
To collect feces, you need to take a clean container and be sure to rinse it. The bottom is lined with a sheet of clean paper, on which you should empty yourself. After defecation, a small portion of feces must be collected in a specially designed disposable container. If the stool has a watery consistency, you can use a pipette to collect it. In this case, the amount of feces should not be less than 2 cm. If there is mucus and pus in the stool, they must be taken for examination, but blood, if any, on the contrary, should be skipped.
Analysis for the disgroup is taken a maximum of 2 hours before the date of delivery. Evening bowel movements are not collected for research. If the diagnosis is carried out in a child, then it is allowed to collect feces from clean linen, avoiding urine residues. At times, you may need to have rectal swabs taken by specialists in hospital. To do this, a tampon is inserted into the rectum and turned several times, after which it is removed. For loose stools, a special catheter is used, which is inserted into the anus with one end and the other into a container for collecting stool.
Feces for bacterial culture
Bacteriological examination of stool (stool tank analysis) allows you to identify possible pathogens of the disease. It is important to know that in order to submit feces for culture, several rules must be followed. Thus, the analysis is not taken when taking antibiotics, NSAIDs, laxatives and anthelmintics. It is necessary to wait 8-12 days before inoculating stool for pathogenic flora. They do not take it even after X-ray examinations of the intestines and laxative enemas. The test cannot be carried out during menstruation, and care should be taken to ensure that urine does not get into the stool.
Stool cultures for examination are taken in the morning and delivered to the laboratory as soon as possible. There, using a certain tool, the resulting material is sown on special nutrient media. These media differ from each other depending on what bacteria need to be grown. After this, the biomaterial is placed in a thermostat to grow colonies of bacteria, which will subsequently be examined to obtain a result about the presence of a certain disease.
Rules for collecting stool for analysis
The feces required for analysis are collected in the morning during the first bowel movement. Before carrying out the procedure, it is necessary to thoroughly wash the toilet, especially its inner surface without using disinfectants, for example, with water and a special brush. After defecation, you should collect the feces with a special measuring spoon from a sterilized container for collecting excrement, which often comes with the container, or can be purchased additionally at any pharmacy. The feces should not contain additional impurities such as urine or blood (during menstruation in women).
The biological material collected by this method should be immediately taken to the laboratory for stool analysis for the intestinal group.
Preparation for bacteriological examination of stool
In order for the results of culture testing for the disgroup to be reliable, you should properly prepare for it. This study identifies pathogenic bacteria that inhabit the human intestines. That is why it is worth excluding factors that affect their livelihoods.
Before taking a test for dysentery, you should exclude medications that could distort the result.
To do this, you need to consult with your doctor. Drugs that distort the test result for dysentery include:
- Antibacterial agents. Even with an acute intestinal infection, you should postpone taking antibiotics until biomaterial is collected for examination. If antibacterial therapy was carried out, then 7–10 days should pass after its completion. And only after that, donate feces to the disgroup;
- Laxatives;
- Enzyme preparations;
- Activated carbon and iron preparations color stool, so they are also excluded;
- Castor and Vaseline oils. It is necessary for their external and internal use;
- Any rectal suppositories.
You cannot perform various enemas before taking the culture for the disgroup. They wash away both beneficial and pathogenic microflora. Nutrition also needs to be adjusted.
3 days before testing stool for dysentery, you should:
- Avoid foods that color feces (for example, beets, pomegranate);
- The menu should consist of cereals, dairy products, fruits and vegetables, eggs and bread;
- Establish a drinking regime. Drink enough clean water.
Alcoholic beverages are prohibited. They promote fermentation, disruption of microflora and coloration of feces (red wine).
How long can biomaterial be stored?
According to the recommendations of specialized specialists, the collected feces should be delivered no later than two hours in order to conduct the most reliable analysis of the intestinal group. If it is not possible to transport the collected biological material within the specified period, a sterile and hermetically sealed container can be placed in the refrigerator in order to increase the specified time interval, but not by more than four hours. If more than six hours have passed since the collection of feces, then the accuracy of the analysis for the intestinal group is significantly reduced, a false positive or false negative result is possible, even if all the rules for collecting and transporting biological material are observed.
General clinical methods
Study of the cellular composition of blood
This routine research method can be quite informative specifically for dysentery, as it reflects the severity of the disease. With a mild course, a general blood test may not reveal any changes or they will be insignificant. On the contrary, in severe forms of the disease, the accents typical of a bacterial infection are expressed very violently.
In severe forms of shigellosis, the following can be detected:
- a significant increase in the absolute number of leukocytes (that is, hyperleukocytosis);
- a significant shift of the formula to the left, that is, an increase in the absolute and relative number of band lymphocytes, up to the appearance of young forms;
- toxic granularity of neutrophils;
- increased erythrocyte sedimentation rate;
- a decrease in the level of color index and hemoglobin concentration, the number of red blood cells (erythrocytes), that is, classic signs of anemia.
Pronounced changes in the general blood test indicate not only the severe course of the disease, but also the possible development of complications, such as intestinal bleeding.
On the other hand, even pronounced changes in the general blood test are nonspecific, that is, they can be observed in many other diseases, and therefore are not the basis for making a final diagnosis.
Urine examination
Only in the case of a very severe course of the disease are changes observed in the general urine analysis, which are a consequence of severe intoxication. Such signs include the appearance of red blood cells, a large number of white blood cells and casts, as well as an increase in protein concentration. In order to exclude possible pathology of the urinary tract, a general urine test should be repeated after the clinical symptoms of dysentery have subsided.
Research methods
The analysis procedure is carried out in several stages:
- microscopic diagnostics, which allows you to examine microorganisms under a microscope;
- bacteriological diagnostics - inoculation of the test material on nutrient media (after six days, the type and activity of microbes is assessed, their number is recorded);
- analysis of the susceptibility of intestinal microorganisms to antibiotics.
The methods listed above refer to in vitro diagnostics, which means “on glass” or “in vitro”.
Bacteriological laboratory specialists can identify pathogenic microorganisms based on their appearance and activity observed using a microscope. This method is called bacterioscopic examination.
Analysis transcript
When analyzing stool for the intestinal group, a “negative result” means the absence of pathogenic intestinal microorganisms and the presence of opportunistic bacteria within normal limits. In this case, an antibiogram is not necessary.
A “positive result” of the analysis indicates:
- the presence of pathogenic bacteria (Salmonella, Shigella, Staphylococcus aureus, pathogenic Escherichia, hemolyzing Escherichia coli);
- active growth of colonies of opportunistic microflora (Klebsiella, Serration, Pseudomonas aeruginosa, Proteus, Citrobacteria).
In this case, the results of the antibiogram are also provided. The acute infectious period is characterized by a sharp disruption of the composition of the intestinal microflora - the displacement of normal microorganisms by pathogenic ones. Deficiency and lack of growth of normal obligate microbes may indirectly indicate the presence of an intestinal infection, in which case experts recommend a repeat analysis.
A positive analysis, that is, the identification of pathogens of dysentery, salmonellosis or escherichiosis in the presence of a clinical picture, means the occurrence of these diseases in an acute form. The absence of clinically significant signs indicates asymptomatic bacterial carriage, including chronic carriage in the case of regular positive test results. If a questionable result is obtained, a repeat examination is recommended. If the test results are negative, the likelihood of disease is low.
Decoding indicators
Only the attending physician interprets the research results. The results are presented on a specialized form according to the form of the medical institution. The quantitative content of microflora microorganisms is taken into account in degrees. The norms for children and adults are different.
| Microorganisms, name | Norms for children under one year old | Norms for adults and children from one year old |
| Bifidobacteria | 1*109 or more | 1*108 or more |
| Lactobacilli | 1*107 | 1*106 |
| Escherichia coli | 1-7*108 | 3-4*108 |
| Pathogenic flora | absent | absent |
| Enterobacter lactose negative | No more than 5% | No more than 5% |
| Cocci from the total number of microflora | No more than 25% | No more than 25% |