Preparing for analysis
In order for the result to reflect reality as much as possible, the analysis must be collected after proper preparation.
- 2 days before the test, you should stop taking medications that affect the child’s stool.
- The day before the test, it is necessary to limit the consumption of meat, fish, vegetables, fruits and herbs.
- 4 days before the analysis, the basis of nutrition should be cereals, eggs, fermented milk products, bread and butter.
For a few days it is strictly prohibited:
- use of rectal suppositories;
- the use of substances that color the mass of feces;
- the presence of allergenic foods on the menu, as well as foods with simple carbohydrates and high fat content;
- smoking and drinking alcoholic beverages.
It is allowed to eat steamed cutlets, vegetable soups, liquid porridges made from rice and oatmeal. A nursing mother should also adjust her diet.
How to take a coprogram
The material should be collected in a clean container after spontaneous bowel movement in the morning. 10-15 g of feces is enough for the study. In rare cases, your doctor may order a 24-hour stool test. In this case, the patient must collect stool for 24 hours.
If the patient suffers from prolonged constipation and cannot empty himself, it is recommended to massage the colon. If this procedure does not bring results, the patient should undergo a cleansing enema. In this case, a solid piece of feces is taken from the washing water.
Analysis collection method:
- In the morning after sleep, the patient is advised to defecate in a pot or vessel
- then, using a special stick or spatula, take a small amount of feces into a clean, dry jar and close the lid tightly.
- It is advisable to immediately deliver the analysis to the laboratory. The deadline is 8-10 hours. After this time, the material may deteriorate and become unsuitable for examination.
- Stool is stored at a temperature of 3-6C.
When examining for worm eggs, the material must be completely fresh, that is, delivered to the laboratory warm.
Stool sampling during bacteriological examination is carried out with the help of a laboratory assistant. The patient is asked to lie on his right side or lean forward while standing. The laboratory assistant spreads the patient's buttocks and inserts a metal loop with a cotton swab wrapped around it into the anus. The insertion should be carried out with rotational movements, very carefully so as not to damage the mucous membrane of the anus
The loop is also carefully removed, then placed in a sterile tube.
Collection of material
Required volume of stool
For research, you should collect 3 - 5 cm 3 (approximately a teaspoon) of feces.
Procedure for collecting stool
You should wash your hands thoroughly and put on latex gloves before collecting stool from a child.
It is necessary to place a polyethylene film under the rim of the toilet, then collect a fecal sample from it. This film can be used in the diaper of a baby who has not yet used the toilet. It is impossible to remove feces from the diaper for analysis, as it absorbs liquid.
It is unacceptable for urine to get into the collected stool, but if contamination has occurred, the sample will have to be taken again. Feces should be collected before they touch the inner surface of the toilet.
You cannot remove feces after a cleansing enema.
How to store and transport coprogram material
Experts recommend donating feces “fresh.” But when it is not possible to provide the material to the place of its research immediately, feces can be stored in a well-closed container at a temperature of +3 oC -+5 oC for up to 8 hours.
It is best to carry the container in a cooler bag or thermal bag. If this is not possible, then the container should be wrapped in several layers of paper and then wrapped in a towel; thick fabric will also work. However, the material must be delivered to the laboratory within 2 - 3 hours.
Why is the material not collected in the evening?
It is not recommended to remove feces for analysis in the evening, since most laboratories are closed and it will not be possible to immediately deliver feces for analysis. You will have to store the material until the morning, as a result of which the results may be false.
Analysis period
The results of the study will be ready 5–6 days after the material is provided. At this time, the laboratory assistant is engaged in microscopic and macroscopic examination of fecal matter, checking them for the presence of foreign impurities, harmful microorganisms and other pathogenic elements.
Coprogram in a baby is normal depending on age and feeding
When examining a child’s stool, a laboratory technician and a doctor (pediatrician or gastroenterologist) take into account the main indicators of the coprogram, which help assess the health of the digestive system and determine pathology.
To determine the presence of a functional malfunction or pathology, you need to know the normal indicators of coprogram in children under one year of age:
| Coprogram indicators | Breastfeeding, newborns and infants up to 8 months | Artificial feeding, newborns and infants up to 8 months | Infants from 9 months to one year |
| Form | Unformed feces | Unformed feces | Decorated feces |
| Consistency | Mushy | Thick mushy | Soft |
| Color | Yellow, sometimes with a greenish tint | Golden yellow or light brown | Brown |
| Acidity (pH) | 4,5-5,5 | 6,5-7,4 | 7-7,5 |
| Neutral fat | Absent, drops may be detected | Absent, may be observed in small quantities | Absent |
| Muscle fibers | – | – | No, only digested ones can be observed in small quantities |
| Soap | Seen in small numbers | A small amount of | May be observed in small amounts |
| Fatty acid | None or found in small quantities | None or small amounts of crystals | No or small amount of crystals |
| Cellulose | Digestible - not detected at all, and indigestible can be detected in small quantities | Digestible - not detected at all, and indigestible can be detected in small quantities | Digestible - not detected at all, and indigestible can be detected in small quantities |
| Starch | – | – | – |
| Iodophilic flora | None or in minimal quantities | None or in minimal quantities | None or in minimal quantities |
| Slime | None or in minimal quantities | None or in minimal quantities | None or in minimal quantities |
| Leukocytes | No or isolated | – | – |
| Red blood cells | – | – | – |
| Hemoglobin | – | – | – |
| Squirrels | _ | _ | _ |
| Bilirubin | + | + | _ |
| Stercobilin | + | + | _ |
Parents should monitor any changes in the health of their child and be sure to pay attention to the presence of pathological impurities in the stool and changes in its characteristics and the appearance of other symptoms of digestive system problems and consult a specialist
It is also important to clarify what resulted in these changes. All this will help to identify functional disorders and pathological conditions in the baby and eliminate them in a timely manner.
All this will help to identify functional disorders and pathological conditions in the baby and eliminate them in a timely manner.
pediatrician Sazonova Olga Ivanovna
Save
Article read: 232
Decoding coprograms in children
In children from one year of age, who already eat mostly solid food, the result and interpretation differs from the data obtained in newborns.
Fecal coprogram in a young child:
- daily norm – 100-250 grams;
- formed feces;
- Brown color;
- fecal odor;
- pH. Acidity should not exceed 7.5;
- mucus, blood, soluble protein - not detected;
- stercobilin. The daily value is 75-150 milligrams;
- no bilirubin;
- ammonia. Calculated for a volume of 1 kg – 20-40 mmol;
- fibers: connective tissue, muscle. Not detected;
- starch, plant fibers, neutral fat, no fatty acids;
- soap Quantity is small;
- leukocytes. Isolated cases.
This is only an approximate transcript of the stool coprogram. Possible deviations from this scheme do not at all mean that the child has health problems. The results obtained can always be explained by a pediatrician.
How to collect stool from an infant for analysis
When ordering a stool test for an infant, parents are faced with a difficult task, which has a time limit; the maximum time allowed for submitting the test to the laboratory is no more than 12 hours.
Of course, the frequency of stool does not cause any particular problems, but the required consistency does cause a number of problems. It is necessary to take into account that a child at this age does not yet go to the potty, so there are a number of rules, knowing which you can collect the necessary analysis.
When do we collect?
You need to collect feces, taking into account the following rules:
- In the morning.
- Without the use of enemas and laxatives. These methods are categorically not recommended by pediatricians.
- You can collect stool the day before, after 17:00, then the analysis will retain its properties. Find out how long you can store stool for analysis here.
- The test will have to be stored in the refrigerator to avoid misdiagnosis.
Where are we collecting?
The analysis is collected in a special sterile jar, which:
- equipped with a spoon;
- costs about 15 rubles;
- sold in any pharmacy.
You should not resort to previously used utensils in the form of mayonnaise jars, even with careful processing, they may contain certain chemical elements that will not allow the doctor to make a correct diagnosis.
Therefore, it is worth observing hygienic storage standards so that feces do not contain any additional impurities.
Of course, before collecting the analysis, it is unlikely that you will be able to wash the child, but it is worth remembering that constant hygiene procedures need to be carried out, this will allow you to correctly draw up a picture of the feces being examined.
How much do we collect?
Many parents wonder how much stool is needed for analysis? To evaluate the result of the analysis, one teaspoon is enough, which in principle will not be difficult when collecting the analysis.
How to decipher the stool analysis of infants
Many mothers, looking at the results of the analysis, understand little about the terms and meanings, but are afraid of the terrible word “leukocytes” (most mothers know that leukocytes mean the presence of some kind of infection). However, decoding the analysis cannot be correct if you do not know the norms for infants, and they differ in many ways from the norms of an adult. The same leukocytes are absent in the stool of adults (possible in minimal quantities in women if collected incorrectly), but for infants, leukocytes in a single quantity are normal.
The decoding of the analysis should also take into account the baby’s nutrition - for artificially fed and breastfed babies, some indicators differ.
Decoding of the analysis, norm for children:
- The amount of feces is from birth to 1 month 10-20 g per day, up to 6 months with breastfeeding - 40-50 g, with artificial feeding - 30-40 g.
- The consistency is mushy when breastfed, and putty-like when bottle-fed.
- Color – breastfeeding – yellow and yellow-green shades, artificial – yellow-brown.
- The smell when breastfeeding is a little sour, when artificially it is putrid.
- Acidity for breastfed children should be acidic (from 4.8 to 5.8), for artificially fed children it should be slightly acidic (6.8-7.5).
- Mucus during natural feeding is allowed in the form of small inclusions, but during artificial feeding it should be absent.
- There should be no blood during any type of feeding.
- Soluble protein, muscle and connective fibers, starch and vegetable fiber are absent.
- Neutral fat is present in minimal quantities as a result of the underdevelopment of the enzyme system.
- Fatty acids are present in minimal quantities in the form of crystals.
- Soaps (salts of fatty acids) are found in small quantities.
- Leukocytes are present in minimal quantities - about 8 within visibility. If leukocytes are found in larger quantities, but the child is cheerful and developing well, there is no reason to panic.
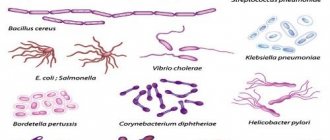
But in the presence of mucus, changes in the consistency, smell and color of the stool, white blood cells in large numbers may indicate the presence of:
- Follicular enteritis. At the same time, lumps of mucus are present in the stool.
- Colitis (dysbacteriosis). In the feces, rods, cocci, and cylindrical epithelium are detected.
- Allergic colitis (eosinophils are present in large numbers).
- Spastic colitis (constipation). Undigested fiber is found in the stool.
- Ulcerative colitis. Neutrophils are detected in the stool.
- Dysentery. In this case, pronounced intoxication of the whole organism is observed, and the content of neutrophils in the leukocyte formula is increased.
In order for the interpretation of the analysis to be correct, it must be taken into account that stercobilin and bilirubin in the feces of infants are normal.
What does stool analysis show in infants and children over one year of age: norms and decoding of the coprogram – Health
Last updated August 29, 2020 at 02:36 pm
Reading time: 7 min
Examination of children at an early age occurs quite often, especially for newborns. Children's still weak immunity needs to be strengthened.
Therefore, in order to prevent diseases, inflammatory processes and disorders that can weaken the body’s protective functions, regular tests are carried out: urine, blood, feces.
Coprogram in children is one of the types of regular research, which involves the collection of fecal secretions and their interpretation by experienced laboratory staff:
- macroscopic analysis. Determines the general condition of bowel movements. May show the presence of parasites, blood, pus, mucus;
- chemical analysis. Studies the pH level of intestinal microflora, coloring pigments such as bilirubin and stercobilin. This also includes a stool test for occult blood;
- microscopic analysis. It is carried out to study the structure and composition of secretions, such as fats, fibers, starch, soaps and other elements of intestinal microflora.
How long does it usually take for the result to be ready?
A standard procedure, such as stool coprogram, takes no more than 2 days. But if there is any doubt, doctors will need more time to study the data obtained, about 6 days.
How to collect stool for analysis
To obtain a reliable and accurate coprogram result, you should prepare for collecting material in advance. Be sure to check with your doctor about the prescription and follow his recommendations.
Submitting stool for analysis requires compliance with several rules before the procedure:
- It is prohibited to carry out cleansing and therapeutic enemas;
- Do not take medications that can change the color of the material;
- Do not introduce medications into the intestines like suppositories.
You will have to limit your baby's food intake for a few days. A newborn baby, of course, will not feel them, since his diet consists only of milk.
Older children will definitely have to adhere to a diet that allows the following foods:
- cooked meat;
- black bread;
- dairy products;
- oatmeal;
- boiled eggs;
- sour cabbage;
- potato.
At the same time, the number of calories received per day should not exceed 2400 - 3000. Switch to a diet that includes eating 5 times a day. On the eve of collecting material and carrying out coprograms in children, it is advisable not to bathe the baby. With normal healthy indicators, the result will be ready on day 2.
Decoding baby feces
What should be the normal result? It all depends on the age of the person being examined. The reason for this is different nutrition and activity, as well as immunity.
What does deciphering the coprogram show in infants and children under one year of age:
- volume. The amount of discharge per day is up to 50 grams;
- consistency. Liquid, viscous;
- color. When breastfeeding - yellow, light yellow, golden, light brown. A bottle-fed baby has a light brown tint;
- smell. In infants with a milk diet it is sour, with a mixed diet it is putrefactive;
- pH level. Acidity values from 4.8 to 7.5;
- mucus, blood, soluble protein - not detected;
- stercobilin, bilirubin – present;
- no ammonia detected;
- detritus. The norm varies;
- fibers: muscle, connective tissue. Small volume;
- there is no starch;
- fiber of plant origin. Dissolves in the body through digestion. Must not be present;
- fatty acid. A little;
- soap Rare cases in infants;
- leukocytes. The indicators are single.
If parents have doubts, they can always consult a pediatrician and check whether all indicators are normal.
Decoding coprograms in children
In children from one year of age, who already eat mostly solid food, the result and interpretation differs from the data obtained in newborns.
https://www.youtube.com/watch?v=jAzNFvk3YKY
Fecal coprogram in a young child:
- daily norm – 100-250 grams;
- formed feces;
- Brown color;
- fecal odor;
- pH. Acidity should not exceed 7.5;
- mucus, blood, soluble protein - not detected;
- stercobilin. The daily value is 75-150 milligrams;
- no bilirubin;
- ammonia. Calculated for a volume of 1 kg – 20-40 mmol;
- fibers: connective tissue, muscle. Not detected;
- starch, plant fibers, neutral fat, no fatty acids;
- soap Quantity is small;
- leukocytes. Isolated cases.
This is only an approximate transcript of the stool coprogram. Possible deviations from this scheme do not at all mean that the child has health problems. The results obtained can always be explained by a pediatrician.
Amount and consistency of stool
A newborn baby can excrete about 20 grams of feces per day, a child from 6 months to one year - from 100 grams to 250 grams. The increase in bowel movements depends on the intensity of growth, as well as changes in nutrition, the transition to normal adult food.
There are other reasons for the amount of feces to increase:
- pancreatitis;
- improper functioning of the digestive system;
- stomach upset. Diarrhea;
- problems with bile secretion.
What does normal stool look like?
In infants it is liquid and viscous, since at this age only milk is consumed. A shaped, denser one indicates that the child has switched to solid food.
Stool color and smell
The familiar brown tint of discharge is considered normal in adults. But in infants and small children, bowel movements do not correspond to these data.
What does the color of a child’s stool indicate? How to understand what to do if it has changed:
- black. This may be a sign of gastrointestinal bleeding;
- brown. Indicates colitis, constipation, consumption of protein, plant foods;
- red. For focal lesions of the stomach;
- greenish. Baby food containing vegetable ingredients;
- light yellow. During the period of milk feeding;
- white chair. Problems with the liver, duodenum, jaundice.
Often in childhood, there may be a dramatic difference in the color of the stool from a yellow and golden hue. In this case, you should take a close look at the baby’s nutrition, especially for a baby on artificial feeding with additives.
If everything is fine with your diet and the color of the discharge does not change, you should go to the pediatrician for examination.
Stool pH
This value determines the level of acid-base balance of intestinal microflora. Any deviation from the norm of coprogram in children is considered a sign of an inflammatory process. It also indicates parasitic diseases, viruses or bacteria.
How to decipher the pH indicator:
- up to 5.5. Acid environment, intolerance to dairy products. The body's reaction to the ingestion of lactose;
- 5.6 - 6.8. The need for examination of the small intestine;
- 7.8 - 8. Weak bowel function;
- 8.1 - 8.5. Colitis, constipation, pancreatic dysfunction;
- more than 8.5. Digestive system disorders or dyspepsia. Alkali predominates.
A baby who eats too many carbohydrates may experience fermentation in the stomach. The pH result can show up to a value of 6.8. In this case, there are bacteria in the body. They lead to the growth of an acidic environment.
Stool with mucus
In healthy children, bowel movements should be uniform, without impurities. In infancy, a slight presence of viscosity is allowed.
But if the baby is more than one month old, then mucus in the stool can show:
- infection;
- haemorrhoids;
- body reaction to dairy products;
- haemorrhoids;
- bowel dysfunction or irritation;
- polyps.
There are still a large number of diseases that lead to the formation of mucus in the bowel movement. To determine them, additional tests are prescribed, and diagnostics are carried out based on specific cases.
Blood in stool
The appearance of even a small amount of blood cells in the baby’s secretions should alert parents. This sign is very dangerous for a child.
https://www..com/watch?v=ogZb7cCxwO0
Blood in the stool can only indicate diseases:
- on toilet paper. A clear sign of hemorrhoids or fissures in the anal area;
- veins in defecation. Symptoms of ulcerative colitis, rectal cancer, Crohn's disease;
- blood with mucus. Indicates proctitis, polyps, ulcers;
- loose stools with blood. Infection in the intestines.
In this case, a coprogram is a necessary procedure. Additionally, other tests will be prescribed to diagnose possible concomitant diseases.
What are stercobilin and bilirubin: norm and deviations
Bacterial formation of intestinal microflora occurs in children under 3 months. At this age, their feces are not colored, since only bilirubin is present.
Stercobilin is an enzyme that gives stool its natural brown color. It is formed from bile and becomes the result of the processing of bilirubin. Only after 9 months is the baby’s intestinal microflora fully formed, which means that the result of stool coprogram shows only stercobilin.
If bilirubin is detected in a child at 10 months:
- dysbacteriosis;
- accelerated bowel function;
- metabolic disorder;
- hepatitis;
- stones in the biliary tract;
- inflammation of the lymph nodes;
- improper functioning of the spleen.
All these complications will be indicated during the examination. Follow-up treatment will be required.
Fiber in stool
The result of coprogram in a child who receives only breast milk or formula will not show muscle and connective fibers. They are observed in rare cases after a year of life in children who consume animal products and receive sufficient amounts of protein.
If fibers are visualized:
- gastritis;
- pancreatitis;
- improper functioning of the pancreas;
- diarrhea;
- dyspepsia;
- ahilia.
The bowel movements may contain undigested cartilage residues. This is not a deviation from the norm and is not considered a violation.
Protein in stool
The presence of unacceptable soluble protein resulting from coprogram should not be displayed.
What does the protein in the coprogram indicate:
- inflammatory process of the digestive organs;
- colitis. Ulcerative;
- dyspepsia. Putrid;
- celiac disease.
A more detailed explanation is given by the pediatrician. He will determine the reasons for the appearance of protein in the stool.
Starch
It enters the baby’s body along with food. These include grains, vegetables, and fruits. Starch breaks down very quickly and therefore should not be visualized.
In what cases is starch found in the coprogram:
- gastritis;
- accelerated intestinal excretory function;
- pancreatitis;
- dyspepsia. Fermentation form;
- diarrhea.
Don’t forget about the digestive system and the reasons why starch cannot be fully broken down.
Undigested plant fiber
It is this type of fiber that can often be found. Digestible is completely absent.
Reasons why undigested plant fiber is observed:
- pancreatitis;
- high content of plant foods in the diet;
- ulcerative colitis;
- indigestion;
- dyspepsia. Putrid.
Requires additional diagnostics.
Neutral fats and fatty acids: indicators
These are products of food digestion that should be absent from the coprogram results.
Even a small amount of them indicates problems with the gastrointestinal tract:
- pancreatic dysfunction;
- insufficient bile production;
- dyspepsia. Fermentation.
In this case, additional research is needed.
Soap in the stool of infants and small children
They appear more often in infants, as they are undigested residues of fatty acids consumed in large quantities, which are contained in dairy products.
https://www..com/watch?v=jAzNF3YKY
If they are observed in adult children:
- pancreatic dysfunction;
- insufficient intestinal absorption;
- dyspepsia. Form - fermentable;
- cholelithiasis;
- problems with bile formation.
The need to examine the liver and find out the reasons for its dysfunction.
Leukocytes
If more than 10 units of leukocytes are detected in the analysis, additional diagnostics must be performed.
This may indicate that an inflammatory process is occurring in the gastrointestinal tract:
- dysentery;
- allergic colitis;
- changes in the structure of the small intestine;
- dysbacteriosis;
- parasites.
Diagnosis of accompanying signs and possible diseases is carried out only as prescribed by a pediatrician. Summer is the most favorable period for the appearance of infestations, so you will additionally need to be tested for worms.
Source: https://healwlrds.ru/chto-pokazyvaet-analiz-kala-u-grudnichkov-i-detej-ot-goda-normy-i-rasshifrovka-koprogrammy.html
Brief description of the research results obtained
Fecal reaction. With a mixed diet in children and adults, a neutral or slightly alkaline reaction is considered normal (that is, pH approximately 6-7.7). If there are poorly digested food remains in the intestines or stomach, then the analysis will indicate a pronounced alkaline environment. An acidic environment is a consequence of a disruption in the absorption of fatty acids in the small intestine.
Protein. For a healthy person, the absence of protein in a stool sample is the norm, provided that the sample was taken according to all the rules. Its presence indicates that inflammatory processes occur in the area of the small or large intestine, which cause minor bleeding.
Blood. If the coprogram revealed the presence of red blood cells in the stool and showed a negative test result for occult blood, this indicates the presence of internal bleeding. This result is most often observed in people with various types of peptic ulcers. The presence of white cells indicates an inflammatory process in the gastrointestinal tract.
Bilirubin. In a child who is no more than 9 months old, the presence of bilirubin in a stool test is considered an acceptable norm, since the normal bacterial flora has not yet fully formed. In older children and adults, stool analysis should not detect it, since during normal functioning of internal organs, bilirubin is processed by intestinal microflora into stercobilin. The cause of the appearance of bilirubin is increased intestinal motility.
In the stool of a healthy person there are altered muscle fibers. The detection of unchanged elements indicates improper functioning of the stomach and pancreas.
Plant fiber. The interpretation of this analysis should not indicate the content of plant fiber in the feces. During normal functioning of the digestive system, plant fiber is completely broken down by microflora. Unprocessed fiber is an indicator that the human body does not have time to process it due to its excessive consumption.
Fat in the stool of a healthy person can only be detected in the form of crystals, soaps and fatty acids, which are contained in minimal quantities. If this indicator is significantly overestimated, then the proper functioning of the liver, biliary tract and pancreas is disrupted in the body.
Starch. It shouldn't exist. Starch is formed as a result of fermentative dyspepsia or disturbances in the functioning of the pancreas.
Iodophilic flora are microorganisms (yeast cells, rods and cocci). A minimum standard of their content or complete absence is acceptable. Excessive amounts of iodophilic organisms indicate an imbalance in the intestinal microflora.
Yeast mushrooms. If analysis of the stool coprogram revealed their presence in large quantities, this indicates a disturbance in the intestinal microflora. To restore the microflora, antimycotic therapy is recommended.
More detailed information on deciphering coprogram data should be obtained from your attending physician, especially if there are any deviations from the norm. After reading the test results, if necessary, the doctor can prescribe a number of additional tests, make a diagnosis, prescribe treatment, or congratulate you on the good results of the stool test.
Stool pH
This value determines the level of acid-base balance of intestinal microflora. Any deviation from the norm of coprogram in children is considered a sign of an inflammatory process. It also indicates parasitic diseases, viruses or bacteria.
How to decipher the pH indicator:
- up to 5.5. Acid environment, intolerance to dairy products. The body's reaction to the ingestion of lactose;
- 5.6 - 6.8. The need for examination of the small intestine;
- 7.8 - 8. Weak bowel function;
- 8.1 - 8.5. Colitis, constipation, pancreatic dysfunction;
- more than 8.5. Digestive system disorders or dyspepsia. Alkali predominates.
A baby who eats too many carbohydrates may experience fermentation in the stomach. The pH result can show up to a value of 6.8. In this case, there are bacteria in the body. They lead to the growth of an acidic environment.
Indications for prescribing coprograms in infants under one year of age
At a certain point in the life of the baby and his parents, there comes a time when the child is prescribed the first tests (blood, urine and stool).
A coprogram is prescribed in the following cases:
- as a routine examination of the baby’s digestive tract in addition to an ultrasound examination of the abdominal organs, which is carried out at the end of the first month of life;
- when a child is admitted to a hospital, this examination is included in the list of mandatory tests, as are blood and urine tests;
- before starting professional vaccinations to eliminate contraindications;
- if you suspect the presence of functional disorders or pathological conditions of the digestive system and other organs (constipation, intestinal colic, regurgitation, diarrhea).
In order for the results to be correct, you cannot take this test if the baby received the following the day before:
- sorbents;
- laxatives;
- iron supplements;
- food products with various dyes or preservatives.
- for constipation;
- with vomiting;
- with periodic abdominal pain;
- for nausea, heartburn, belching;
- when clarifying chronic pathology of the stomach and/or duodenum;
- with dysbacteriosis;
- for other symptoms of gastrointestinal pathology.
Standards for general stool analysis
In terms of chemical composition, stool consists of 80% water, the remaining percentage is dry residue - living microorganisms and undigested food particles (in a 1:1 ratio)
It is important to understand that the composition and structure can vary significantly even within one week. First of all, it depends on the diet and the amount of water consumed.
In the presence of pathologies of the gastrointestinal tract, an even greater variation in the chemical composition of the biomaterial under study is noted. The health of all other systems and organs of the patient being examined also has an indirect effect.
Particular attention should be paid to the normal content of ammonia, muscle and connective fibers, fatty acids, soaps, plant fiber, and leukocytes in feces. The norm of all defined criteria for coprogram in children is presented in the table with interpretation
The norms of all defined criteria for coprogram in children are presented in the table with a transcript.
| Analyzed indicator | Variant of the norm |
| Structure | Soft and dense are allowed |
| Form | Cylindrical |
| Smell | Natural feces, in infants – slightly sour |
| Color | Brown is allowed (from light to dark), yellow - for babies |
| pH | 7,0 – 9,0 |
| Blood and its elements (erythrocytes and leukocytes) | Not detected or single elements noted |
| Slime | |
| Remains of undigested food particles | |
| Muscle fibers unchanged/changed | |
| Plant fiber | |
| Fat neutral | |
| Fatty acid | |
| Soap | |
| Starch intra- and extracellular | |
| Crystals | |
| Iodophilic bacteria | |
| Clostridia | |
| Intestinal epithelium | |
| Microscopic fungi (yeast) |
Meaning of indicators
If the resulting transcript does not correspond to the norm, this indicates disturbances in the functioning of the child’s gastrointestinal tract or an ongoing illness.
If the volume of feces does not match, this warns that the baby is prone to diarrhea or constipation. Its density shows the volume of fluid in the stool: with high fluid levels, increased secretion occurs, with medium levels - loose stools and colic, with low levels - constipation and intestinal spasms. The diet of the baby or mother affects the color of children's stool. The norm does not allow the presence of black or dark brown color, which indicates putrefactive processes in the body. An exception is taking iron-containing medications. Green indicates increased peristalsis, and red indicates ulcerative colitis. If whitish shades occur, you should sound the alarm, as they are a consequence of hepatitis and pancreatitis. The norm can be represented by green discharge if it appears in the first 4 months of the baby’s life. Acidity analysis helps determine the quality of the microflora: with a high level, fermentation takes place in the body, and with a low level, a putrefactive process takes place. Only a coprogram can detect red blood cells and blood in the stool. The norm does not imply their presence in the mass, which indicates polyps or bleeding. Sometimes in healthy children the analysis reveals red blood cells, but their norm will be in the range of 2 to 3 units. However, even with such indicators, it is necessary to see a doctor. There should be no protein in the biomass. Protein present in the results indicates inflammation and digestive difficulties. If mucus is present in children who are only breastfed and up to 5 months, this is normal
Also here you should pay attention to the content of leukocytes: normally they are absent or there should be a minimum number of them. If, before the introduction of complementary foods, the analysis shows the presence of starch or fiber, this indicates poor absorption of food by the baby. Fatty acids appear during a disease accompanied by putrefactive dispersion, and neutral fats appear when the functioning of the gallbladder or pancreas fails. If the analysis reveals fatty acids or neutral fats in the test material, you should consult a doctor as soon as possible. Increased intestinal motility is manifested by the presence of bilirubin in the stool
Determining bilirubin only for children under 8 months is the norm. The absence of soaps in children indicates dispersion. The norm dictates that an increased number of leukocytes can signal colitis, dysentery or hemorrhoids. Stercobilin first appears in the analysis when positive beneficial microflora is established in the baby’s intestines - by about 5-6 months of life. Therefore, in infants up to 5 months of age, stercobilin is absent in the feces. In children under 8 months of age who are breastfed or bottle-fed, stercobilin should already be detected. At 8-9 months, the analysis will normally show only stercobilin, and bilirubin will be absent. Thus, stercobilin gradually replaces bilirubin in the child’s body.
Stercobilin, present normally, is characteristic of healthy children. If stercobilin is shown in reduced quantities, this may indicate diseases such as:
- obstructive jaundice;
- inflammation of the bile ducts;
- hepatitis.
If stercobilin is not detected, this indicates underdeveloped bile ducts or their complete blockage
In this case, you should pay attention to the age of the baby
If stercobilin is present in increased quantities, this indicates:
- hemolytic anemia;
- excessive secretion of bile;
- increased spleen function.
Due to the collection of material for a coprogram, the doctor may recommend special preparation in order to carry out the analysis correctly and obtain accurate results. The analysis needs to be deciphered only by a pediatrician, who, if necessary, can prescribe effective treatment for the baby.
Undigested plant fiber
It is this type of fiber that can often be found.
Digestible is completely absent. Reasons why undigested plant fiber is observed:
- pancreatitis;
- high content of plant foods in the diet;
- ulcerative colitis;
- indigestion;
- dyspepsia. Putrid.
Requires additional diagnostics.
Neutral fats and fatty acids: indicators
These are products of food digestion that should be absent from the coprogram results.
Even a small amount of them indicates problems with the gastrointestinal tract:
- pancreatic dysfunction;
- insufficient bile production;
- dyspepsia. Fermentation.
In this case, additional research is needed.
When is a stool test prescribed for a newborn?
If the baby is completely healthy, then he does not need to submit stool for examination. But there are a number of symptoms for which the doctor may prescribe this test:
- Too frequent watery stools.
- Incessant colic, constant bloating.
- The presence of impurities in the stool (fresh blood, a lot of mucus and foam).
- A sharp change in the color of stool and its smell.
- Allergic reactions, manifested by symptoms of digestive disorders.
- Suspicion of infectious diseases or parasitic lesions.
Prescribing a course of treatment with antibacterial drugs is also the reason for examining stool. This is extremely necessary to identify dysbiosis.
How to prepare a child for analysis
To obtain a reliable coprogram result, you need to properly prepare the child for stool collection. It is better to check with your doctor about all the key aspects of such preparation.
But there are also generally accepted measures:
- You cannot give the child enemas or carry out any cleansing procedures before the analysis;
- do not administer rectal suppositories several days in advance;
- the material provided for research must be fresh;
- exclude in advance the use of medications that may affect the properties of feces;
- Before collecting feces, you cannot wash the child or wipe the anal area with napkins; it must be untouched.
Another important stage in preparing for stool collection is diet. Parents will need to limit the baby's diet for several days.
The following will need to be temporarily excluded from the child’s diet:
- potatoes;
- black bread;
- boiled meat;
- oatmeal;
- boiled eggs;
- sauerkraut;
- dairy products.
A child should consume no more than 3000 kilocalories per day. The entire amount of food taken should be divided into 5 meals. As for newborns who are breast-fed or bottle-fed, they do not need any diets.
How to take a stool test for coprogram
To decipher the results of a stool analysis, you need to follow some rules:
- Before taking a coprogram, you should not take any medications. This also applies to infants who take medications to relieve bloating and colic.
- If a stool sample is taken to detect occult blood, then for several days before the test you should not eat meat, tomatoes, fish and all foods that help increase hemoglobin. It is worth holding off on additional studies of the stomach and the entire intestinal tract (fibrogastroscopy, irrugoscopy). On the day of the test, you should not brush your teeth to avoid the risk of injury to the gums and blood entering the gastrointestinal tract.
- A week before collecting a stool test for a coprogram, you need to change your usual diet. Daily food items for the entire preparatory period should be: potatoes, white bread, dairy products, oils and eggs.
- Feces are collected in a dry and clean container. A clean baby food jar can be used as it, but it is best to purchase a container specially designed for collecting tests at the pharmacy (it is sterile).
- The stool test should be done in the morning and no older than 6 hours.
- Apart from feces, other excretions (urine, leucorrhoea, etc.) should not get into the container for collecting tests.
- Fecal analysis of an infant involves collecting excrement from the diaper, since the diaper absorbs some of the liquid from the sample. For this reason, there is a possibility that the transcript may be incorrect.
Coprogram of feces, decoding for an infant - Infant
07.11.2019
Especially if we are talking about a small child who cannot talk about what hurts him. By prescribing tests, the doctor can understand the causes of certain diseases, help the patient improve his well-being and relieve him of ailments.
One of such informative analyzes in children is coprogram. What kind of analysis this is, why it is prescribed and how to take it correctly, we will tell you in this article.
Indications for use
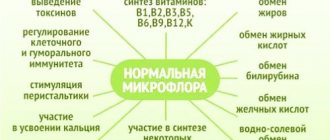
A coprogram is an informative examination that can determine the state of the child’s intestinal microflora. It is responsible for the synthesis of enzymes, vitamins and proteins, and is actively involved in the fight against harmful microorganisms and the formation of the baby’s immunity.
- Accordingly, if the state of the microflora worsens, the child’s immunity and digestion suffer, the synthesis of useful substances and the ability to absorb useful vitamins and minerals are disrupted.
- The intestinal microflora of a newborn is just beginning to form and become populated with beneficial bacteria, which contributes to problems with the process of digestion and bowel movements.
- Indications for prescribing a stool test for coprogram in newborns may be:
- frequent and ongoing attacks of colic;
- green stool;
- the presence of mucus particles or bloody discharge in the baby’s stool.
Nowadays, there are a variety of drugs for colic in newborns. Among them: “Linex”, “Bobotik”, “Sab Simplex”, “Bifidumbacterin”, “Plantex”, “Espumizan L”, “Infacol”, “Baby Calm”, “Plantex”, “Lactobacterin”, “Microlax”, "Smecta". A doctor may recommend stool testing for older children if there are suspicions related to:
- problems of the digestive system, stomach, pancreas, intestines and liver;
- the way fatty, carbohydrate and protein foods are digested and absorbed in the child’s body;
- the presence of parasites in the body;
- the need to identify the causative agent of intestinal infection in order to prescribe the correct antibiotic therapy.
Preparing for the study
Having learned from what was previously stated what stool coprogram is in children, you need to find out how to take this test correctly.
Preparing to submit stool for examination is not difficult; you must adhere to some rules:
- Before donation, it is recommended to stop taking medications such as: anti-inflammatory drugs, antibiotics, antidiarrheals, laxatives, drugs with a high iron content and some others. If the baby cannot refuse to take these medications, then when submitting stool for analysis, it is necessary to indicate information about what medicine the baby is taking and in what dosages. This information will help the doctor make the correct diagnosis;
- notify the doctor if the baby had an enema or rectal suppositories the day before. These actions can also have an impact on the result obtained;
- When preparing to donate feces for coprogram for children under one year of age and older, you should avoid eating foods such as tomatoes, tomato juice, beets and other fruits and vegetables that contain coloring substances. In your child’s diet, you should limit the consumption of fish, greens, and meat. They can be temporarily compensated by eating dairy products, cereals, butter, eggs, and baked goods.
Important! The reliability and accuracy of stool examination depends on how quickly the child’s biomaterial is delivered to the laboratory for diagnosis.
Why are infants given a referral for stool analysis?
In the minds of most people, stool analysis is associated with a suspicion of helminthiasis, and for an infant before independent active movements, the chances of becoming infected with worms are minimal. Therefore, many parents are perplexed by the referral for stool analysis. However, it is the coprogram that allows you to determine the state of the baby’s intestinal microflora.
A newborn’s intestines lack the microflora a person needs for normal digestion, and this causes colic and problems with stool. Bacteria (both beneficial and harmful) enter the baby's body along with mother's milk, gradually populating the intestines, and by the end of the second month the microflora usually returns to normal. At the same time, there are babies who, after two months:
- colic problems continue
- green stool observed
- there is mucus or blood in the stool
Even if these phenomena are episodic, doctors advise in such cases to take a stool test. It is used to determine or evaluate:
- digestive ability of the digestive system and enzyme activity
- absence or presence of inflammatory processes in the intestines
- evacuation function of the digestive system
- state of the microflora (it is found out which bacteria in the baby’s intestines are in insufficient quantities and which are in excess)
Other pathologies in feces
A coprogram for occult blood examines its presence in the stool, which can be a sign of problems in the child’s digestive system. Blood may appear in several cases:
- benign or malignant polyps in the colon;
- haemorrhoids;
- anal fissures;
- intestinal infections that cause inflammation;
- ulcers;
- ulcerative colitis;
- Crohn's disease;
- diverticular disease caused by a disruption of the wall of the colon;
- abnormalities of blood vessels in the colon.
Gastrointestinal bleeding may be microscopic (invisible to the eye) or easily visible as red blood or a black tar called melena.
Results of scatology
Results are issued the next day or one day after submitting a stool sample for testing. The laboratory does not provide for deciphering and explaining the results obtained to the patient. It only gives out a sheet with words and numbers that are difficult to understand for a person who does not have a medical education. You should contact a specialist with the research results. After reading the data received from the laboratory, the doctor makes a conclusion whether pathological processes are occurring in the patient’s body or not. If they are identified, additional studies may be prescribed to confirm the correctness of the diagnosis. Then treatment is prescribed.
How to collect stool from an infant for analysis
The pediatrician wrote out a referral for a stool test for the baby, and the parents faced a difficult task. If older children need to be “caught” on time (material for research must be submitted to the laboratory after a maximum of 12 hours), then there are no problems with the frequency of the infant’s stool. But collecting feces from newborns and children under one year of age is much more difficult.
You can’t put a baby under one year old on the potty on a schedule (or you won’t get the desired result), and it’s quite difficult to remove the contents from a disposable diaper. Therefore, if you need to collect baby stool for analysis, you need to consider a few simple rules:
- You only need to collect material for research in a sterile pharmacy plastic jar (a spoon is attached to it, which simplifies the procedure, allowing you to remove the child’s “product” from a diaper or diaper). The use of any other container may affect the analysis results due to the presence of foreign impurities.
- Hygienic procedures are carried out as usual, since it is difficult to predict in advance the time of a baby’s bowel movement.
- For analysis at this age, one teaspoon is enough.
- Although it is usually recommended to donate stool the same day, you can collect it in an airtight container in the afternoon and place it in the refrigerator until the morning.
- Since the coprogram involves determining the quantity, consistency, etc. feces, you cannot collect material for research after an enema. Some medications also affect the results of the analysis, so you should not use them during the day. Also, before collecting feces, you should discard suppositories.
- If the stool is of a liquid consistency, you can simply pour it from an oilcloth or from a diaper into a plastic container (from the diaper very quickly, until it is absorbed). For a baby in the first months of life (while the baby is not moving much), you can use a special urine collector attached with Velcro. Feces of normal consistency are removed only from the surface of the diaper.
- To collect material for research, it is recommended, if possible, to use diapers without gel filler (from a diaper).
- If the baby is already using the potty, he must first be washed with baby soap and rinsed thoroughly with water - the use of chemicals or a poorly washed potty will affect the results of the analysis.
In order to identify Giardia, feces must be collected while still warm. Pinworms can be determined only by collecting the remains of feces from the folds of the butt (children over one year old are taken for a three-time smear) immediately after defecation - infection with pinworms is determined by the presence of eggs, which females leave around the anus.
How to properly collect feces
Correctly collected material is a guarantee of obtaining results that reflect the current condition of the baby, and this is what is necessary for prescribing the correct treatment.
Collection instructions
How much urine is needed to test a baby?
How to collect feces from a baby for analysis:
- You need to wait until the baby wants to go to the toilet, preparing a sterile container. It is important that this is a spontaneous process. When the child does this at the same time, there is no inconvenience. It is often impossible to predict in advance, so you need to take a sterile container and wait;
- Usually babies go to the toilet after eating. If the baby is almost a year old and sitting, then you can use the potty. Many mothers begin toilet training their children at 6-7 months. The pot must be washed well and wiped dry. Collect the required amount of material from the container with a spoon and close the lid tightly;
- You can take feces from a diaper or diaper, but you need to do this carefully, do not scrape it on the surface, so that the analysis does not contain unnecessary impurities.
How much feces do you need?
There is no need to put as much material into the container as will fit; 5-10 grams of feces is enough. This is approximately one teaspoon. Ideally, if its condition is semi-liquid, mushy. This is exactly the type of stool that a baby should have normally.
How to collect liquid stool
How to collect liquid feces from a baby:
- You can drain it from the surface of the diaper. You need to catch it before it gets absorbed. Immediately after defecation, remove the baby's diaper and transfer the material to a container;
- It’s good if you can put a clean oilcloth under the child so that you can drain it into a container. The main thing is not to use gauze or cloth sheets, otherwise there may be particles of materials in the analysis, which will affect its result.
There are special urinals. These are disposable test bags. They are sold in pharmacies. Their adhesive base is fixed on the child's skin. You can stick it to the baby's bottom and put a diaper on top. It is necessary to ensure that the baby does not toss and turn too much, otherwise the contents of the bag will spill out.
Note! You need to make sure that no urine gets into the analysis. Otherwise, it is better to collect the material again. Do not leave the urine collector for a long time - irritation may appear on the baby’s delicate skin at the attachment point.
Urinals
When is it prescribed?
The reason for prescribing the analysis is the following symptoms in a child:
- Nausea followed by vomiting;
- Acute abdominal pain;
- Sudden weight loss, lack of appetite;
- The appearance of foreign bodies or blood clots in the stool;
- Changes in the consistency, color, smell of feces;
- Increased gas formation, bloating, colic;
- Yellow tint to the skin or eyes;
- Deterioration in the quality of skin, nails, hair.
After identifying the cause of poor health, conservative treatment is prescribed. After a course of therapy, the pediatrician issues a second referral for diagnostics to assess the quality of treatment.