Blood tests
Based on blood tests, liver function is examined and tumor marker levels are determined.
Liver function test
Determination of biochemical parameters - liver enzymes, protein levels and bilirubin - is included in standard diagnostic schemes, but is not a specific method: liver function may be impaired due to other reasons.
Tumor markers for liver cancer
As mentioned above, the main tumor marker for liver carcinomas is AFP. A persistent and rapid increase in the level of alpha-fetoprotein in combination with positive ultrasound results makes it highly likely to suspect the development of a malignant neoplasm, however, some types of cancer tumors are AFP-negative.
How to determine liver cancer if the tumor marker AFP is within the normal range, and ultrasound data and symptoms indicate a high probability of developing a cancerous tumor? In these cases, the levels of other tumor markers - ferritin and neurotensin - can be examined.
Lab tests
Laboratory tests are performed to detect tumors in the liver. Additional information about pathology can be obtained from a blood test. Doctors prescribe general as well as biochemical analysis and blood testing for tumor markers. Let's consider the features and results of each method:
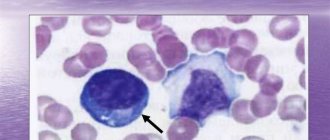
- A general analysis for diagnosing the initial stage of development of inflammation due to a tumor is quite informative. The following disorders may indicate a pathological process:
Blood biochemistry for the liver: normal
change in leukocytes in plasma (significant increase in their level);
- decreased hemoglobin level;
- increased ESR levels;
- low platelet count. However, a diagnosis cannot be made using a general analysis alone. The identified disorders can occur in the human body in the case of other diseases. It is not recommended to decipher the analysis results yourself, as this can only be done by an experienced specialist.
Liver tumor markers
Therefore, the study makes it possible to diagnose the disease even in the initial stages. An elevated tumor marker alpha-fetoprotein (AFP) indicates the presence of primary liver cancer or metastases of other malignant tumors to the liver. The level of AFP is sometimes elevated in other diseases, for example, cirrhosis or hepatitis, so the method cannot be the only justification for diagnosing liver cancer and requires confirmation by hardware methods.
Liver cancer: Ultrasound diagnosis
Ultrasound is the simplest, painless and absolutely safe method of examination for the patient if a malignant neoplasm is suspected. Despite the fact that ultrasound is highly informative, especially in the nodular form of the disease, its results are not enough to make a final diagnosis.
Is it possible to detect liver cancer using ultrasound? Just like the determination of AFP and other markers, ultrasound examination without a comprehensive diagnosis cannot become the basis for a final diagnosis.
Therefore, if, based on the results of the examination, ultrasound and tests, the doctor suspects oncology, the patient is prescribed an additional examination.
Types and symptoms of pathology
Determine primary and secondary liver cancer. In the first case, the tumor develops on the basis of hepatocytes; not so often the source is the cells of the hepatic vessels or bile ducts. Secondary liver cancer develops in parallel with oncological pathologies of other organs. The fact is that when other organs metastasize, pathological cells spread throughout the body most often settle in the liver parenchyma. Secondary pathology develops ten times more often than primary pathology and is more dangerous, since dysfunction of organs affected by cancer is observed.
Before prescribing blood tests and other studies, the specialist collects anamnesis, familiarizes himself with the existing symptoms, and performs an initial examination. Signs indicating the presence of liver cancer are very characteristic:
- painful condition, weakness, nausea and vomiting occur against the background of deteriorating appetite;
- there is a sharp decrease in body weight;
- the liver quickly increases in size, becomes dense and often lumpy, which is determined by palpation;
- discomfort and unpleasant feelings in the hypochondrium on the right side;
- As the pathology progresses, jaundice appears, and a change in the color of the whites of the eyes is especially noticeable.
Modern visualization methods
CT and MRI.
Using various types of tomography, the structure, location and shape of the tumor are clarified, and tissue areas with impaired metabolism are determined.
PET CT is a comprehensive study using modern devices of the latest generation, which allows you to distinguish a malignant tumor from a benign one and determine the presence of metastases.
Angiography.
Intravenous administration of contrast followed by photographs of the liver vessels makes it possible to determine how close the cancerous nodes are to them.
Liver biopsy
Prescribed for elevated levels of liver tumor markers. The procedure allows you to determine the structure of the liver and the extent of damage, as well as accurately determine whether the tumor is malignant. Carrying out a biopsy has a certain degree of risk associated with the high concentration of blood vessels in the liver. Many patients complain of pain during a biopsy.
There are also the following risks:
- if the sampling instrument gets into the vessel, bleeding may occur,
- puncture of the intestines, lung or gall bladder with a needle,
- entry of pathogenic microbes into the body.
After the procedure, it is important that the patient is transported from the hospital. Upon returning home, you need to remain in bed until the next day. During the week, you should not carry heavy objects or engage in physical activity. The examination results will be ready in 7-14 days.
Biopsy for liver cancer
The collection of fragments of liver tissue for biopsy analysis can be carried out in various ways; the choice of a specific method is carried out taking into account the characteristics of the patient and the tumor. Percutaneous, fine-needle, and transvenous biopsies are usually performed under ultrasound or CT guidance.
Laparoscopy.
The procedure is carried out using a special device - a laparoscope, which is inserted into the abdominal cavity through small incisions to examine the surface of the liver, nearby organs and lymph nodes. During laparoscopy, areas of tissue may also be taken for biopsy.
As with the diagnosis of other types of malignant tumors, a biopsy allows you to detect cancer cells, determine their type and degree of differentiation (an important indicator that affects the prognosis).
However, due to the intensive blood supply to the organ, the procedure is associated with a fairly high risk of bleeding. Therefore, invasive diagnostic methods are used infrequently.
In addition, with a diffuse form of the disease, it is usually impossible to determine the location of collection of material for analysis.
It should be added that the choice of the most informative diagnostic methods is the doctor’s task. It is he who decides how to identify liver cancer with maximum accuracy, speed and minimal problems for each individual patient. Therefore, it is necessary to follow the recommendations of a specialist, and not try to “undergo a more accurate study” on your own.
Additional tests
Diagnosis of liver cancer should be carried out taking into account the suspected underlying diseases. These are viral hepatitis B, C, D. They can lead to cirrhosis and malignant transformation of the parenchyma; in addition, their identification influences treatment planning. Detection methods – ELISA, PCR.
In addition, if there are reasons (symptoms, medical history), I recommend tests for patients:
- For markers of autoimmune hepatitis.
- For hemochromatosis (serum iron, transferrin, ferritin, biopsy).
- For Wilson-Konovalov disease (copper, ceruloplasmin).
These studies are carried out only when indicated (for example, if the patient, in addition to signs of liver damage, also has joint pain, acne and other symptoms suggestive of autoimmune hepatitis).
What to do if the tumor marker is elevated?
The determination of tumor markers plays an important role in the diagnosis of malignant diseases. If you receive a laboratory test result with elevated values, do not panic. The first step is to consult a doctor and determine what could have caused the change in the quantitative composition of the markers. This will be helped by both a detailed history taking (with an emphasis on chronic gastrointestinal diseases, liver diseases, lifestyle, diet and addictions) and additional examination.
Tumor markers should not be used as the only method for detecting a tumor. Only through comprehensive diagnostics can it be possible to accurately verify cancer and determine further tactics for patient management.
Interpretation of indicators: norms and deviations
The norms for blood tests for tumor markers for liver cancer depend on the testing systems used. Therefore, information about the normal range of tumor markers is necessarily contained in the study form. They are indicated next to the analysis results.
| Tumor marker name | Content standard |
| Alpha fetoprotein marker | Less than 15 ng/ml |
| Cancer antigen CA 19-9 | Less than 37 units/ml |
| Mucin-like glycoprotein (CA 15-3) | Less than 28 units/ml |
| Glycoprotein CA 24-2 | Less than 30 units/ml |
| CA 72-4 | Less than 4 units/ml |
| Ferritin | Less than (F) 22- (M)30 units/ml |
| B2 –MG beta microglobulin | 0.68-2.3 mg/l |
Indications for research
Tumor markers for liver cancer are advisable to use for:
- primary detection of malignant cells in the organ;
- differential diagnosis of primary disease and metastases;
- assessing the dynamics of pathology progression;
- monitoring the effectiveness of chemotherapy;
- screening of people at risk. This applies to long-term patients with hepatitis and cirrhosis.
Laboratory testing is prescribed:
- before starting chemotherapy, which is necessary to establish the concentration of markers. In the future, dynamics will be assessed only taking into account those indicators that had the maximum values;
- at the end of treatment - required to determine the initial level of indicators after completion of chemotherapy or surgery. This is necessary for subsequent monitoring of dynamics and timely detection of relapse, which is manifested by an increase in tumor markers;
- after treatment - every three months for two years and twice a year - thereafter;
- before changing the chemotherapy regimen;
- a month after the first detected increase in tumor markers.
Indications for tumor marker analysis
Oncologists often use the medical term cancerophobia (fear of cancer). There are quite a lot of people suffering from such a psychological disorder, and they, without compelling reasons or recommendations from a specialist, strive to regularly undergo tests for tumor markers, both liver cancer and other internal organs. But the need for such research does not always exist. Only people with unfavorable heredity – a family history of malignant lesions of the digestive organs – should undergo such tests regularly.
In addition, a specialist may prescribe a test for tumor markers in a number of the following cases:
- the patient complains about the presence of alarming symptoms;
- differentiation of malignant lesions from benign tumors;
- drawing up a protocol for drug therapy and monitoring its effectiveness;
- the need to obtain reliable information about the effectiveness of surgical intervention;
- early detection of relapse of a disease that is in remission or the onset of a metastatic process.
But the decision that a patient needs to undergo such a test should be made only by the attending physician, who will be able to select the required volume of proteins to be tested in each specific case and correctly interpret the results obtained.
Preparation and execution
To ensure accurate results, the following rules should be taken into account:
- Research is carried out on an empty stomach. The biomaterial is collected 12 hours after eating protein foods. One glass of water is allowed.
- A few days before the analysis, alcohol, smoked foods, fried, fatty and spicy foods are removed from the diet. For 5-7 days, sexual intercourse is excluded.
- It is prohibited to smoke and take medications 2-3 hours before the test. If it is impossible to refuse a particular drug, you must notify your doctor about taking it.
- The analysis is performed before the start of antitumor therapy or 1-2 weeks after drug withdrawal.
- It is recommended to avoid psychological and physical stress before the study.
When determining the primary diagnosis, the biomaterial is checked every month, in the second year - every 2 months, in the third - from 2 times a year, thereafter - 1-2 times a year.
What it is?
A laboratory way to confirm malignant liver processes is to determine the concentration of tumor markers in the blood. They are specific substances released during tumor growth. These molecules, which are combined with protein and fat, are synthesized by dividing atypical components. The ability to detect them in the liver is high, since important metabolic reactions occur in this organ.
Tumor markers are protein compounds that, in the absence of a tumor process in the body, are absent in the blood or their quantity is so small that they do not have a harmful effect. These complex substances are inherent only in pathological tissues. An increase in them, in the absence of any symptoms, may indicate a hidden tumor process, which is important for early diagnosis and therapy.
Preparing for tests
Before submitting biological fluid for histological examination, you should go through the preparatory stage:
- One meal half a day before the test. You should eat foods that contain sufficient amounts of protein. Doctors do not recommend eating fatty foods.
- It is strictly forbidden to consume alcoholic beverages, fast food and smoked foods before the procedure.
- Remove physical activity from your daily routine.
- Avoid stressful situations that can lead to mental overexcitation.
- Do not eat food before taking tests.
- Before the procedure, do not use nicotine products for at least two or three hours.
- Limit sexual contact a week before the test.
Before the procedure, the patient is allowed to drink a glass of clean water.
Basic diagnostic methods
Diagnosis of liver cancer consists of an objective examination, the nature of the disease, the results of instrumental and laboratory examination methods.
Visual inspection
Hepatocellular carcinoma develops very quickly. At first, it is characterized by nonspecific manifestations - pain in the upper abdomen, prolonged fever, loss of appetite, weight loss. Typical clinical signs appear later.
Soon the liver begins to enlarge, its lower edge reaches the navel. By palpation you can determine the compaction on the surface of the organ. Late symptoms of cancer are yellowing of the skin, bloating, and dilated veins on the anterior abdominal wall. The face takes on an earthy tint, and noticeable loss of weight in the limbs combined with an enlarged abdomen. Nosebleeds often occur.
History taking
Determining the dynamics of the disease is very important for making a diagnosis. At the first visit to the clinic, the doctor asks the patient about how long ago the complaints appeared and the nature of their development. Next, the order of occurrence of symptoms and its severity are determined. To detect a possible cause of cancer, heredity, concomitant pathologies, and the presence of occupational hazards are studied.
Laboratory research
Laboratory diagnosis of liver cancer is aimed at testing blood and identifying specific markers of a malignant tumor.
General analysis of urine and blood
A general blood test for liver cancer gives the following abnormalities:
- decreased levels of red blood cells and/or hemoglobin – anemia of varying severity;
- an increase in the number of leukocytes, a shift in the leukocyte formula to the left;
- granularity of erythrocytes associated with intoxication;
- significant increase in ESR – 50 mm/h or more.
These blood parameters for liver cancer are nonspecific, as they can be observed in other diseases. Based on them, a diagnosis cannot be made, but a conclusion can be drawn about the presence of a pathological process.
In general urine analysis, changes rarely appear; they can be observed even with advanced oncology:
- an increase in ketone bodies as a result of protein breakdown;
- the appearance of urobilin;
- increase in urea level.
These criteria indicate the degree of metabolic disturbance due to intoxication.
Blood biochemistry
Biochemical tests for liver cancer reveal changes in the following indicators:
- increased globulin levels;
- fibrinogen growth;
- significant alkaline phosphatase activity.
It is important to know! These indicators also cannot be considered basic for making a diagnosis, since they reflect only the degree of liver dysfunction.
Tumor markers
Tumor markers are substances that are detected in the blood only during the development of malignant tumors. For hepatocellular carcinoma, this is alpha-fetoprotein. This tumor marker for liver cancer is a combination of protein and glucose, which is found only in the body of the embryo and fetus. After birth, its amount decreases sharply, almost reaching zero.
Tumor markers for liver cancer are nonspecific; they can also be detected in other cancers. Hepatocellular carcinoma can be suspected if the level of this protein exceeds 1000 ng/ml. If the amount of alpha-fetoprotein is significantly greater than this figure, it is already considered a specific marker of liver cancer.
Preparing for blood collection
Blood for general and biochemical analysis for liver cancer is collected in the usual way. The procedure is carried out in the morning; the person is advised not to eat less than 12 hours before the test. 2-3 days before the test, adhere to the principles of a healthy diet. Blood is taken from the cubital vein, and then it is examined in the laboratory.
Instrumental studies
Instrumental methods allow you to visually assess the appearance of the organ, determine the location, number and size of neoplasms. The interpretation of the studies is given by the doctors conducting them, but the diagnosis is made based on the totality of the data.
Ultrasound
This is the primary method for diagnosing cancer. The tumor itself, its location in the organ, and size are detected. Ultrasound assesses the structural state of the liver tissue. A sign of a neoplasm is a darkened area with uneven edges.
CT and MRI
These two radiation research methods are highly accurate and specific. To perform a CT scan, an intravenous injection of a contrast agent is required - Ultravist or Omnipaque. They contain iodine, which accumulates inside the tumor and makes it more “visible”.
MRI provides a layer-by-layer image of the tissue being studied, making it possible to detect even the smallest tumor. The method is based on the ability of magnetic rays to penetrate organs and reflect from them at different speeds. Also used for differential diagnosis with other diseases. Allows you to distinguish a malignant neoplasm from a benign one. It can be used to determine the condition of the blood vessels inside the organ.
Diagnostic laparoscopy
Indicative when the tumor reaches a large size. In this case, the laparoscopic picture looks like this:
- a large single knot, with an uneven surface, whitish-gray in color, with a dense consistency;
- multinodular form of cancer - several formations of different diameters, brown in color;
- Cirrhosis-cancer - a thickened capsule, many small nodules on the surface of the liver.
Laparoscopy can also reveal the presence of free fluid in the abdominal cavity - ascites.
Angiography
This is a method of studying the liver vessels using an X-ray machine and injected contrast. It is used to assess the condition of the arteries feeding the tumor, on the basis of which a conclusion is made about the possibility of surgical intervention.
Needle biopsy
This type of diagnosis is based on microscopic examination of liver tissue. A piece of the organ is collected using a puncture. Take a long needle with a hollow shaft and pierce the anterior abdominal wall, reaching the liver. The procedure is carried out under ultrasound control. A piece is taken from the neoplasm, then histological material is prepared, which is studied under a microscope.
PAT
Positron emission tomography is a radionuclide research method. This analysis is quite complex and expensive and requires special equipment. A radiopharmaceutical is injected into a vein, then the body is scanned using a positron tomograph. Tumor tissue absorbs much more contrast agent than healthy hepatocytes. Therefore, when transilluminated, it looks much brighter.
Specific tumor markers
For the liver, only alpha-fetoprotein is a specific indicator. There are many other tumor markers, but they can be detected in stomach, ovarian, and pancreatic cancer.