© Author: Z. Nelly Vladimirovna, laboratory diagnostics doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
Normoblasts (normocytes) are the last, still nuclear, stage of red blood cells (erythrocytes) on the way to an adult, full-fledged state. At this stage, normoblasts have a nucleus, so that, having lost it, they can turn into a young, nuclear-free cell containing hemoglobin and already capable of performing the main task of red blood cells (participation in respiration).
Before becoming normoblasts, future red blood cells go through a certain path. As is known, all blood elements originate from a stem cell - it is the ancestor of future leukocytes, platelets, erythrocytes, etc., since it gives rise to several sprouts, among which is the erythrocyte (from it will come the cells of the erythroid series, including, and those of interest to us are normoblasts).
The youngest, morphologically distinguishable cell of the red row is the erythroblast, which was previously called proerythroblast. This is a fairly large cell (14 - 20 microns), containing an equally large nucleus, but does not even have signs of what an adult red blood cell is so valued for - it does not contain hemoglobin.
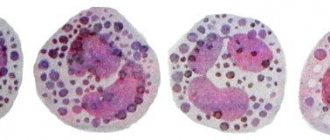
Stages of transition of normoblasts into erythrocytes
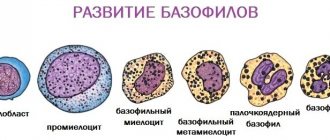
It will take a little time for the described blood cells to transform into red blood cells. Initially, the development of a basophilic erythroblast is observed, in the central part of which there is a nucleus. It is characterized by the presence of a round shape and a size of 18 microns.
These cells have a rich blue color. Subsequently, polychromatophilic erythroblasts are formed from them, which are smaller in size than basophilic ones. These cells are characterized by the presence of a wheel type of chromatin, and the cytoplasm acquires a pink-blue color.
Subsequently, the present erythroblast is converted into an oxyphilic form. Such cells are characterized by the presence of a fuzzy purple nucleus. The cell becomes even smaller and more closely resembles an erythrocyte.
Over time, the cell nucleus becomes pyknotic, and the cytoplasm becomes light blue. This indicates the transition of the erythroblast to the polychromatophilic form. The cell then transforms into reticulocytes. And only at this stage are red blood cells formed in the blood without a nucleus.
Blasts are... Definition, concept, norm and pathology, interpretation of tests
If leukemia is suspected, doctors will prescribe a blood test for blasts. This study helps to promptly identify a dangerous disease and begin treatment as early as possible. How to properly prepare for taking a sample? And how to decipher the results of the analysis? We will consider these questions in the article.
What it is?
Blasts are immature blood cells that are produced in the bone marrow. They are subsequently converted into red blood cells, white blood cells and platelets. Blast cells are the precursors of mature blood cells.
In a healthy person, blasts in the bone marrow make up no more than 5% of the cells. In infectious diseases, their concentration can increase up to 10%. However, normally immature cells should not enter the bloodstream. They can only be located within the bone marrow.
In severe hematological pathologies, the patient develops blasts in the blood. What does it mean? This analysis result indicates oncological diseases of the hematopoietic system. With these pathologies, an excessive amount of immature elements is formed in the bone marrow. Excess blasts are released into the bloodstream. Their presence in the analysis is an alarming sign.
In the initial stage of blood cancer, the bone marrow may contain about 40% blast cells. Subsequently, a malignant tumor is formed from these immature elements.
Blood analysis
How to detect the presence of blasts in the bloodstream? This can be done using a general blood test. This study shows the number of mature and immature cells.
For the sample, blood is taken from a finger or from a vein. The biomaterial is studied under a light microscope. This device has a special grid for counting blood cells. With its help, the concentration of blasts is determined. In the analysis transcript, the number of immature cells is indicated as a percentage.
In what cases do doctors prescribe a blast test? This test is indicated if the patient has the following symptoms:
- swollen lymph nodes;
- causeless increase in temperature;
- enlarged liver and spleen;
- weakness;
- severe inflammation of the tonsils;
- red dots on the skin;
- increased bleeding.
Very often, patients mistake these manifestations for signs of tonsillitis and other infectious diseases. However, such symptoms may indicate the presence of severe bone marrow pathology. For the purpose of differential diagnosis, doctors prescribe an analysis for the presence of blasts in the blood.
Preparing for analysis
A sample for blast cells is usually taken in the morning, on an empty stomach. The analysis results are most often ready the next day.
What rules must be followed before taking biomaterial for blasts? This study does not require complex preparation. You must adhere to the following recommendations:
- stop eating 8 hours before the test;
- do not drink alcohol on the eve of the study;
- Avoid smoking 2 hours before taking blood.
It is also recommended to stop taking medications 3 days before the test. If the patient cannot interrupt the course of drug treatment, then you need to tell the doctor about all the medications you are taking.
Decoding
Normally, blasts should be absent from the analysis. In this case, the study results indicate that their rate is 0%. A healthy person can only have mature elements in their blood.
If even a small percentage of blasts is present in the analysis, then this is a dangerous sign. The test results must be shown to the doctor and treatment must begin immediately.
Reason for deviation: leukemia
The main reason for the appearance of blast cells in the sample is leukemia. This disease is otherwise called leukemia or blood cancer. The pathology is accompanied by uncontrolled division of immature cells in the bone marrow, which subsequently form a tumor.
Doctors distinguish two forms of leukemia:
In acute leukemia, a huge number of blast cells are found in the blood. Their concentration can be more than 20%. In the chronic form of blood cancer, the rate of immature elements usually does not exceed 5-10%.
Other blood indicators
When studying the results of the analysis, the doctor must pay attention to other indicators of the clinical study. The presence of blast cells in the biomaterial is always considered in combination with other blood parameters. The presence of leukemia may be indicated by the following data:
- Leukocytosis. In approximately 15% of patients with acute leukemia, the white blood cell count is tens of times higher than normal.
- Low hemoglobin. Patients with blood cancer have severe anemia and a decreased number of red blood cells.
- Drop in platelet levels. For this reason, patients with leukemia experience increased bleeding.
- Decrease in reticulocytes. These cells are young forms of red blood cells. Their small quantity leads to anemia.
- Complete absence of eosinophils and basophils. This causes a sharp decrease in immunity.
The above signs, together with the appearance of blast cells in the blood, allow the doctor to diagnose leukemia.
Bone marrow examination
If blasts are detected in a patient's blood, doctors usually prescribe a bone marrow puncture. The examination is carried out under local anesthesia. A special long needle is used to make a puncture in the sternum or spine and take a piece of bone marrow tissue for examination.
The punctate is examined using a microscope. The amount of mature and immature blood elements in the biomaterial is determined. An increase in blast cells up to 10% does not always indicate leukemia.
This study result is possible in case of severe stress or an infectious disease. If the concentration of blasts exceeds 30%, then this is most often a sign of blood cancer.
At the same time, the patient’s number of red blood cells, platelets and leukocytes in the puncture material decreases.
If leukemia is suspected, a cytochemical analysis of the punctate is also performed. It allows you to detect the level of enzymes in blast cells. These substances react with some dyes, which is what is used in laboratory research. Positive test results indicate leukemia. By measuring the level of each blast enzyme, the form of blood cancer can be determined.
Treatment
What to do if a blood test shows the presence of blast cells? In these cases, the doctor usually prescribes a number of additional tests. The most informative of them is a bone marrow puncture. An excessively high number of blasts in the punctate is a sign of leukemia.
If the diagnosis of leukemia is confirmed, then it is necessary to immediately begin treatment. It is important to remember that in the early stages of blood cancer it is quite possible to achieve complete or partial remission. The following methods of treating leukemia are used today:
- Chemotherapy. The patient is prescribed cytostatics that suppress the growth of tumors in the bone marrow. This treatment can take quite a long time.
- Blood transfusion. The patient is given intravenous red blood cells and platelets obtained from a donor. This helps raise hemoglobin levels and reduce bleeding.
- Radiotherapy. This type of treatment is indicated for chronic leukemia. The patient is irradiated with enlarged lymph nodes and the spleen area.
- Antibacterial therapy. Patients with leukemia are very susceptible to infectious pathologies. In order to prevent such diseases, courses of antibiotics are prescribed.
- Bone marrow transplantation. This operation helps to completely get rid of leukemia. The difficulty of transplantation lies in the fact that a foreign hematopoietic organ does not always take root.
After complex therapy, a repeat bone marrow puncture is performed. If the concentration of blasts has decreased to 5%, then doctors talk about complete remission.
If the rate of immature cells does not exceed 20%, then remission is considered partial. In any case, the patient must follow the doctor’s recommendations for life. Leukemia is a dangerous and serious disease.
Even with complete remission, relapses of the pathology cannot be ruled out.
Source: https://FB.ru/article/421713/blastyi—eto-opredelenie-ponyatie-norma-i-patologiya-rasshifrovka-analizov
Causes of normoblasts
Normoblasts are formed and transformed in the human bone marrow. As a result, the number of 0.01 normoblasts in a general blood test is considered a deviation from the normal value. These cells should not enter the peripheral blood. Their detection on a hemogram is a sign indicating the possible formation of serious diseases associated with hematopoiesis or brain structure.
The causes of normoblasts in a general blood test include the following:
- Hemolytic type of anemia.
- Various forms of leukemia or erythroleukemia.
- Brain cancer.
- Tumors of a malignant nature.
- Problems with blood circulation.
- Severe blood loss.
- Formation of metastases in the bone marrow.
An increase in the number of normoblasts in the blood is considered especially dangerous after surgery. The presence of these cells indicates a serious condition of the patient.
In this case, the presence or absence of blood cells, and not their number, acts as a diagnostic element. Even the slightest deviation from zero is a sign of a pathological process. But do not get upset ahead of time, because the appearance of normoblasts may be associated with the presence of prolonged inflammation or hypoxia.
From birth to great achievements
However, by focusing on the names, we have deviated somewhat from the topic. So, the events take place in the bone marrow:
Stage 1: erythroblast
The erythroblast is the first cell that can be identified under a microscope in a bone marrow specimen. A rounded nucleus, a delicate mesh structure of chromatin, several small nucleoli (usually 2 - 4), no clearing around the nucleus yet - this is the morphology of the ancestor of cells that will later become erythrocytes. In a general analysis of the blood of a healthy person, you don’t even need to look for it, since it simply cannot be there, because it has only just arisen and, before it goes “out into the world,” it must acquire new features and qualities in order to become workable in the peripheral blood, and, therefore, useful.
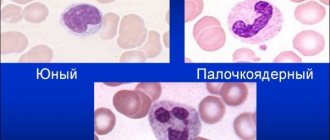
Stage 2: pronormocyte
Having passed the erythroblast stage, a very young cell slightly reduces its size (10 - 15 microns) and begins to change the structure of the nucleus, so that later it is easier to get rid of it (the nucleus becomes smaller and coarser, the nucleoli disappear, a slight perinuclear clearing appears around the nucleus) - this is no longer erythroblast. The new cell is called a pronormocyte in a new way, although some continue to call it in the old way - a pronormocyte. At this stage, the cell of the erythroid series is very poorly differentiated in the myelogram, because it has not yet completely lost the features of its predecessor, and has not yet acquired new ones.
Stage 3: normoblast (normocyte)
However, very little time passes before the “hero of our story” appears from an unrecognizable cellular structure - a normoblast or normocyte. It begins to be saturated with hemoglobin, which first concentrates around the nucleus (basophilic normocyte), and then spreads to the entire cytoplasm, turning the cell into a polychromatophilic normoblast, that is, the cell is clearly preparing to perform its responsible function.
As normoblasts accumulate complex chromoprotein (Hb), the need for the nucleus disappears; it only prevents the accumulation of hemoglobin by its presence. Having received a sufficient amount of Hb, the normocyte becomes oxyphilic: the cytoplasm spreads over almost the entire territory, the nucleus loses its significance, therefore it becomes very small (pyknotic), coarsened with a structure changed beyond recognition, reminiscent of a cherry pit.
Stage 4: birth of a red blood cell
A normoblast, which is about to get rid of a nucleus that is no longer needed, remains a normoblast for some time, but in small numbers. Having finally pushed out the nucleus, the cell turns into a “newborn” polychromatophilic erythrocyte, retaining a small amount of hereditary information (RNA), which will finally leave the cell within 24 hours, although it is difficult to call the “newly formed” form a cell (rather, also out of habit).
Young red blood cells, saturated with hemoglobin and having lost their last connection with their “homeland,” are called reticulocytes, which very soon, after arriving in the bloodstream (up to 48 hours), will lose the last thing that emphasizes their young age - reticulum, and turn into full-fledged adult blood cells - erythrocytes. A special stain helps detect reticulocytes in the blood. The entire path traveled by an erythrocyte from an erythroblast to a cell that has lost its nucleus takes at least 100 hours.
It is obvious that normally red cells at the normoblast level (before it becomes a reticulocyte) do not appear in the blood of a healthy person of all ages.
Normoblasts in a child's body
Hematopoiesis in a child’s body is significantly different from an adult’s, so normoblasts in a general blood test are considered a completely normal process, which is explained by the fact that during birth the bone marrow, which is responsible for the production of blood cells, is located in all bones, both flat and tubular types. A heavy load, as well as increased synthesis of erythropoietin by the child’s kidneys and liver, leads to physiological changes. And they, in turn, entail the release of a small number of normoblasts into the blood.
The maximum number of normoblasts in the analysis is found in infants aged 2 to 3 months. A small number of normoblasts may be periodically detected throughout the early developmental period.
It is worth noting that normoblasts in a child’s general blood test may also indicate pathology, in particular, the development of a disease such as an acute form of lymphoid leukemia. This disease requires immediate treatment, since in advanced stages it can even cause death.
The appearance of normoblasts in a general blood test, norms and abnormalities, causes and symptoms
Normoblasts are formed and transformed in the human bone marrow.
As a result, the number of 0.01 normoblasts in a general blood test is considered a deviation from the normal value. These cells should not enter the peripheral blood. Their detection on a hemogram is a sign indicating the possible formation of serious diseases associated with hematopoiesis or brain structure. The causes of normoblasts in a general blood test include the following:
- Hemolytic type of anemia.
- Various forms of leukemia or erythroleukemia.
- Brain cancer.
- Tumors of a malignant nature.
- Problems with blood circulation.
- Severe blood loss.
- Formation of metastases in the bone marrow.
An increase in the number of normoblasts in the blood is considered especially dangerous after surgery. The presence of these cells indicates a serious condition of the patient.
In this case, the presence or absence of blood cells, and not their number, acts as a diagnostic element. Even the slightest deviation from zero is a sign of a pathological process. But do not get upset ahead of time, because the appearance of normoblasts may be associated with the presence of prolonged inflammation or hypoxia.
If there are no pathologies in the human body, then normoblasts are always in the red bone marrow, practically not penetrating into the bloodstream. That is why the norm of normoblasts in a general blood test is zero. The only exceptions are small children, who have a small number of these cells and are not considered a pathology.
Therefore, if in a general blood test there are 2:100 normoblasts, then this is a clear sign of pathology.
Early diagnosis of leukemia significantly increases the chances of cure, so it is recommended to consult a doctor immediately after the following symptoms appear:
- pale skin;
- feeling of weakness;
- dizziness;
- problems with blood clotting;
- deterioration in the functioning of the immune system;
- excessive fatigue.
If, against this background, a normoblast result of 1:100 is detected in a general blood test, then this may indicate the occurrence of leukemia (high blood cell counts may also indicate the presence of this pathology).
Blood is tissue in a liquid state. The liquid physical state does not detract from its qualities as a full-fledged human organ. It is as important as nervous, muscle and bone tissue. The bloodstream consists of a substance that connects cells - plasma and other components. According to evolutionary laws, these stem cells were transformed, losing their distinctive features.
Unchanged components of the blood flow can remain in their original form throughout the life of the body.
Red blood cells
Red blood cells are classified among the transforming components, which, according to the laws of existence and development of the human body, have lost their cellular characteristics. It is they who are entrusted with the most important function - the delivery of oxygen and carbon dioxide to all tissues and organs. Because red blood cells lack a nucleus, they are not cells.
A normoblast, or normocyte, is a stem cell sprout, or the initial molecular stage of transformation into a full-fledged erythrocyte. Let's look at what normoblasts are in the blood. They are distinguished by the presence of a nucleus with two or three bases.
Normoblasts
Like all primary cells of the human body, a normoblast arises from a stem cell - the founder of all living things. The entire process of formation, growth and transformation into a red blood cell occurs inside the bone marrow. From the moment of its molecular state to the red blood cell carrying oxygen through the bloodstream, the normoblast goes through several stages of formation:
- Generation from the smallest particles of erythroblast. These are cells that are visible under a microscope in the bone marrow material being examined. They have a nucleus with several bases and chromantin (the membrane around the nucleolus).
- Transformation of sprouts into pronormocytes. This is a more complete form of a hypothetical red blood cell. Since the nucleus inside the shell, changing, becomes hardened and small in size, the cell decreases. In a similar way, the pronormocyte prepares for release from the excess part.
- Creation of a normocyte. At this stage, the cell is filled with hemoglobin. It changes color, becoming red, and acquires the properties of red blood cells. At this stage, the core shrinks. Since the human erythrocyte does not have a nucleus and can accommodate more hemoglobin inside and deliver much more oxygen to tissues and organs, this fact becomes a distinguishing feature of the human erythrocyte from the nuclear blood cells of an animal.
- The birth of a red blood cell, or erythrocyte. A reticulocyte is a cell that detaches from a place in the bone marrow and sets off to float freely. One to two hours after entering the bloodstream, it becomes a complete red blood cell, performing its duties.
The transformation takes approximately four days and four hours, or 100 hours.
The term “normoblast” has the main part of the word “norm”; this fact is not perceived by most people as critically as we would like.
The presence of this calming root, it would seem, does not bode well; it seems to indicate that the presence of normoblasts in the bloodstream is normal. However, this is a superficial perception and an illusion.
This means that normoblasts are so named not because of their proper presence in the blood, but because of their normal size, in contrast to megaloblasts that are identical in origin.
Magaloblasts
For a healthy body, the characteristic location of normoblasts is the place where they form into full-fledged red blood cells. And only when the period of disappearance of the nucleus is completed, it can enter the bloodstream.
Without pathologies or negative deviations, the quantitative norm for the presence of normoblast in the analysis material should be 0.
There is only one possible variant of the norm with the presence of a defective normocyte in the blood - a newborn child. In the first two to three months, the baby undergoes physiological formation of all tissues, including bone, so the presence of a small number of normocytes cannot be ruled out.
For a newborn, the presence of normoblasts in the blood is allowed
During this period of time, blood components appear quickly; some of them may enter the bloodstream without fully maturing.
Regardless of gender, normocytes are found in the red bone marrow of flat and tubular bones. Normoblasts are not detected in the blood of a small child older than 3 months.
After three months of life, all processes in the baby returned to normal, and a small number of normocytes should be alarming.
The occurrence or presence of blasts in the blood is interpreted by specialists as a pathology. And an increase in their number is a threatening sign, signaling diseases with negative transformations in the bone marrow.
Such test results are an urgent reason to visit an oncologist or a blood specialist. A number of diagnostic measures are strictly required. For example: repeated blood tests, radiography and MRI. An increased rate is a dangerous circumstance. Every minute is important here, since we are talking about leukemia.
Leukemia
Since the presence of normocytes in the blood is a deviation from the norm, there cannot be a decrease in their number. We are talking about a decrease in the content of red blood cells, or “followers” of normoblasts, in the blood.
In other cases, dilution of red blood cells occurs with a large volume of plasma (unconfirmed or slight decrease in the content of red blood cells), and there is a threat of a real failure of the synthesis of red cells.
All of the above is a description and symptoms of diseases of bone marrow tissue due to radiation exposure or due to iron deficiency.
Possible reasons
Normoblasts increase in size under many circumstances. They are not interdependent, but always have depressing consequences. The most common disease that provokes the presence of normocytes inside the bloodstream is Di Gugliermo’s pathology. This is a type of cancer. Primary signs include a low platelet count, which implies bleeding and death.
The disease is characterized by a rapid decline in the number of red blood cells in the blood, which is destructive because oxygen starvation occurs in organs and tissues.
Cancer and leukemia affect people who have been exposed to radioactivity during nuclear tests and man-made disasters. Another cause may be benzene, pesticides, and many others. etc.
Treatment of such diseases is carried out with chemotherapy; other options for relieving the condition do not provide the desired effect.
In addition to all of the above, there are situations in which blasts are detected in the blood - these are cases that lead to large blood losses. These include injuries, severe wounds, and ruptures of internal organs in women during childbirth. In such circumstances, accelerated hematopoiesis can increase the number of normoblasts, during which some blood fragments simply do not have time to clot.
Trauma during childbirth causes an increase in normoblasts
In cases where normoblasts are detected in a general blood test, it is immediately necessary to repeat the analysis more thoroughly in order to exclude or confirm the presence of a serious disease.
Adult men and women, regardless of age, finding that normoblasts in a general blood test are elevated, have every reason to be wary. When conducting appropriate tests, you should pay attention to your own feelings and well-being. Often the reasons for such alarming indicators can be:
- Chronic anemia, or iron deficiency.
- Bleeding and large volume of blood loss.
- Severe and frequent infectious diseases.
In many general blood test tables, abs (normoblast) values vary by no more than 0.32. Sometimes inside the peripheral blood of children (sampling of biomaterial from a finger) there can be such values, this is not scary. Today there are centers with highly sensitive instruments - analyzers. Such high-quality equipment is capable of determining the composition of any, even peripheral capillaries.
- Home » Blood test » Nrbc in blood test what is it
- More than fixing bugs
- Because nucleated red blood cells (NRBCs) are similar in size and nuclei to lymphocytes, many hematology analyzers misclassify NRBCs, resulting in incorrect white blood cell and lymphocyte count totals.
Decreased number of normoblasts
Since the norm of normoblasts in the blood is 0, then their number cannot be reduced.
Only the number of red blood cells that are formed from normoblasts can be reduced. Red blood cells can be diluted with a large volume of liquid, or their normoblasts can actually form in smaller numbers.
The latter problem is observed in the presence of various bone marrow diseases as a consequence of radiation exposure. But the main cause of this condition is recognized to be a deficiency of iron, which is required to create hemoglobin.
What are normoblasts?
Blast cells are an intermediate form of erythrocytes (red blood cells), responsible for saturating body tissues with oxygen, as well as removing carbon dioxide from the body. These substances are formed, like all formed elements of blood, in the bone marrow. Blue-violet cells at this stage of development are actively enriched with hemoglobin, which provokes a decrease in the nucleus. When it is completely dissolved, normoblasts will acquire smaller sizes and transform into pinkish reticulocytes.
Symptoms of leukemia
Early diagnosis of leukemia significantly increases the chances of cure, so it is recommended to consult a doctor immediately after the following symptoms appear:
- pale skin;
- feeling of weakness;
- dizziness;
- problems with blood clotting;
- deterioration in the functioning of the immune system;
- excessive fatigue.
If, against this background, a normoblast result of 1:100 is detected in a general blood test, then this may indicate the occurrence of leukemia (high blood cell counts may also indicate the presence of this pathology).
What is acute leukemia?
Acute leukemia is a consequence of a disruption in hematopoiesis in the initial stages. In a normal state, blast cells turn into functional blood cells and fulfill their mission. Each such little body immediately after “birth” has its own line of development. For example: for erythrocytes one type of such cells is “produced”, and for leukocytes another, and so on.
When the hematopoietic system fails and the creation of healthy base cells is disrupted, the corpuscles behave differently. They do not turn into “working” cells - they only consume useful substances and multiply. Over time, they replace healthy cells and penetrate the bones, destroying them without supplying useful substances. The number of useful cells sharply decreases, hemoglobin, platelets and leukocytes drop.
This disease is lymphoblastic and myeloblastic - depending on what type of cells became the “culprit” of the disease. They are divided into other, smaller categories, depending on the purpose of the damaged blast elements.
They can be designated, for example: acute B-lymphoblastic leukemia, which implies a failure in the creation of blasts at the level of “production” of elements such as B-lymphocytes, or acute monoblastic leukemia, which arose due to problems in the creation of monocytes. Depending on the degree of complexity and type of leukemia, the prognosis for a patient’s cure varies.
Diagnosis of leukemia
If there are symptoms characteristic of leukemia, the doctor first sends the patient for a hemogram and a blood test to detect blast cells. Thanks to the analysis, an accurate indicator of all atypical blood elements will be obtained, which will reveal the extent of the spread of the disease. In the case of leukemia, a general blood test reveals a decrease in the number of platelets. In parallel with this, there is an increase in ESR and the number of normoblasts in the blood.
In addition, the following diagnostic studies may be prescribed:
- blood chemistry;
- study of immunoenzymes;
- myelogram (bone marrow biopsy).
Only after studying all the data obtained as a result of the presented research methods, the doctor is able to make a diagnosis.
Diagnosis of blast cells in the blood
In order to timely determine whether a patient has cancer, a blood test for cancer or leukemia is usually done. If a doctor detects blast cells in a blood test, this is considered a sign that the patient has acute leukemia in the blood.
What it is
Blast cells in a blood test, what are they? They are immature cells from which normal blood cells are then formed. Normally, they are not found in the circulatory system, but are always found in the bone marrow, therefore, after this analysis, the bone marrow is also checked for the presence of normoblasts.
Normal blood and leukemia
Medicine divides blood leukemia into two types - this is a chronic form of leukemia (consists of mature and immature elements), and it never turns into an acute form of leukemia (in which blasts are detected in the blood). In acute leukemia, these cells are a tumor component in the human body.
Typically, this form of the disease is named after the cells whose precursors are immature blast cells, for example, these can be myeloblasts, lymphoblasts, monoblasts, erythroblasts. Thus, acute myeloblastic leukemia, acute lymphoblastic leukemia and other forms of blood cancer are distinguished.
There are no specific symptoms of blast cells in the body that can be used to determine the presence of leukemia in the blood, but the sooner you feel unwell and take a general blood test, the faster a specialist will be able to identify this pathology. It should be remembered that the acute form of blood leukemia, in most cases, occurs in children.
Features of the analysis
To diagnose an acute form of leukemia, you need to take a general blood test and from it a specialist will determine what diseases you have. If the number of red blood cells is reduced, then the anemia is said to be normochromic.
Most likely, such an analysis of blast cells will also reveal a reduced platelet count. In rare cases, their number is greatly increased, and they have oddly shaped nuclei.
ESR (erythrocyte sedimentation rate) is increased in acute forms of leukemia, but there are cases when it is normal.
Automatic Leukocyte Analysis System
You should know that normally there are no blast cells in a blood test, since they are located in the bone marrow and do not extend beyond it. The first symptom of blood leukemia, however, is a high level of white blood cells, which are found in the blood along with blast cells.
In any case, one general blood test does not diagnose leukemia. If cytopenia is not clear, then a puncture test is taken from the bone marrow.
There are cases in which this procedure shows that platelets are normal and there are no blast cells in the blood, and when a puncture is taken from the bone marrow, it is determined that the blasts are also within normal limits, but if the specialist has doubts about the diagnosis, then a trephine biopsy is performed, which finds Cell proliferation in the blood is what determines the presence or absence of the disease.
In vitro, blast cells are determined in a blood test in different ways and repeated blood testing is carried out, which will help make the correct diagnosis.
Carrying out analysis
The test for blast cells and cancer, as always, is taken in the morning on an empty stomach and no special preparation is required for it. Blood is drawn from a vein.
If a blood test for leukemia is taken in the morning, then in the laboratory it is much easier to determine normoblasts and other cells that indicate abnormal abnormalities in the patient’s body.
Of course, such a study is carried out at the request of the patient if he begins to notice poor health and other signs of illness.
However, it should be remembered that the acute form of leukemia in women and men usually passes quickly, therefore, the earlier the diagnosis was made, the better.
This disease, in most cases, occurs in children, so it is easy to identify abnormal cells that quickly spread in the body. Therefore, doctors advise parents to regularly submit such a blood test to their children in the direction of a pediatrician.
If there are symptoms characteristic of leukemia, the doctor first sends the patient for a hemogram and a blood test to detect blast cells. Thanks to the analysis, an accurate indicator of all atypical blood elements will be obtained, which will reveal the extent of the spread of the disease. In the case of leukemia, a general blood test reveals a decrease in the number of platelets. In parallel with this, there is an increase in ESR and the number of normoblasts in the blood.
In addition, the following diagnostic studies may be prescribed:
- blood chemistry;
- study of immunoenzymes;
- myelogram (bone marrow biopsy).
Only after studying all the data obtained as a result of the presented research methods, the doctor is able to make a diagnosis.
What it is
Purpose of a myelogram
To determine the cause of an increase in the number of normoblasts in the blood, a myelogram is often prescribed. The analysis is a study of the condition of a smear taken from the bone marrow through a biopsy. The procedure is performed under local anesthesia. The puncture is performed in the area of the sternum or ilium.
The procedure does not require special preparation or any restrictions. If a person is taking medications, then before the procedure he must inform the doctor about this, and if possible, temporarily stop using the medications. The result of the study can be obtained after just a few hours.
Preparing for diagnosis
Having received the results of a general analysis, the attending physician will never evaluate only one of its parameters, without paying attention to the others.
To ensure that the balance of the quantitative content of all blood cells in addition to normoblasts is not artificially disrupted, you should adhere to certain preparation rules for several days before diagnosis.
A week before the procedure, you need to inform the specialist about the list of medications you are taking so that he can assess the degree of their effect on the composition of the blood. If certain medications cause undesirable changes, their use may be temporarily suspended. In 3–4 days, harmful foods and drinks are removed from the diet, especially fast food, alcohol, marinades, fatty and fried foods.
It is also necessary to stop sports activities for 1-2 days; running and swimming are no exception. You should visit a medical facility on an empty stomach. Smoking is prohibited before diagnosis. If the patient hastily came to the clinic, he definitely needs to catch his breath before entering the office.
Treatment
There is no treatment for elevated levels of normoblasts in the blood. They disappear on their own after successful treatment of the underlying pathology is completed.
It is very important to identify the reason that provoked the increase in normoblast levels in the blood. After the pathology is detected, therapy is carried out, thanks to which the process is either completely stopped or a state of stable remission is created for the patient in chronic forms of the disease.
The most terrible disease, which may be indicated by elevated normoblast counts, is leukemia.
Treatment methods for leukemia
If it is confirmed that elevated normoblast counts indicate the presence of leukemia, then treatment of the pathology includes the following manipulations:
- Chemotherapy. Prescribed if the malignant nature of the pathology is confirmed. During this procedure, all affected cells are destroyed.
- Radiation therapy. Provides relief from the process of tumor growth in the affected area.
- Biotherapy. It is used at the final stages of treatment of the disease or when it is mild. It involves the use of special medications that act as analogues of substances produced by a healthy body.
- Targeted treatment. Based on the use of monoclonal bodies for therapeutic purposes. It is an alternative to chemical therapy in the initial stages of treatment of the disease.
If the disease is in an advanced state, then the only way to cure it is through stem cell transplantation. This is a rather labor-intensive process that requires a lot of professionalism and money.
Therapy for erythromyelosis
Having understood what normoblasts are in the blood, what this means for children and adults, it should be noted that elevated levels of these blood cells can directly indicate the presence of such a serious disease as erythromyelosis.
This disease is characterized by the following symptoms:
- severe weakness;
- bruising;
- painful sensations in the bones;
- weight loss;
- difficulty breathing;
- the formation of a fungal infection.
In the absence of quality therapy, pathology can provoke the formation of a focal type of necrosis of the spleen, swelling of the lymph nodes, bleeding from the nose and gums, as well as hemorrhages in the retina.
Such complications develop as a consequence of the fact that the cells containing the nucleus penetrate through the circulatory system into the internal organs, digestive and reproductive systems, and enter the skin and muscles.
In some cases, diseases that are characterized by an increased level of normoblasts, after about six months or even faster, cause death.
Therapy for this dangerous disease consists of several sessions of chemical or radiation therapy. In addition, the patient can have stem cells transplanted.
Rarely, people may develop a chronic form of erythromyelosis. Diagnosing this pathology is quite difficult, because, despite the presence of a tumor, red blood cells containing nuclei do not penetrate into the blood.
The presented diagnosis can be confirmed by a detailed study of the condition of the internal organs, since the liver and spleen are enlarged in size, and swelling of the lymph nodes develops.
This form of the disease has a long course (over 2-3 years). To rid the patient of pathology, doctors perform multiple transfusions of red blood cells. An alternative method of therapy is the introduction of a special medicinal serum, but a greater effect is achieved through stem cell transplantation.
Acute myeloblastic leukemia
Acute myeloid leukemia (AML) is a malignant process in the bone marrow that impairs hematopoietic function. The disease affects the myeloid lineage. A healthy leukocyte cell does not mature and enters the bloodstream in an altered form. Uncontrolled division begins. Leukocytes lack the ability to protect the body from microorganisms and infections. The production of red blood cells and platelets is inhibited. Anemia and thrombocytopenia begin to develop. The composition of peripheral blood changes.
The reasons that provoke the development of the disease are not fully understood. Scientists associate a number of factors with mutations in the hematopoietic system, for example, heredity, radiation or genetic abnormalities.
Myeloid leukemia is most often diagnosed in adult patients. The disease affects people after 50 years of age. The peak age for cancer is 63 years of age. Older men are more susceptible to myeloid leukemia. Among the younger generation, both sexes suffer equally.
In children, the disease is primary. A child is exposed to leukemia due to anomalies in the genetic code, when the mother comes into contact with heavy toxic substances (radiation, carcinogens) or if the medical history of blood relatives contains oncological pathologies. Symptoms of the disease are the same as in adults.
At the beginning of the disease, the clinical picture is blurred. Gradually, the patient notices unusual changes in his condition. In the acute course of the disease, the patient notes symptoms of well-being:
- Fatigue;
- Dyspnea;
- Bruises and minor bruises;
- Bleeding of the oral mucosa;
- Infectious lesions of the body that are not amenable to classical treatment and have pronounced symptoms.
For terminal stage leukemia, the bone marrow becomes ineffective, and metastases affect the organs and systems of the human body. This is characterized by signs:
- Significant weight loss;
- Paleness of the skin;
- Gastrointestinal and nasal bleeding;
- Weakness;
- Pain and aching bones;
- Fainting;
- Vomiting blood;
- Black chair;
- Stomach ache;
- If the genitourinary system is affected, partial or complete urinary retention is noted.
Treatment is carried out by oncohematologists. ICD-10 code for myeloid leukemia C92.
general characteristics
Precursors of blood cells are divided into 2 large groups - lymphocytic and myelocytic lineage. The lymphocytic germ creates lymphocytes: cells “responsible” for immune reactions. The myelocytic lineage develops (differentiates) into erythrocytes, platelets, neutrophilic leukocytes and granulocytes. Immature blood cells are called blasts.
Thus, acute myeloid leukemia is a tumor that arises from immature cells of the myelocytic lineage of hematopoiesis.
The diagnosis is considered established if the bone marrow analysis (myelogram) shows more than 20% blast cells.
Classification of oncological pathology
Non-lymphoblastic leukemia represents a group of subtypes of the disease. For each species, the chances of survival and treatment tactics are selected individually.
The FAB system consists of 9 types of acute myeloid leukemia. The forms differ in the types of leukocyte precursors and their degrees of maturity. Cells are determined by microscopic and cytogenetic examination.
Blood cells at 1000x magnification
- M0 indicates minimally differentiated acute myeloid leukemia.
- M1 characterizes myelocytic leukemia without maturation. In single blasts, azurophilic granules and Auer rods are found.
- In M2, leukemia is characterized by maturation. Blasts predominantly contain Auer rods and azurophilic granules.
- M3 denotes the acute form of promyelocytic blood cancer. The cells are hypergranular. Auer rods are present in multiples.
- M4 represents an acute myelomonoblastic oncological process.
- In M4eo, myelomonocytic pathology is observed with an increased level of eosinophils in the bone marrow.
- M5 defines acute monoblastic (-cytic) leukemia.
- M6 characterizes acute erythroid blood diseases.
- M7 stands for megakaryoblastic leukemia.
- Subtype M8 represents basophilic anemia.
Treatment tactics
Treatment is carried out in a hospital setting, where contact with the outside world is reduced. Clinical recommendations are to administer chemotherapy. The hematologist-oncologist selects the appropriate protocol for each case. When diagnosed with acute myeloid leukemia, doctors select a combination of drugs. Intensive chemotherapy helps to recover and enter stable remission.
Carrying out a chemotherapy procedure
In the first stage of treatment, prescribed drugs indiscriminately kill healthy and cancer cells. Side effects develop:
- Nausea;
- Vomit;
- Lethargy;
- Ulcerative lesions of the oral cavity;
- Nasal bleeding;
- The patient's body is susceptible to dangerous infections.
At the second stage, several courses of cytostatics are prescribed. To destroy cancer, taking a high dose of cytosine arabinoside is important. The drug prevents the creation of particles that carry hereditary information. In case of liver and kidney failure or bone marrow suppression, taking the drug is prohibited.
Idarubicin is prescribed to suppress bone marrow functions and fight tumor cells.
Mitoxantrone suppresses the immune system and destroys tumors.
To achieve maximum efficiency, protocols with three blocks of post-remission chemistry are used.
The prognosis for life with chemotherapy improves significantly.
If the organs of the central nervous system are affected, radiation therapy is recommended. Ionizing radiation reacts with abnormal cells, disrupts their structure and provokes death.
There are stories among people about healing blood cancer with the help of traditional medicine. However, no method or drug has shown 100% effectiveness. By refusing medical intervention, the patient allows leukemia to rapidly develop and disrupt the functioning of vital organs! Treatment can only be carried out by a qualified oncologist after a thorough diagnosis. Unconventional methods usually only worsen the course of the disease.
Full recovery occurs after a bone marrow transplant. The method has nuances and consequences:
- Before the operation begins (infusion of donor material through a catheter installed in the artery), the patient's bone marrow is destroyed using loading doses of chemotherapy.
- In the absence of immunity, any infections and diseases, for example, acute respiratory infections or a scratch, can lead to death.
- The transplanted material may not interact with the patient’s body:
- In the first case, the human body perceives foreign bone marrow as foreign and rejects it. The work of all organs is disrupted. Immune cells kill everything in their path. However, this completely destroys cancer cells without the opportunity to develop again. Immunosuppressive therapy helps to establish a normal hematopoietic process.
- The patient's body rejects the injected stem cells. Immunity is not formed. The production of blood cells does not begin.
- When the biomaterial is introduced, an allergy or anaphylactic shock develops.
- Half of patients die in the first month after surgery.
Bone marrow transplant
Suitable bone marrow is difficult to obtain. The best donors are identical twins and siblings. Parents' material is very rarely suitable.
Stem cells can be taken from the patient himself during a period of remission or from a stranger.
Adequacy of chemotherapy
This factor is not included in foreign clinical recommendations; unfortunately, it is relevant exclusively for Russia. Even correctly prescribed medications may turn out to be less effective than necessary if the calculated doses of the medication are reduced, the intervals between courses are not observed, and similar “external” factors. In addition, belonging to one or another risk group in adults determines the need for bone marrow transplantation, and if a cytogenetic study has not been carried out, it is impossible to classify the patient into one of the three groups. Russian clinical guidelines suggest focusing on clinical signs as factors of unfavorable prognosis:
- age over 40 years;
- blood leukocytes > 100 x 109/l;
- presence of extramedullary lesions;
- remission did not occur after the first course of chemotherapy;
- secondary AML (occurred after a course of chemotherapy for another malignancy);
Treatment and prognosis: adults
Factors influencing the prognosis in adult patients can be divided into 3 groups:
- Individual characteristics of the body and health status;
- Biological characteristics of the leukemic clone;
- Correct selection of treatment method.
Prevention of increasing the number of normoblasts in the blood
To prevent an increase in the number of normoblasts, it is necessary to take preventive measures aimed at preventing the formation of anemia and acute forms of leukemia. To avoid the occurrence of these pathologies, it is recommended to avoid radioactive radiation, inhalation of toxic chemicals, and uncontrolled use of medications.
Medical workers insist that if an increased number of normoblasts is detected in the blood, it is imperative to contact the clinic. Only identifying an accurate diagnosis and timely initiation of therapy will ensure a full recovery and rapid restoration of all body functions.
It is important to understand that the detection of even a small number of normoblasts in a blood test is already a sign of pathology that requires immediate treatment.