Fungi are often a common part of the microflora of human skin and mucous membranes.
For quite a long time, the mycelium and bodies of yeast-like fungi can exist in symbiosis with their host.
Without manifesting itself in any way and without causing inflammatory changes or discomfort.
However, under a number of circumstances, the dynamic balance of the biocenosis may be disrupted.
Conditions are created that are as comfortable as possible for the non-competitive flourishing of fungi, their active growth and reproduction.
Loss of the status quo by the mucous membrane invariably leads to its pathological modifications or even restructuring, which are clinically manifested by at least discomfort.
Mushroom time or what is yeast in a smear
Yeast-like representatives of the genera Candida albicans and Candida tropicalis belong to imperfect fungi (actinomycetes).
They feel very comfortable on mucous membranes, including the mucous membranes of the urethra, vagina, cervix, mouth or rectum.
The cells of infectious agents are collected in chains (pseudomycelium), which visually makes the representatives of the genus similar to yeast.
Blastospore cells are located on the constrictions of the pseudomycelium.
The first contact with candida occurs in a person in infancy.
Adults receive them through household and sexual contact, as well as from food without heat treatment.
The fact that the fungus begins to manifest its properties as an inflammatory agent is facilitated by the presence of many factors.
- The ability to remain on the surface of epithelial cells, showing affinity for various cellular substances and structures, while avoiding immune aggression from the human body.
- Tendency to mild antigenic and morphological variability. Fungi can exist not only in the chain form of pseudomycelium, but also imitate mold fungi. This variability makes it easier for candida to adapt to different temperature, humidity, and acid conditions, and improves their survival even under the pressure of external circumstances.
- Fungi quickly show resistance to fungicidal drugs or learn to quickly eliminate them. This makes it difficult to treat chronic candidiasis.
What is a fungal infection
Elements of a pathological fungus are entire colonies of parasitic species, which consist of approximately 55,000 varieties. The presence of mycelium of a pathogenic fungus in humans provokes many unpleasant factors. When any type of pathogenic fungus enters the body, the following troubles may occur:
- immune resistance is significantly reduced,
- dangerous diseases recur,
- associated inflammatory processes occur,
- the quality of general well-being drops significantly.
The reason for this is the fact that, multiplying and living inside the host, the fungus is parasitic and feeds on the vital forces of a person.
This consumption is due to the fact that mushrooms, for active reproductive life, need mineral and organic substances that make up the cells of the human body.
Pathogens, multiplying, absorb more and more nutrients, and the functional system of human life weakens.
Yeast in a smear: variations in lesions
If we consider only lesions of the mucous membranes, then today candidiasis of the oral cavity, vagina, its vestibule, cervix, urethra, and rectum are known.
In men, candidal urethritis is often combined with balanoposthitis (damage to the leaves of the foreskin and glans penis).
What is needed for opportunistic fungi to exhibit the properties of pathogens?
Some weakening of the immune defense of the body of their owner and the creation of the most comfortable conditions for the life of fungi.
Owner factors:
- A decrease in general and local immunity in chronic pathologies (diabetes mellitus, tuberculosis, oncology), burn and radiation sickness, frequent and uncontrolled use of cytostatics, glucocorticoids, fasting, protein-free diets, aplastic anemia are powerful provoking factors on the part of humans. Yeast in a smear in diabetes and HIV is most often found.
- Pregnancy, part of the menstrual cycle before and during bleeding (due to a decrease in the anti-inflammatory activity of progestins), and the menopause period can be considered special cases of a decrease in the immune defense in women.
- Change in the acidity of the mucous membrane in the direction of its growth. In healthy women, genital candidiasis develops more often than in men due to the high acidity of the vagina.
- Anaerobic conditions, increased sweating, tight or uncomfortable synthetic underwear are circumstances that improve the survival and reproduction of fungi.
Reasons for appearance
Before starting to restore the natural flora of the vagina in women, it is important to establish the cause of the development of the pathology. The Candida fungus begins to actively multiply under the influence of the following factors:
- diabetes;
- weak immunity;
- use of antibiotics based on microorganisms;
- tuberculosis;
- hormonal imbalance (the level of estrogen in the body in women decreases);
- neglect of hygiene rules;
- synthetic underwear;
- inflammatory diseases caused by infection;
- use of oral contraceptives.
- Canadian men's haircut (PHOTO)
- Leukopenia - what it is and its causes. Signs and symptoms of leukopenia in children and adults
- Chicken liver fried with onions in sour cream: recipes
Comfortable environment for yeast-like fungi
Fungi of the genus Candida will be able to carry out their life activities most successfully when they have no one to compete with for their habitat.
It is worth conducting a course, or better yet several, aggressive antibiotic therapy.
Or abuse antiseptics for intimate hygiene.
And the entire protective microbial association, to which we have become accustomed as a constant companion of our lives, dies or is washed away.
As a result, you can easily detect yeast in a smear from the mucous membranes or see the clinic of candidiasis.
In women, the vagina is populated by lactobacilli, which protect the mucous membrane, but do not prevent the growth of fungi.
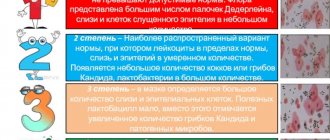
Yeast in a smear in women is detected at 3-4 degrees of purity of the vaginal flora.
This does not mean that aggressive sanitation of the genital tract is immediately required, but it does indicate an imbalance in the bacterial balance.
Detection during pregnancy
The growth of yeast fungi provokes hormonal imbalance. Thrush is one of the very first symptoms of successful conception. Unpleasant symptoms may disappear on their own or require special treatment.
Candidiasis in pregnant women can develop in any trimester, but its most dangerous presence is in the last months. Severe candidiasis can cause miscarriage, fetal pathology, and infection of the child with candidiasis during passage through the genital tract.
However, you should not panic, especially since during pregnancy there is no need for unnecessary worries. Under the guidance of specialists, the proliferation of painful microflora is stopped, and risks are minimized.
To avoid thrush during pregnancy, it is necessary to pay special attention to hygiene procedures, but not to use special detergents. It is recommended to wash with a solution of potassium permanganate, soda, decoction of calendula, chamomile. Monitor your sleep, rest, and nutrition patterns. Sweets, smoked foods, kvass, beer, coffee, flour products - baked goods provoke the growth of yeast fungi.
Why does yeast appear in a smear in men?
Having contacted a urologist with complaints of urinary disorders (usually itching, pain or frequency), a man receives an examination.
It is aimed at searching for pathogens of the main types of sexually transmitted infections.
For this purpose, at an appointment with a urologist, he undergoes a smear and scraping of the urethral endothelium.
Subjecting smears to microscopy (except for approximate identification of signs of inflammation) today is considered to be of little information, even if they are stained.
It is more reasonable to carry out PCR diagnostics, since with its help it is possible to strictly specifically identify the genetic material of certain pathogens.
Yeast in a smear of men can, in principle, be seen under microscopy, but nucleic acid amplification methods are also relevant for them.
Most often, candidiasis is a clinical manifestation associated not with a fresh infection with fungi, but with the flourishing of an existing population.
Although cases of superinfection or reinfection from sexual partners during any type of sexual contact cannot be ruled out.
Symptoms
There are other reasons why the process of reproduction of candida fungi is activated. Such violations occur as a result of taking antibiotics and douching using chemicals. In addition, the proliferation of fungi is possible due to the use of contraceptives and hormonal drugs.
When yeast cells are detected, treatment should be aimed at suppressing the proliferation of microorganisms. Representatives of the fair sex who suffer from this disease dream of getting rid of such strong unpleasant sensations in a short time. After all, a yeast infection can cause unpleasant itching, burning and a terrible odor. In this case, the discharge is whitish in nature and has a cheesy consistency, and the disease tends to recur. During pregnancy, treatment is especially important, since the presence of a large number of pathogenic yeasts can provoke infection of the fetus.
Are there always complaints when there are mushrooms in a smear?
Quite often there are situations when yeast fungi are found in a smear, but the patient does not make any complaints.
That is, there is no detailed clinical picture of the candidiasis inflammatory process; there are no symptoms of yeast in a smear in men and women.
In such a situation, there is no need to sanitize the body.
You just need to pay attention to the state of the immune system, the nature of nutrition, and the state of the endocrine system.
It is advisable for women to take care of normalizing the vaginal microflora.
How dangerous is the pathogen?
Yeasts are a whole group of microbial agents that are also called Candida spp., that is, candida. The results of a regular coprogram do not indicate the type of candida; the answer looks like “yeast detected.” The variety of this fungal agent is not important for the choice of further treatment tactics and management of the patient.
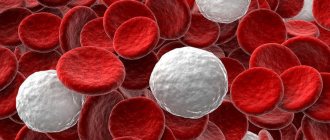
Any type of candida is dangerous if there are a lot of yeast cells. Various toxic substances enter the human blood, the integrity of the intestinal mucosa is disrupted, and the likelihood of the proliferation of other pathogenic microorganisms increases.
As already mentioned, yeast fungi can cause significant harm to the human body only in conditions of immunodeficiency. In this case, severe clinical symptoms and even complications may develop:
- severe gastroenterocolitis with impaired absorption and digestion of food;
- generalization of the process involving the respiratory system;
- development of a fungal septic process.
In the case of fungal sepsis, the prognosis for the patient’s life is unfavorable, since there are pronounced disturbances in all metabolic processes, and antifungal drugs are not always effective.
Under what symptoms can yeast be detected in a smear?
Variants of clinically developed candidiasis may be as follows.
- Vulvovaginitis is most often accompanied by redness, swelling of the vaginal mucosa and its vestibule, single or group whitish deposits, which, as the process becomes more severe, can be replaced by eroded surfaces. A cheesy discharge is characteristic.
- Urethritis is itching, burning during urine discharge, swelling of the external mouth of the urethra, and later an admixture of crumbly whitish discharge or plaque on the urethral sponges.
- Balanoposthitis in men is accompanied by redness, swelling of the head and leaves of the foreskin, accumulation of curd-like deposits in the precipitate sac, erosion and weeping, along with whitish, difficult-to-remove deposits on the head and inner leaf. Pain is observed when touching foci of inflammation.
- Oral candidiasis - single or multiple foci of fungal deposits in the form of white spots, aphthae, swelling, white, difficult to remove plaque on the cheeks and tongue.
- Rectal candidiasis repeats the clinical picture of proctitis of any other etiology - pain, discomfort, burning. With erosive lesions - drops of blood, painful bowel movements.
Symptoms of fungus in the intimate area in women
Women are most susceptible to fungal infections due to hormonal instability at certain periods of life and structural features of the body. The most vulnerable place for pathogen penetration is the groin area and external genitalia. As the infection develops, patients develop the following symptoms:
- Severe itching, especially at night, in the groin area and external genitalia;
- the presence of discharge of a cheesy consistency of a grayish tint;
- the formation of rashes in the form of small bubbles with liquid contents;
- change in skin tone in the affected area;
- the appearance of a pronounced sour odor from the affected areas.
With the development of chronic forms of the disease, symptoms intensify; pain during urination and sexual intercourse may be added to the main symptoms. Due to the structural features of the female reproductive and urinary systems, the infection can easily penetrate into the urine of women, causing diseases of the urinary system. When you detect the first signs of fungus, it is recommended to immediately contact a specialist.
Which doctor can help if you have these symptoms?
For women it is a gynecologist, for men it is a urologist or venereologist.
For lesions of the oropharynx, a dentist; for proctitis, a proctologist.
Since the clinical picture of the described lesions does not have strict specificity, and the presence of a mixed infection cannot be excluded, patients are looking for fungi in a smear or scraping.
If fungi are detected in a smear during microscopy, a polymerase chain reaction may be additionally prescribed.
It is also suitable as an express diagnosis and allows you to more accurately type the type of fungus.
Blood alone is not always suitable for testing.
It is advisable to analyze material collected directly at the site of inflammation.
That is, a sample of scraping of the endothelium of the urethra, vagina, cervical canal, epithelium of the oral cavity or rectum, saliva.
The doctor will also advise you, if yeast is found in the smear, what clarifying tests are needed.
Cultures may be required to determine the sensitivity of pathogens to fungicides.
Analysis of the results obtained
When receiving the results of a smear, the following inclusions may be detected in it:
- Leukocytes;
- The epithelium is flat;
- Slime;
- Lactobacilli;
- Yeasts and yeast-like fungi;
- "key cells";
- Trichomonas;
- Gonococci;
- Escherichia coli;
- Strepto-, staphylo-, enetorococci.
Some of them are normal and constitute the biocenosis in the vagina of an absolutely healthy woman. The presence of certain bacteria, as well as an increased content of opportunistic bacteria, indicates the presence of a particular pathological process. Correct interpretation of a smear for microflora in women is very important at the stage of preliminary diagnosis of the disease.
So, a smear for microflora can have the following letter designations and abbreviations:
- “V” is an abbreviation for vagina, or vagina. Everything that is indicated opposite this column refers to the flora that is in the vagina.
- “C” is short for cervix, or cervix. Accordingly, it reflects the result of the microflora in the cervical canal.
- “U” is the letter designation for the urethra, or urethra. The values next to this letter will be understood by the doctor as indicators of flora in the urethra.
- “L” - a smear on the flora reflects the number of leukocytes.
- "Ep" - squamous epithelium.
- “abs” is a Latin designation that should be interpreted as the absence of something. “gn” is a designation for gonococci, the microorganisms that cause gonorrhea.
- “trich” is an abbreviated name for another pathological bacterium, Trichomonas, which causes trichomoniasis.
| Index | Norm | ||
| V | U | C | |
| Leukocytes (L) | 0-10 | 0-5 | 0-30 |
| Squamous epithelium (ep.) | Up to 5-10 in sight | Up to 5-10 in sight | Up to 5-10 in sight |
| Slime | moderately | Moderate/absent | moderately |
| Yeast, yeast-like fungi, Candida fungi | none | none | none |
| Gonococci | none | none | none |
| Key cells | none | none | none |
| Trichomonas | none | none | none |
| Tlamydia | none | none | none |
How to look for mushroom elements in a smear
The genus Candida is quite variable and the cells of its representatives cannot always be fully seen under microscopy.
But today this is not a problem.
The resulting smear sample can be placed in a test tube, an enzyme can be added to it, and an amplifier can be used.
Various modifications of PCR can detect the genetic material of fungi.
One hundred percent specificity of the technique allows you not to confuse candida with other yeasts or molds.
There is only one thing.
Even if the fungal culture has stopped its rapid growth in the body, the tests will be positive.
Since they will also react to fragments of nucleic chains (at least during the first six months).
Signs and causes of candidiasis
Vaginal candidiasis is one of the most common ailments, manifesting itself clearly in women and very weakly in men. It is worth noting that cases of candidiasis in women and men are almost the same, only men visit medical specialists much less often than women do to a gynecologist.
The main factors of vaginal candidiasis are the symptoms of itching and burning in the vagina, as well as the appearance of a cheesy consistency released from the perineum. Symptoms of itching and burning increase after showering, sexual intercourse and during sleep.
Women, if they detect such symptoms, sooner or later consult a doctor, who makes a diagnosis and prescribes appropriate treatment.
If you do not visit a doctor in a timely manner and self-medicate, then the urinary organs may be involved in the pathological process.
The reasons for the development of candidiasis are varied, but doctors say the most common reason is a weakening of the body’s protective properties. The human body contains a certain number of not only beneficial but also pathogenic pests. Candida fungus is no exception.
When the immune system functions normally, the fungus predominates in a dormant state. As soon as the body’s protective function is weakened, the number of pathogenic microorganisms begins to prevail over beneficial bacteria.
At this moment, the Candida fungus begins to actively develop, leading, accordingly, to the occurrence of the disease. The following factors also influence the development of candidiasis:
- Pathological deviations of the reproductive system organs;
- Pathological deviations of the endocrine system;
- Chronic infectious diseases;
- Metabolic disorders;
- The period of pregnancy, during which the female body is more vulnerable.
It is very difficult to protect yourself from thrush, so if it occurs, you should immediately resort to treatment. Untimely treatment of thrush can contribute to the development of serious complications of the reproductive system, including infertility.
When to treat candida mushrooms in a smear
Identifying symptoms and complaints in patients is a serious reason to consult a doctor and begin treatment for candidiasis.
When choosing therapy, the doctor may favor local medications (for example, for mild oral candidiasis) or resort to systemic antimycotic agents.
Local remedies are gels, ointments, solutions.
- Universal antiseptics like miramistin work well against fungi during rinsing and instillation.
- For local treatment of mucous membranes (vagina, rectum), as well as balanoposthitis, it is possible to use clotrimazole cream, candida bene, miconazole, butoconazole, amphotericin ointment.
- Treatment for yeast in a smear in women is possible with the help of vaginal tablets clotrimazole, suppositories miconazole, livarol. There are also combinations of antibacterial and antimycotic agents in one preparation: Macmiror complex 500 - these are suppositories or cream, Klion-D vaginal tablets, Terzhinan, Polygynax in suppositories.
- For the oral cavity, rinsing with solutions of clotrimazole, biglucoconate, chlorhexidine, and nystatin is suitable. A 1% solution of clotrimazole is also used in applications on sterile napkins. These funds are designed for course use in cases of superficial lesions. Painful sensations are relieved with local anesthetics (1% lidlokin, procaine in applications). To accelerate the healing of erosive defects, Metrogil Denta is used.
Systemic drugs – tablets.
They are used for moderate inflammation or severe pathological changes.
There are two main groups in use today: azoles and antifungal antibiotics.
- Ketoconazole inhibits the process of building the cell wall of candida, achieving an increase in its permeability.
- Fluconazole , including in the form of Diflucan and Flucostat, inhibits the enzymatic activity of the pathogen, inhibiting the oxidation and synthesis of fats - triazole. This group also includes itraconazole or orungal and irunin.
- Through the use of tableted clotrimazole, it is possible to disrupt the normal structure of fungal membranes and achieve the breakdown of their nucleic acids.
- Griseofulvin, like amphotericin B , are fungicides from the class of antibiotics.
The drug is selected taking into account the patient’s weight and the characteristics of his allergic history.
The duration of one course of taking tablets is on average one to two weeks.
Often the pathogen eludes the effects of the drug due to its rapid variability and adaptability.
Therefore, chronic candidiasis may require several courses of treatment with an azole or amphotericin.
Treatment of candidiasis with medications
Medicines that destroy yeast-like fungi are listed in the table:
| Systemic action (in tablets) | Local action (candles) | ||
| Drug and analogues | Active substance | Drug and analogues | Active substance |
| "Diflucan" ("Diaflu", "Diflazon", "Flucostat") | Fluconazole | "Pimafucin" | Natamycin |
| "Nizoral" ("Oronazole", "Fungavis") | Ketoconazole | "Terzhinan" ("Polyzhinaks") | Nystatin |
| “Itrazol” (Rumikoz, “Kanditral”) | Itraconazole | "Klion-D" ("Mikogal") | Miconazole |
| "Pimafucin" | Natamycin | “Candide” (“Candibene”, Kanesten”) | Clotrimazole |
| "Nystatin" | Nystatin | "Livarol" ("Mycozoral") | Ketoconazole |
Local medications are used in the early stages of the lesion.
Systemic drugs have a number of side effects. They cause allergic reactions, headaches, and digestive disorders. Their use is contraindicated during pregnancy and the lactation period. Therefore, systemic treatment is advisable only in the chronic stage of the disease. Topical preparations are effective against fungi in the initial stages.
If you do not treat mushrooms in a smear
Simple carriage of a fungal infection, as we have already found out, is not fatal or dangerous until the clinical manifestations of candidal infection of any body system develop.
The only exceptions can be considered patients with HIV, as well as patients in hematology departments at the stage of aplastic changes and inhibition of leukopoiesis.
For these categories of patients, fungi can pose a fatal threat.
Since they may well lead to a generalized infection.
Complications with yeast in a smear can develop in pregnant women, for whom sanitization of the birth canal is mandatory before delivery.
Otherwise, the fetus may suffer.
Severe forms of genital lesions in women are fraught with ascending infection, the development of cystitis, endometritis, but only in cases of errors in immunity.
For men, prolonged fungal balanoposthitis is fraught with phimosis.
Urethritis can become the primary source of prostatitis, epididymitis, orchitis or cystitis.
Also, other types of infections (viral, bacterial) can be associated with fungi.
Oral candidiasis can lead to persistent problems with chewing and speaking.
Candidal proctitis can spread to proctosigmoiditis or lead to paraproctitis.
In general, the presence of any signs or suspicions of a fungal infection should lead a person to a doctor in order to thoroughly search for the causes of deviations and competently eliminate them.
Treatment of yeast fungus in pregnant women
Treatment of fungus during pregnancy has its own characteristics. In most pictures, doctors prescribe medications with local effects - suppositories and ointments, which are allowed during pregnancy.
It is not recommended to engage in self-treatment, as this is fraught with various complications. Even the most harmless medications should be prescribed by a doctor, taking into account the characteristics of the clinical picture, trimester, and concomitant diseases.
Treatment regimen during pregnancy:
- Use of suppositories Pimafucin, Terzhinan;
- Douching with chamomile decoction;
- Careful hygiene;
- Diet food.
Sweet foods should be excluded from the menu, as they create a favorable environment for fungal activity. The menu includes fermented milk products, sauerkraut, pickled cucumbers, fish, and walnuts.
Mushrooms in a smear: preventive measures
It is always easier to take care of your own safety than to treat a full-blown inflammatory process.
- To reduce the risk of sexual candidiasis, you should use barrier contraception (condoms, latex wipes).
- Antiseptics should be used wisely and only when indicated.
- Antibiotic therapy should be carried out under the supervision of a physician and as prescribed. For long-term or repeated courses, the doctor may recommend prophylaxis with antifungal drugs.
- To prevent monthly exacerbations of genital candidiasis in women, simultaneous administration of flucanazole or flucostat in doses of 150 mg is recommended.
- For patients using topical inhaled hormones (for example, for asthma or COPD), soda mouth rinses are recommended to avoid fungal inflammation.
- Preventive diagnostic examinations by a urologist and gynecologist twice a year are advisable for all sexually active people.
If you suspect yeast in a smear, contact the author of this article, a venereologist in Moscow with many years of experience.
The danger of yeast inclusions in the analysis
Exceeding the fungus norm can signal a dangerous disease.
If a bacterioscopic analysis of a smear shows an increase in the number of Candida fungi above the norm, then there is a risk of developing dangerous consequences. Yeast in a smear in women is the main sign of thrush.
Thrush is often accompanied by erosion of the cervix, which, in turn, often leads to an obstacle to the successful fusion of sperm and egg - infertility. Long-standing erosions are the most common cause of cancer.
Candidiasis detected in a smear in men leads to balanoposthitis.
Interpretation of smears and test norms
To take a smear from men, a special probe is used, which is inserted into the urethra to a depth of 30-50 mm. Then make light rotational movements with the probe and remove it. The material for research is placed on glass. After receiving the results, the doctor interprets them.
If we talk about Candida in a smear, the norm for this indicator is as follows:
- normally, Candida albicans fungi should not exceed 10³ CFU;
- if the number of colony-forming units is 10³, then they speak of a slight excess in the number of fungi;
- if Candida fungi are detected, the norm in the smear is exceeded by up to 10⁴, then this indicates a moderate excess of the normal value;
- a value of 10⁵ or more indicates a large number of mushrooms.
The test results also describe the category of sensitivity of fungi to antimycotic agents. These indicators are deciphered as follows:
- H – means the sensitivity of the fungus to the drug;
- DZ - this abbreviation stands for dose-dependent sensitivity;
- R(U) – resistance or resistance of fungi to an antifungal agent.
Important! Different laboratories may have different reference values and a set of indicators in analyses.
Detection of Candida fungi in a smear in single values is a variant of the norm. The diagnosis of urogenital candidiasis is made only when indicators are in the range of 10⁴-10⁵ CFU per milliliter or higher.
Methods for diagnosing HPV types 16 and 18
Have you been fighting thrush for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure thrush by taking it every day.
Papillomavirus infects epithelial cells of the mucous membrane and skin. The main feature of the pathogen is its ability to accelerate the process of reproduction of these cells. Due to the rapid development of medicine, 120 of its species have been identified today. It spreads through direct contact with the skin, through kissing, anal, vaginal, and oral sex. Moreover, each strain of the virus manifests itself differently. Thus, pathogens of types 4, 1 and 2 lead to the appearance of plantar warts, 29, 26, 27 - ordinary neoplasms.
Of the total number of viruses, approximately 30 infect the organs of the genitourinary system. The most dangerous is the papillomavirus with a high percentage of cancer - HPV 16: the diagnosis should not be determined only by the PCR method, since sometimes the tests can be erroneous. This type of pathogen is characterized by the highest ability to provoke cancer of the urethra or cervix. A quantitative test is best used to assess the clinical burden of HPV 16.
But a positive test for the presence of papillomavirus does not mean that cancer is inevitable. The disease actively progresses under the condition of persistent infection - that is, if the human papillomavirus HPV type 16 is detected and again a year later it is detected again.
Negative factors that increase the chances of contracting papillomavirus:
- early sexual life and frequent changes of partners;
- decreased immunity and the presence of infections;
- miscarriages and abortions;
- alcoholism, smoking.
If HPV 16 is positive and a woman has had the virus in her body for a long time in the cervix, her chance of developing cancer is 65 times higher than for those who have not been diagnosed with it. For patients over 30 years of age, these have shown to increase significantly.