The main task of leukocytes is to protect humans from pathogens. Having antibacterial and antiviral effects, they are responsible for strengthening the immune system. Leukocytes in urine during pregnancy, significantly exceeding standard values, indicate progressive inflammation in the woman’s urinary system. To prevent the adverse effects of the disease on the developing fetus, the expectant mother is prescribed medication under the supervision of the attending physician.
Probable reasons for the increase
The presence of chronic inflammatory diseases can often lead to the appearance of a high level of leukocytes in the urine (leukocytosis).
Cystitis, urethritis, pyelonephritis, urolithiasis contribute to the development of this pathological condition. Sometimes, due to decreased immunity, inflammation enters the body in 3 ways:
- ascending;
- hematogenous;
- lymphogenous.
During pregnancy, the most common route is the ascending route. From the lower parts of the urinary system, microorganisms penetrate into the upper parts, disrupting the functioning of the kidneys and ureters.
Infectious agents can penetrate from the genital tract during a long-term fungal infection (candidiasis or thrush).
In addition to these reasons, there are others that are less common:
- presence of a renal cyst;
- systemic lupus erythematosus;
- oncological diseases of the urinary system;
- sexually transmitted diseases;
- inflammation of the female reproductive system.
Why does the rate increase in the 1st trimester?
In the first trimester, an increase in the level of leukocytes may be associated with improper hygiene of the genital organs, inflammation of the uterine appendages (adnexitis), transition to an exacerbation phase - pyelonephritis, cystitis or urethritis.
At the initial stages, this is manifested by a slight or moderate (10-20 in p/z) asymptomatic increase in leukocytes in urine. Reduced immunity, changes in vaginal microflora and hormonal changes can cause the development of inflammation in the bladder tissues.
In the absence of adequate therapy, a persistent increase in leukocytes and a pronounced clinical picture of these diseases develops.
Is it normal to increase white blood cells in urine in the second trimester?
In the second trimester, an increase in white blood cell levels is considered normal. Due to the fact that the fetus grows and increases the load on the mother's body, leukocytosis may develop.
In the second and third trimester, the reasons for the increase may be gestosis. Preeclampsia is a pathological condition in which renal function is impaired. Swelling, increased blood pressure and protein levels, and cramps occur. Preeclampsia develops as a result of hormonal imbalance or the development of an immunological conflict between mother and fetus (due to different Rh factors). This leads to a narrowing of the blood vessels of vital organs (brain, heart, kidneys), impaired circulation in them and thinning of the vascular wall. The result is an increase in vascular permeability, the formation of blood clots and pathological changes in cells.
After eliminating the symptoms of gestosis and adequate therapy, the number of leukocytes in the urine returns to normal.
If elevated before childbirth
In the last trimester, the load on the mother's body increases.
Pregnant women are increasingly susceptible to the development of gestosis and increased levels of leukocytes and proteins in the urine. The doctor diagnoses and prescribes a course of therapy to eliminate the causes of leukocytosis in the urine. Having assessed the condition of the pregnant woman, the obstetrician-gynecologist chooses the route of delivery. If the fetus is at low risk of developing antenatal or postnatal infection, then vaginal delivery is performed. Otherwise (for sexually transmitted diseases, fungal infections) - cesarean section.
Treatment approach
There is no specific treatment regimen for leukocyturia, which is understandable, because each clinical case has its own etiology, gestation period, distinctive features of pregnancy and other nuances. For mild infectious processes, patients are prescribed disinfectant and diuretic natural medicines. These include kidney tea mixtures, chamomile decoction, lingonberry tea, Canephron and other herbal medicines.
If the inflammation occurs in a pronounced form, then treatment is based on antibiotic therapy, for which the doctor individually selects drugs taking into account the type of pathogen and gestation period. Local antibiotic preparations, for example, urethral and bladder instillations with disinfectant solutions, have an excellent therapeutic effect. With this approach to therapy, there is a minimal degree of penetration of the drug into the bloodstream.
Among the most commonly used drugs in the treatment of pregnant women are Clotrimazole and Canephron, Amoxicillin and Monural, Furadonin, etc.
Critical norm: what is the largest number of leukocytes that can be in the urine
The critical norm depends on the stage of pregnancy at which the increase in leukocyte levels occurred. In the first trimester, the level of cells is no more than 5 in the field of view, in the second and third – no more than 10.
There are 3 degrees of leukocytosis:
- insignificant when up to 15 cells in the field of view are detected in the urine;
- moderate, the number of leukocytes varies from 20 to 40;
- high, leukocyte count more than 40.
When leukocytosis is detected, the doctor carefully interviews the expectant mother and collects research data that can help in making an accurate diagnosis so as not to harm the body of the mother and fetus.
How to avoid elevated white blood cells
To prevent the development of leukocyturia during pregnancy, a woman needs to seriously prepare for the prevention of inflammatory diseases.
- It is necessary to regularly undergo laboratory tests of urine and promptly treat inflammatory lesions of the genitourinary system.
- Avoid stress, physical overload, and hypothermia.
- Spend more time outdoors, don’t be nervous and relax.
- If there are suspicious changes in your urine, you should definitely tell your obstetrician-gynecologist about them.
If treatment is undertaken in a timely manner, and the inflammatory process is eliminated at its earliest stages, then the child and mother will not be in any danger.
Symptoms and pathogenesis
With a slight increase in leukocytes, clinical symptoms may be absent. As it progresses, symptoms of the disease present in the mother’s body appear.
Pyelonephritis
This is an inflammation of the renal tubular system, which is caused by bacterial agents. During pregnancy, it occurs due to the fact that the fetus and uterus constantly increase in size and begin to put pressure on nearby organs and blood vessels. When a child pinches the renal arteries, blood flow in them is disrupted, and there is a risk of infection. Kidney changes also occur during pregnancy. They reduce blood pressure, vascular tone, and reduce motor activity. Urine is not completely evacuated into the ureters and bladder. This leads to the accumulation of pathogenic microorganisms in it and the development of leukocytosis.
Due to changes in hormonal levels and an increase in the amount of estrogen, the growth of microflora, in particular E. coli, increases.
Pyelonephritis is diagnosed in women who have already had it, and develops for the first time against the background of gestosis.
Symptoms:
- nagging pain in the lumbar region;
- increased body temperature;
- pain when urinating;
- general weakness;
- nausea;
- vomit.
Cystitis
This is an inflammation of the walls of the bladder, caused by hypothermia or the presence of microbes in the body. This is due to long-existing chronic foci of infections - carious teeth, inflammation of the tonsils, chronic diseases of the urinary system, which were in remission.
With cystitis, the following symptoms develop in pregnant women:
- difficulty urinating, combined with itching and burning, after which pain occurs;
- the amount of urine excreted is reduced, there is a feeling of insufficient emptying of the bladder;
- general weakness;
- hyperthermia;
- severe pain in the lower abdomen;
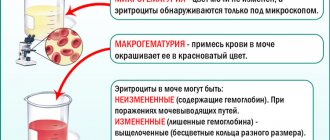
- change in color and density of urine;
- presence of blood streaks in the urine.
Urethritis
This is an inflammation of the urethra that occurs when microorganisms penetrate from the upper parts of the urinary tract or from the genitals.
For urethritis:
- frequent urination with pain that does not disappear after emptying the bladder,
- copious discharge from the urethra.
Diseases of the reproductive system
Kinds:
- chlamydia;
- gonorrhea;
- syphilis;
- HIV and others.
In the presence of infectious and inflammatory diseases of the reproductive system, a pregnant woman is found to have:
- itching and burning in the external genital area,
- copious vaginal discharge with an unpleasant odor,
- the presence of rashes in the genital area,
- pain in the lower abdomen and genitals.
Systemic lupus erythematosus (SLE)
SLE is a pathology of connective tissue that occurs during the formation of an immune conflict (antibodies arise to one’s own cells).
Systemic lupus erythematosus is not transmitted from mother to child. The child has placenta-transmitted lupus factor, which disappears by 5-6 months. The growth and development of the newborn is normal.
The disease manifests itself:
- joint pain;
- rashes on the face;
- hair loss;
- inflammation of the cardiac membranes - pericardium, myocardium (heart pain, shortness of breath);
- hyperthermia;
- headache;
- kidney damage (increased protein and leukocytes in the urine).
Tumors
They also cause an increase in the level of leukocytes and the development of a severe clinical picture and complications for the fetus.
If the tumor is benign (cyst), then in the first stages there are no symptoms. Over time, general symptoms may occur: pain in various parts of the lower back, difficulty urinating, etc.
For malignant tumors that are hormone-producing, the clinical picture quickly worsens. In addition to pain, short-term fainting and bloody discharge from the urethra and genital tract occur.
What to do if leukocytes are elevated during pregnancy
If leukocytes are elevated, you should first do a repeat urine test to rule out a possible error. If leukocytosis persists after 2-3 times, and other signs of pathology are also present, additional methods are used to make a diagnosis.
Additional examinations
To clarify the pathology of the urinary tract, the following is carried out:
- urine analysis according to Nechiporenko;
- three-glass sample;
- Ultrasound of the kidneys and bladder;
- vaginal smear;
- general and biochemical blood tests;
- ultrasound diagnostics of the abdominal organs;
- tests for specific infections.
In some cases, you may need to consult a therapist, allergist, surgeon, nephrologist, and undergo additional tests and instrumental studies.
What treatment is needed
Treatment is aimed at eliminating the cause or reducing the provoking factor of the pathological condition:
- Antibiotics are used for inflammation of the kidneys and bladder. They are prescribed only by a doctor.
- To overcome stagnation of urine, it is recommended to drink fluid (1.5 liters or more per day), if there is no tendency to edema.
- It is useful to drink rosehip decoction, which saturates the body with vitamins and has a diuretic effect.
- Mild inflammation can be relieved by washing the genitals with chamomile infusion. If the cause is a fungus (thrush), then soda baths will help.
- Preeclampsia, glomerulonephritis, and neoplasms require constant hospitalization. In complex, severe and life-threatening conditions, artificial termination of pregnancy may be required.
The appearance of leukocytes in a pregnant woman's urine requires special attention. Leukocyturia can be a sign of a serious illness, so the analysis should be repeated and additional research done.
Complications for the fetus
An increase in the level of leukocytes is fraught with the development of complications for both the fetus and the mother.
Fetal complications include:
- spontaneous miscarriage;
- intrauterine infection, which provokes the development of hypoxia and fetal death;
- amniotic fluid embolism;
- growth retardation and impaired fetal development;
- formation of placental blood clots;
- change in the position of the fetus (from an oblique size to a transverse one, which makes it difficult to move along the birth canal with the risk of developing birth tumors and injuries);
- high risk of infectious pathologies in the fetus when moving through the birth canal (conjunctivitis, pneumonia).
From the mother:
- preeclampsia;
- eclampsia;
- premature placental abruption;
- bleeding.
Why is leukocyturia dangerous?
If an increased number of leukocytes is observed against the background of an inflammatory process in the kidneys, treatment should be carried out immediately, otherwise the consequences can be very dire. Why is delay dangerous in this situation? Leukocyturia, which is a sign of nephritis (inflammation of the kidneys) in pregnant women, is fraught with the following:
- development of late toxicosis - one of the causes of gestosis, and fetal death;
- the inflammatory process can lead to gangrene of the bladder, followed by rupture of its wall and the entry of contents into the peritoneum, and therefore to the occurrence of peritonitis;
- chronic inflammatory processes often lead to the formation of stones in the kidneys and bladder, and severe attacks of pain sometimes force surgery even during pregnancy;
- hypertension causes deterioration in the nutrition of the fetus, and leads to its death, as well as abnormalities of cerebral and coronary circulation in the mother;
- eclampsia leads to convulsive syndrome, the baby in the womb does not receive enough oxygen and nutrition, which increases the likelihood of premature birth or congenital anomalies.
How is differential diagnosis and treatment carried out?
Differential diagnosis is carried out in a hospital setting after laboratory and instrumental research methods.
Not only urine but also blood is taken from pregnant women for testing. A general blood and urine test is performed, which reveals an increased level of leukocytes, indicating an inflammatory process.
A general blood test also determines the presence of young and mature forms of leukocytes, which indicate an oncological process.
In addition, it is necessary to do microbiological inoculation on nutrient media in order to identify a possible pathogen.
In order not to expose the fetus to a high level of X-rays, only ultrasound diagnostics are prescribed, since it does not harm the body of the mother and fetus. Using ultrasound, the presence of a pathological process in the organs of the urinary system is checked (inflammation of the walls of the organs, the presence of stones, tumors, etc.).
After confirmation of the diagnosis, a combination treatment is carried out that does not interfere with the development of the fetus and does not provoke the formation of pathological conditions for its existence. The doctor draws up a prescription based on the duration of pregnancy, the clinical picture and research data.
What is prescribed
After confirmation of the inflammatory process in the mother's body, antibacterial therapy is prescribed.
The most effective and safe drugs are Monural and Amoxiclav. In addition, uroseptics are prescribed - drugs that suppress microflora in the urinary tract - “Canephron”, “Furadonin”.
To combat fungal infections, vaginal suppositories are prescribed - Nystatin, Flucanazole.
A course of treatment
The duration of treatment is prescribed individually by the doctor. On average, the course of antibacterial therapy is 7-12 days, and antifungal therapy is 5-10 days.
Until the pathogen is completely destroyed (confirmed by tests), it is prohibited to stop taking medications on your own.
Additional examination
Leukocytes in the urine during pregnancy, significantly higher than normal, indicate serious pathologies of the urinary system.
To make a diagnosis, the obstetrician-gynecologist prescribes a number of additional tests, including:
- urine test according to Nechiporenko - to determine the functionality of the urinary organs, quantitative measurement of the content of leukocytes in 1 ml of urine;
- Urine analysis according to Zimnitsky - to assess the ability of the kidneys to concentrate and excrete urine, shows the daily volume of urine produced;
- bacteriological culture - in order to identify the causative agent of the disease and determine the antibiotic to combat it;
- Ultrasound of the kidneys - for visual diagnosis of the condition of the organ.
Expert opinion
Elena Ivanova
Practicing obstetrician-gynecologist. More than 20 years of experience. Experience working abroad.
Ask a Question
In extreme cases, chromocystoscopy and contrast-enhanced x-rays are performed. These procedures can harm the baby. Often, the obstetrician-gynecologist sends the woman for a consultation with a nephrologist.
Forecast
With timely diagnosis and therapy, a favorable prognosis is characteristic. It is necessary to complete the full course of treatment even after the symptoms disappear, to prevent recurrence of the pathology.
Elevated white blood cells in the urine are not a reason to panic. Sometimes they can be triggered by heavy physical exertion. If leukocytosis is detected in the urine of pregnant women, it is not necessary to undergo additional research methods to identify the cause of the increase in leukocytes. After this, the doctor will prescribe adequate therapy so as not to harm the body of the mother and fetus. Compliance with all doctor’s instructions will contribute to a favorable course of labor.
Basic rules for collecting urine for analysis
During pregnancy, expectant mothers are prescribed a urine test quite often. In the 1st trimester - once a month, in the 2nd trimester - approximately every 2 weeks, and in the third - almost every week. What points need to be taken into account so that the research result is reliable and does not have to be repeated?
Leukocytes and bacteria in urine during pregnancy
These include the following:
- 1–2 days before the analysis, you should reduce the amount of protein products in the diet, as well as citrus fruits, fruits and berries;
- discuss with your obstetrician-gynecologist the possibility of continuing to take medications if the woman is currently undergoing treatment;
- prepare a container for collecting urine (rinse and sterilize the existing one or purchase a special container at the pharmacy);
- in the morning, immediately before collecting biomaterial, the genitals should be toileted;
- Before you start urinating, you must insert a tampon into the vagina - this will reduce the risk of epithelium or microflora getting into the urine sample.
Collection is carried out according to the following principle: the first portion of urine is flushed into the toilet, the next - into the container, and the rest - into the toilet. The collected sample should be delivered to the laboratory as quickly as possible, since if the urine stands at room temperature for more than two hours, its physical and chemical properties may change and the analysis will not be reliable.
When storing the sample in a refrigerator at a temperature of 4–6º, this time increases to 6–8 hours. It is optimal to take urine tests in special containers, which, along with compliance with all preparation rules, guarantees the receipt of reliable and informative research materials.