From birth, the baby undergoes a bunch of various tests to check the condition of the baby and identify possible health problems in time.
One indicator that is measured daily is the level of bilirubin.
A slight excess of bilirubin in the first 23 days after birth is considered a physiological phenomenon, characteristic of 80% of babies. If the indicators are much higher than the established values, the child should be under constant supervision, as the consequences can be very serious.
Classification
A blood test evaluates three types of enzyme:
- indirect bilirubin;
- straight;
- general.
Direct type bilirubin is non-toxic and is excreted naturally. Features of indirect are its combination with fats, toxicity and ability to accumulate in tissues. This type of bilirubin is excreted only after it is converted by a gastric enzyme into a direct enzyme.
Reasons for low level
In response to the obstetrician’s words about the presence of jaundice, many mothers ask in bewilderment: “Where could it come from if everything was in order during the prenatal examination?” This pathological deviation is observed in a newborn if hemoglobin is destroyed in his body, which is also accompanied by a characteristic change in skin color to an olive (yellowish) tint.
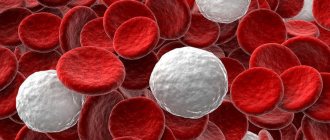
The fact is that the composition of hemoglobin in a fetus and a newborn baby is slightly different. And during the breakdown of fetal hemoglobin after the birth of a child, a side effect may occur in the form of a secreted pigment. This substance is called bilirubin (direct and indirect). In newborns, it is formed when the process of decomposition of red blood cells that have outlived their “lifetime” begins in the blood. The pigment bilirubin, which exceeds the permissible level, can turn the skin of a baby olive green.
We can notice the decomposition product of hemoglobin, bilirubin, on the body in the form of dirty yellow halos that form after 7-9 days around the injury. In newborns, physiological jaundice manifests itself in 80% of cases and can go away on its own in 7-14 days without causing harm to health.
Usually the pigment is eliminated from the body on its own. However, which way bilirubin is released will depend on the type of hemoglobin breakdown products. There are two types of pigments:
- direct bilirubin - dissolved by enzymes produced by the liver and excreted from the body in urine and feces;
- indirect - is not able to dissolve in water, therefore it is excreted through the bloodstream into the liver together with the protein albumin, where it turns into direct. Only after this will it be excreted through the gallbladder.
- 205 mmol/l – in children born on time;
- 171 mmol/l – in prematurely born (premature) infants.
A month later, these indicators will also be different. So, in a baby who is one month old, the level of bilirubin in his blood should vary between 8.5 and 20.5 mmol/l. If the norm exceeds the permissible limit (256 and 172 mmol/l for full-term and premature babies, respectively), you will need to take a blood test to identify the causes of increased bilirubin and eliminate them.
Important tests
The very first test for newborns is a blood test. Immediately after cutting the umbilical cord, blood is taken from it for a general analysis. Thus, not only the blood type is determined, but also the level of various substances in it (including bilirubin in a newborn).
Based on the results of the baby's blood test, bilirubin in newborns should be detected:
- general – level of total pigment concentration (direct indirect);
- direct (the norm for the indicator is no more than 25%);
- indirect (more than 75%).
If a newborn's blood test shows values exceeding the limit of 256 mmol/L (171 mmol/L), a doctor may diagnose jaundice. At the same time, such a condition, when the level of direct or indirect bilirubin is more than permissible, can have three forms of manifestation.
There are cases when there is an excess level of bilirubin in a newborn baby seven days old. This phenomenon most often occurs in breastfed children, who gain weight very quickly. The fact is that a food product such as breast milk contains a high level of estrogen, which prevents the natural excretion of bilirubin from the tiny body of a newborn.
- incompatibility of blood groups between a new mother and her baby;
- Rh conflict in a pregnant woman during the period of gestation;
- an infectious disease affecting the child's liver, or liver dysfunction;
- destruction of red blood cells that occurs against the background of the genetic characteristics of the body;
- mechanical jaundice;
- intestinal obstruction in a newborn;
- premature birth;
- stimulation of active labor with special substances;
- hormonal imbalances in a newborn;
- minor hemorrhages in the baby.
Pathological jaundice lasting 2.5-3 weeks with discoloration of feces and intense coloration of urine indicates serious problems in the body associated with the biliary tract.
If we talk about how long jaundice can last, it is also important to clarify what its danger is. If a blood test of a newborn baby shows a high level of bilirubin, this can be fraught with a negative effect on the nervous system.
In this case, the excess hemoglobin breakdown product, without being completely blocked by proteins in the blood, is able to penetrate the nervous system.
As a result, against the background of extraneous interference with bilirubin, bilirubin encephalopathy can develop, the symptoms of which can make themselves felt already in the first days after the birth of the child (enlarged spleen, large liver, convulsions, drowsiness, etc.).
If the pathology is not detected in a timely manner and jaundice in a newborn is not treated, then by 5-6 months the pediatrician can diagnose developmental disorders in the child. These may include hearing problems, vision loss, or paralysis. A table of acceptable values by month (see below) will help you monitor the level of pigment in the baby’s blood in the future.
As you can see, a newborn blood test to determine the level of bilirubin in it is mandatory for all children. Its results make it possible to assess whether bilirubin levels (total, direct and indirect) do not exceed the permissible limit in order to eliminate deviations in time.
In every newborn, the level of bilirubin in the blood increases in the first days of life. Normally, by the month, bilirubin decreases significantly and subsequently does not increase to such high levels. If a child experiences severe yellowing that does not go away and intensifies, then it is imperative to go to the hospital.
What is bilirubin
Bilirubin is formed during the breakdown of red blood cells from hemoglobin. Since blood cells break down in the spleen, bilirubin is mainly formed in this organ.
The spleen produces only unbound bilirubin, which is dangerous to the body and is a strong poison.
Jaundice occurs when the liver cannot cope with the load and converts indirect bilirubin more slowly than it is formed. Bound bilirubin can also be excreted through the intestines.
In newborns, physiological or transient jaundice usually occurs, which appears as a result of the body’s adaptation to new conditions.
Transient jaundice occurs in 60-70% of cases and often does not require medical intervention. Pathological jaundice is much more dangerous and can lead to serious disturbances in the functioning of the central nervous system and brain.
An increase in bilirubin to a critical level can lead to the death of the baby.
Bilirubin standards for a newborn are up to 34 units per liter of blood. On the second day, the levels increase and can reach 150 µmol/liter.
On the third day, the maximum value is 250 µmol/liter. After the third day of life, the child's bilirubin begins to gradually decrease. By the month it should be 9-20.5 µmol/liter.
All indicators are checked only using a blood test.
In addition to bilirubin, doctors also look at other blood indicators that may indicate problems with the body. In some cases, the first signs of jaundice may appear only on days 4-7, which is due to the large birth weight and good appetite.
If the child has no changes in the color of feces and urine, he is calm, and his indicators are within normal limits, then they try not to prescribe medications and additional procedures to newborns.
One of the important factors for the successful removal of bound bilirubin is regular bowel movements and urination. Factors that cause transient jaundice include:
- Premature or difficult labor;
- The mother has chronic diseases, including diabetes, diseases of the hematopoietic system;
- Rhesus conflict;
- Stimulation of labor;
- Emergency delivery by caesarean section;
- Lack of breastfeeding;
- Anomalies in the development of organs and systems;
- Sudden weight loss after birth;
- Oxygen starvation of a child.
For children who were born before 34 weeks of pregnancy, critical bilirubin levels are half the normal level than for full-term children.
An increase in bilirubin can be initially detected using a special device that photometrically determines the concentration of the substance in the blood.
If suspicions arise, doctors conduct more detailed studies and take blood for analysis.
In order not to be afraid of these words, it is necessary to understand what role bilirubin plays in newborns and what amount of this substance is safe for the baby.
Bilirubin is a pigment, a high concentration of which in the body can become poisonous to the nervous system. This substance is the result of the breakdown of red blood cells.
Hemoglobin is released from obsolete red blood cells, which immediately becomes toxic. The immune system begins to “attack the enemy” and destroys hemoglobin, releasing hemes - compounds containing iron. Under the influence of enzymes, hemes are transformed into bilirubin.
It is necessary to distinguish between direct and indirect bilirubin. Direct bilirubin is excreted in feces and urine, while indirect bilirubin first forms a compound with albumin and is transported to the liver, where it ferments and becomes direct bilirubin, which easily leaves the body.
Bilirubin in the blood of a newborn is always elevated. The fact is that oxygen in the body of an unborn child is carried by red blood cells saturated with fetal hemoglobin. After childbirth, it loses its functions and is destroyed, leaving behind a breakdown product - bilirubin.
In the maternity hospital, the child's blood is taken several times to determine the level of this pigment. Increased bilirubin in newborns indicates the occurrence of jaundice, and thus doctors monitor its progress.
Jaundice with high bilirubin is dangerous both in itself and may indicate the development of some pathological condition in the baby.
- Immediately after the baby's first cry, doctors measure the level of pigment in the umbilical cord blood. Two days later, the full-term baby is tested again.
- For premature babies, the amount of pigment in the blood is checked a day after birth, and it is monitored every 24 hours.
- For children at risk (difficult pregnancy, difficult childbirth, severe yellowness of the sclera and skin), blood is taken from the vein on the head.
What is bilirubin
Symptoms of pathological jaundice in newborns:
- long period of manifestation (longer than 14 days);
- occurs both immediately after birth and some time later, but always in the first 28 days of the child’s life;
- bilirubin values change abruptly;
- the skin changes pigmentation on all parts of the body, the limbs are especially intensely colored;
- waste products change color (light feces and dark urine);
- changes in liver function;
- hyperexcitation gives way to lethargy and apathy.
The danger of such jaundice is that with high levels of bilirubin in the blood, the enzyme can penetrate the child’s nervous system. And for her, the yellow pigment is real poison.
Then, already on the first day of life, the child develops a serious disease called Bilirubin encephalopathy.
Its symptoms:
- low pressure;
- limb spasms;
- lack of appetite;
- drowsiness and weakness;
- jaundice weakens, after a while it increases again;
- clearly expressed.
If the necessary measures are not taken in time, then by six months the child may experience hearing loss, delayed development, and even paralysis.
Mom should also be concerned if jaundice lasts more than three weeks, and the urine turns dark, and the stool, on the contrary. Discolored. This is a sign of bile duct disease.
Norms of values
Normal bilirubin levels in infants may fluctuate. At birth, the limit is from 51 to 60 µmol/l, but hemoglobin continues to break down. As a result, tests may show inflated values already on the 3rd day of a baby’s life. Further indicators decrease.
Below is a table by day reflecting the rate of bilirubin.
| Age | Norm for full-term babies | Normal for premature babies |
| 24 hours | up to 85 | up to 97 |
| 36 hours | up to 150 | up to 120 |
| 48 hours | up to 180 | up to 150 |
| 3-5 days | up to 256 | up to 171 |
| 6-7 days | up to 145 | up to 145 |
| 8-9 days | up to 110 | up to 97 |
| 10-11 days | up to 80 | up to 50 |
| 12-13 days | up to 45 | up to 35 |
| more than 14 days | up to 20.5 | before 18 |
After a week of life, the high concentration of the enzyme decreases. The level of the substance stabilizes by 21 days. A baby's pigment levels should be constant at one month. The monthly table shows only the threshold values. When an increase in bilirubin is observed at 2-3 months of life, immediate therapeutic intervention is required.
| Age (month) | General indicator (µmol/l) |
| 1 month | 11,1 |
| Over a month old | 8.5 - 20.5 (bilirubin can fluctuate from 9 to 21 µmol/l even by two months of age) |
Premature babies are diagnosed with jaundice in almost 80 percent of cases. Their enzyme concentration, unlike that of healthy children, will be lower. In addition, bilirubin in this case is most often indirect.
Treatment methods
It is necessary to start treatment only after the type of disease has been established. Physiological jaundice usually goes away on its own. If after the third week your bilirubin levels have not returned to normal, you should take the test again. To quickly eliminate the pathology, there is a need for frequent breastfeeding (10-12 times a day).
If breastfeeding is impossible or the volume of milk is insufficient, injections of glucose, ascorbic acid, and B vitamins are prescribed. Phenobarbital is usually used as a medication.
An effective modern method of therapy is phototherapy, a procedure that involves the breakdown of indirect bilirubin under the influence of ultraviolet rays. It has a number of side effects: allergies, burns, so it is not suitable for everyone. The sooner treatment begins, the greater the likelihood of avoiding complications. Physiological jaundice can sometimes develop into pathological jaundice, so the newborn is under constant medical supervision.
How to improve a low score
The skin and mucous surfaces (sclera of the eyes, surface of the tongue, etc.) may acquire a yellowish tint in the first days of a baby’s life. Such a manifestation is quite normal.
But this does not mean that the listed signs can be left to chance. If you do not pay attention to jaundice in newborns, it can become chronic and cause complications.
Bilirubin is a greenish-yellow bile pigment. It is formed as a result of the breakdown of outdated fetal blood cells (erythrocytes), which after birth become useless for the baby.
Since the baby's liver is immature, it is not able to cope with the full load and process the entire volume of dead blood cells.
Bilirubin present in the baby’s blood can be of 2 types:
- direct (connected). It is excreted from the body in feces and urine. This is a water-soluble substance that is formed in the liver and leaves the body without problems;
- indirect (free). It combines with albumin and enters the liver, after which it is processed by the organ and excreted from the body along with decay products (urine and feces) in the same way as direct. It is insoluble in water. When this enzyme gets inside cells, cellular mechanisms are disrupted, resulting in the toxic effect of free bilirubin on the body.
Experts also use the concept of total bilirubin. This is the sum of intermediate products (bound and free) in the blood serum.
When it comes to monitoring the situation in the first days of a baby’s life, experts pay special attention to indirect (free) bilirubin, which is the cause of the development of the well-known jaundice in newborns.
The norm and limit of bilirubin in newborns are generally accepted norms.
By comparing the data obtained after blood sampling with the normal value, doctors can make an objective conclusion about the child’s health status and take appropriate measures to normalize the indicators.
The norm for babies born at term is 256 µmol/l. If the baby was born prematurely, a figure of 171 µmol/l is considered normal.
At the same time, the skin, sclera of the eyes and mucous membranes may still have a yellowish tint, without posing a danger to the life and health of the baby. As a rule, such pigmentation goes away on its own within 7 to 10 days after the baby is born.
The critical indicator for children born at term is considered to be 324 µmol/l, and for premature babies – 150-250 µmol/l. With such results, specialists usually insist on drug treatment. And their fears and demands are completely justified. Lack of treatment can provoke the development of serious complications or chronic pathologies.
Over time, the amount of fetal hemoglobin in the body decreases. The liver gradually processes dead blood cells, as a result of which the skin and mucous membranes acquire a normal shade, and the condition of the baby is normalized.
You can get complete information about acceptable indicators by looking at the table data.
| Baby's age | Bilirubin, µmol/l |
| 12-24 hours | up to 85 |
| 36 hours | up to 150 |
| 48 hours | up to 180 |
| 3 – 5 days | up to 225 |
| 6 – 7 days | up to 145 |
| 8 – 9 days | up to 110 |
| 10 – 11 days | up to 80 |
| 12 – 13 days | up to 45 |
| from 14 days or more | until 20.5 |
Exceeding the indicators indicated in the table is an alarm bell for specialists. In such cases, immediate medical measures and constant monitoring of the child’s condition are required.
The condition is characterized by yellowing of the skin and often goes away after a couple of weeks, but in some cases it can have serious consequences.
What amount of pigment should a baby normally have up to a month and what to do if the indicators are very high?
Bilirubin is a yellow-brown pigment formed as a result of the destruction of protein elements in the blood. It is involved in the formation of hemoglobin.
When red blood cells break down, hemoglobin is released, becoming toxic. The immune system, whose task is to protect the body, destroys it, as a result of which compounds that include iron - hemes - appear.
Special enzymes transform them into bilirubin, which is sent to the liver and is gradually excreted in urine and feces.
Bilirubin in an infant is always elevated, but jaundice occurs in 80–85%. In the body of a baby in the womb, oxygen is carried by red blood cells, which contain a lot of fetal hemoglobin.
When a child is born, its functions are lost and it is destroyed, leaving behind a yellow pigment. An adult's body works hard to remove this dye, but a newborn's liver is unable to cope with the increased load.
To obtain data on pigment levels, blood is taken multiple times.
When hemoglobin decomposes, indirect bilirubin is formed. It is highly toxic - during hypoxia, prematurity or due to other reasons leading to weakening of the newborn, it can concentrate in the brain tissue, provoking the development of encephalopathy. This pigment easily penetrates fat cells, which gives it the opportunity to disrupt the functioning of the body.
The dye binds to blood proteins, as a result of which only about 1% is deposited in the skin, and the bulk is sent to the liver, where it combines with glucuronic acid. This creates a direct type of pigment that poses no threat to the body.
In addition to the direct and indirect forms of bilirubin, whose amount in plasma is 75% and 25%, respectively, in medicine there is the concept of total bilirubin. This is a combination of two types of dye.
To determine the level of pigment, doctors do a blood test. Many mothers are interested in where they get biomaterial for research.
In the first minutes of the baby’s life, a syringe needle is inserted into the cut umbilical cord, and after 2-3 days, when the analysis is repeated, into the heel or a vein on the head. The procedure is completely safe.
During the study, all bilirubin fractions are determined. Premature babies are tested every day.
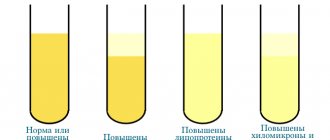
To determine the amount of pigment, a special device is also used - a bilirubinometer. This is a photocell that records the color of the skin on the baby’s forehead, bridge of the nose or chest and determines the degree of yellowness of the tissues. The device makes it possible to evaluate the effectiveness of therapy and predict the course of jaundice.
The bilirubinometer test is most often done in babies who do not have symptoms of jaundice. Its advantage is that the result is instantly displayed on the screen, but the disadvantage is that the device does not show direct and indirect dye levels.
The next time the study is carried out at one month of age during a routine examination. The biomaterial is taken from the heel, vein in the head or arm.
| Child's age (days) | Amount of bilirubin (µmol/liter) |
| Blood collection at birth | 51–60 |
| 1 | 85 |
| 2 | 180 |
| 3–5 | 256 |
| 6–7 | 145 |
| 8–9 | 110 |
| 10–11 | 80 |
| 12–13 | 45 |
| 1 month | 8,5–20,5 |
An increase in the amount of dye on the third day of life is normal. The limit is considered to be 256 µmol/l. If it is exceeded, this is evidence of jaundice.
If the values increase to 300 µmol/l, the child needs urgent medical attention, since the toxic dye begins to negatively affect the functioning of the liver and brain.
It is worth remembering that the bilirubin norm for a baby born at 36 weeks and a premature baby is different. At birth, its indicator in a premature baby is 71.8–106 µmol/l, and a day later – 97.4–148 µmol/l. The maximum value is observed at 5–6 days. Jaundice is diagnosed when the dye level limit reaches 172 µmol/L.
Pathological jaundice develops rapidly. In severe forms of the disease, the pigment content increases by 90 µmol/l daily. The disease proceeds for a long time (at least 3 weeks) and in waves, externally it manifests itself:
- poor appetite;
- yellowing of the skin below the navel, feet and palms;
- light feces and dark urine;
- depressed or overly excited state of the baby.
If elevated bilirubin is diagnosed in newborns, this is the first sign that jaundice has begun to develop. It has two forms:
- physiological jaundice, which in most cases does not pose a danger and goes away on its own by the 4th week of the baby’s life, but constant monitoring of the baby’s condition is required, since the disease can become complicated;
- pathological, which requires immediate treatment; in its absence, the risk of adverse consequences increases.
The reasons for high enzyme values are as follows:
- difficult pregnancy;
- complications during labor;
- prematurity;
- diabetes;
- asphyxia in the fetus during pregnancy or childbirth, for example, when the child is wrapped in the umbilical cord.
The values of indicators in the pathological form of jaundice can go off scale. In this case, the provoking factors are those listed above. In addition, excessively high bilirubin may indicate problems such as:
- hormonal imbalances;
- Rhesus conflict;
- liver pathology in an infant;
- obstruction of the intestines or biliary tract;
- diseases at the genetic level, against the background of which the erythrocyte membranes are destroyed.
- iron deficiency;
- chronic malnutrition;
- low level of fetal hemoglobin.
Bilirubin: normal in a newborn. Table by month
The situation when bilirubin in the blood of newborns exceeds standard values is not uncommon. Most often, this phenomenon goes away on its own. However, too high rates require additional treatment, as they can lead to significant complications. Therefore, high bilirubin should be treated extremely carefully.
Concept of bilirubin
Bilirubin is a product formed as a result of the breakdown of red blood cells. If their cycle of existence has already completed, they turn into toxic hemoglobin, from which the dye is formed.
In medical practice, it is customary to distinguish two types (fractions) of this substance: direct and indirect. Initially, indirect bilirubin is formed. It is slightly soluble and difficult to remove from the body. Therefore, first bilirubin is converted into direct bilirubin, which enters the liver, then into the gallbladder and is excreted through the intestines.
The human body makes every effort to get rid of this substance. However, the baby's liver is initially unable to cope with such a load. That is why in the first days of life it is so important to monitor whether the norm of bilirubin in the blood of newborns is observed. The table, which contains the threshold values of the indicator, is intended to help do this.
How to take blood for bilirubin
In the first days of life after birth, the baby undergoes blood donation for multiple tests. Among the latter is the determination of the concentration of bilirubin in the body. In this regard, most mothers are concerned about where the baby’s blood is taken from.
Special laboratories are equipped with professional equipment, with which you can establish the enzyme level with an accuracy of tenths of a micromole.
Thanks to this device, it becomes possible to determine the most accurate value of bilirubin in the blood fluid of an infant and provide timely treatment even before the first symptoms of jaundice begin to appear.
The analysis proceeds according to the following scheme:
- for the first time, blood is taken from the umbilical cord immediately after the baby is born;
- every other day the sampling is carried out from the heel;
- subsequent analyzes are carried out daily.
For babies who are at risk, that is, those born during a complicated pregnancy, blood fluid is taken from a vein in the head. For this, a special thin needle is used.
There is another way that allows you to control bilirubin levels - bilitest. It is used only as a preventative measure or when jaundice is not suspected.
This test is carried out with a special device that examines the color of the skin at the site of application. The tester allows you to measure the level of yellowness of the epidermis of a newborn, as well as determine the pigment concentration.
Bilirubin level is the most significant indicator that allows you to generally assess the health of a newly born child.
Experts do not recommend ignoring the analysis, since it can help identify the development of jaundice and other pathological abnormalities and begin timely treatment. The main thing is to remember that the lack of therapy can lead to not the most favorable consequences.
The liver of a newborn baby does not yet contain a sufficient amount of enzymes that are responsible for the “utilization” of bilirubin, so the content of this component in the baby’s blood in the first days after birth is almost always increased.
Normally, indicators should stabilize 5-7 days after birth. If this does not happen, or the amount of bilirubin initially far exceeds the permissible values, the child is prescribed treatment.
Doctors distinguish three types of bilirubin:
- indirect (the original type of bilirubin, which is practically insoluble and cannot be excreted from the body naturally);
- direct (bound bilirubin, which is formed in the liver from indirect bilirubin by combining with glucuronic acid);
- total (total amount of bilirubin contained in blood cells).
To diagnose pathologies in humans, the content of direct and total bilirubin is studied. If the values obtained are much higher than normal, the child may be suspected of pathologies of the liver and gallbladder or ducts: cirrhosis, hepatitis, biliary atresia, etc.
On the fourth day, the amount of bile pigment reaches a maximum, after which the indicators stabilize and begin to correspond to the established normal values (if we are talking about healthy children).
A child may be born with the following bilirubin levels, which are considered normal:
- 51 µmol/l is the average value for most newborns;
- 256 µmol/l - the maximum value for healthy children born at 37-41 weeks;
- 171 µmol/l - in healthy children born before 34-36 weeks.
What bilirubin values are considered normal are indicated in the table. It is worth considering that the amount of bile pigment can change every day until the neonatal period ends.
| Child's age | Amount of bilirubin (µmol/l) | ||
| General | Indirect (free) | Direct (tied) | |
| After birth | 23,09 | 14,37 | 8,72 |
| 2 days | 54,22 | 45,5 | 8,72 |
| 4 days | 90,14 | 82,27 | 7,87 |
| 6 days | 69,1 | 63,28 | 7,72 |
| 9 days | 53,02 | 44,3 | 8,72 |
| 3 weeks | 13,04 | 4,49 | 8,55 |
| 1 month | 11,12 | 2,57 | 8,55 |
In newborns, blood for analysis is taken from the heel. After receiving the results, the indicators are compared with normal values established for a particular age. If the content of coloring pigment is much higher than normal, the child will be prescribed a comprehensive examination and treatment, if necessary.
In most maternity hospitals, a special device, which is a photocell, is used to measure bilirubin. It is brought to the forehead of the newborn and the skin color is recorded, and a special program recognizes the pigment content in the skin. This method is more gentle, as it does not cause pain and can be used when the baby is sleeping.
But parents should know that the data obtained cannot be considered completely reliable, since the device has an error (the value is established for each category of device).
In addition, this method does not allow measuring bilirubin fractions, which is necessary to compile a complete clinical picture and determine the cause and degree of pathology (in cases where an increase in the total amount of pigment is determined).
Important! Measuring bilirubin using a photometer is allowed if the baby is healthy and the total bilirubin level is within the normal range. If any abnormalities are detected, it is better to use a blood test (more accurate and reliable).
This condition is called jaundice, which can be physiological or pathological (depending on the reasons that caused the increase in pigment).
In some cases, the child may experience yellowing of the eye sclera - this is an alarming sign that indicates the need for immediate examination.
The following factors can cause physiological jaundice:
- retardation in physical development caused by intrauterine abnormalities;
- feeding on artificial milk substitutes from the moment of birth (for example, if the mother is in intensive care);
- Rh conflict between mother and child (occurs when a woman has a negative Rh factor and the baby has a positive Rh factor);
- use of potent drugs during pregnancy (especially in the first and last trimester, as well as during childbirth);
- significant weight loss in the child in the first days after birth.
A pathological increase in bilirubin occurs in severe pathologies, for example, cirrhosis of the liver, hepatitis, atresia (obstruction) of the bile ducts, etc. Treatment of pathological jaundice comes down to treatment of the underlying disease, which takes a lot of time and is difficult for infants to tolerate.
This video covers many general points about bilirubin so that parents can understand physiological jaundice in newborns.
The death of nerve endings and brain cells can lead to tragic consequences, including:
- loss of vision;
- hearing impairment;
- dementia;
- mental disorders and deviations;
- severe delay in physical and intellectual development;
- persistent decrease in immunity.
Treatment of children older than two months is carried out according to the same scheme as therapy in adult patients. This is due to the speed of spread of intoxication and the severity of possible complications.
Parents should immediately consult a doctor if their baby exhibits the following signs:
- weakness of the sucking reflex;
- yellowness of the skin and eye sclera;
- lethargy, lack of appetite;
- anxiety, disturbed sleep;
- convulsions;
- nervous tic;
- enlargement of the spleen and liver.
During a routine examination of the child, the pediatrician may suspect a pathology based on low blood pressure and other signs characteristic of this problem.
Jaundice in newborns is not as harmless a problem as it might seem at first glance. In some cases, the reasons can be very serious. For example, with biliary atresia, a child requires urgent surgical treatment - otherwise there is a high probability of the child’s death. Therefore, you should not take tests such as measuring bilirubin in the blood lightly.
Timely treatment and preventive measures for the mother during pregnancy will help protect the baby from severe consequences and reduce the risk of postnatal complications.
What can jaundice lead to?
The threat to a baby with increased bilirubin is due to the fact that this pigment does not dissolve in water. This means that it is impossible to remove it from the child’s body naturally. But it is fat soluble, and is quite capable of settling in the subcortex of the brain. Deposition in the zone of the subcortical nuclei can lead to bilirubin encephalopathy, in other words, kernicterus. This happens due to intoxication of the subcortex of the brain. And it is extremely dangerous, as it can lead to disability of the baby, and sometimes ends in death.
Symptoms of kernicterus are:
- drowsiness, lethargy of the baby;
- the baby does not suck well at his mother’s breast;
- convulsions;
- loud, incessant crying;
- neck muscle tension.
It is precisely because of the danger of kernicterus that the level of bilirubin in the baby’s blood is thoroughly checked by doctors while he is in the maternity hospital. If the level is elevated, even slightly, bilirubin levels are tested three times a day.
How to independently recognize harmless jaundice:
- the skin becomes colored on the 2-3rd day, but never before the first day of life;
- the level of pigmentation increases gradually in the first 3-4 days of life;
- jaundice begins to disappear from the first week to the 10th day of life, and completely disappears by the second or third week;
- the baby feels well;
- the liver and spleen are not enlarged;
- stool and urine are of normal color.
Clinical signs of physiological jaundice in newborns (recognized by doctors). At birth, bilirubin taken from the umbilical cord is less than 51 µmol/l; the level of hemoglobin, red blood cell count and hematocrit corresponds to the norm; Bilirubin in the first day increases by 5.1 µmol/l per hour; The maximum permissible total bilirubin, estimated on days 3-4 of life, is not reaches a value of 256 µmol/l in children born during; and the indicator is 171 µmol/l in children born earlier than expected. The average bilirubin analysis is 103 - 137 µmol/l;
The indicator of skin colorability is usually assessed using the Cramer system:
| Stage | Description |
| I Art. | Only the face and neck are painted |
| II Art. | The skin is yellow up to the umbilical area |
| III Art. | The upper limbs turn yellow |
| IV Art. | All skin turns yellow |