A blood test for hidden infections is necessary to identify pathogenic microorganisms that are the causative agents of sexually transmitted diseases such as ureaplasmosis, mycoplasmosis, genital herpes, papillomavirus and cytomegalovirus diseases, hepatitis and HIV infection.
Laboratory diagnostics allows us to identify clinically silent diseases
Stages and signs of development of hidden pathology
A latent infection may not make itself felt for a long time, but be present in the body, that is, the carrier period can be quite long. Under certain conditions, for example, weakening of the functionality of the immune system, the pathogen initiates a pathological process, after which a full-fledged clinical picture of a particular disease develops. Each disease is characterized by its own characteristics of phasing and course, so it is impossible to distinguish strict stages in the development of a latent infection. We can definitely say only about two mandatory stages - the carrier stage and the stage of development of clinical symptoms.
The list of signs of latent infection also varies depending on the pathology. Sexually transmitted infectious pathologies do not always affect only the reproductive system. Therefore, the clinic can be diverse. Features of the symptoms of individual diseases will be discussed below.
Modern methods of testing for infections
How to get tested if a person wants to get tested on his own initiative? You should know that many infectious diseases can be detected using modern techniques by concluding an agreement with one of the licensed laboratories or a private clinic. Today there are express methods that allow you to find out results in a few minutes or within a day. Results from more complex tests will have to wait for several days.
You can start with a rapid test to determine C-reactive protein. A general finger blood test will answer the main question: whether there is a bacterial or viral infection in the body. Depending on the symptoms, doctors will propose an examination plan.
Why is it necessary to undergo timely tests to detect hidden infections?
The list of indications for prescribing an analysis for latent sexually transmitted infectious diseases includes:
- pain syndrome in the lower abdomen;
- Vaginal discharge in large quantities, with an unpleasant odor and uncharacteristic color;
- pregnancy planning;
- preparation for surgical intervention on the organs of the excretory and reproductive systems;
- accidental unprotected sexual intercourse;
- problems of infertility and miscarriage;
- monitoring the effectiveness of therapeutic correction of infectious diseases of the genitourinary system.
Analysis for hidden infections is especially important during pregnancy and during preparation for it. The doctor must issue referrals for examination to women who are planning to become pregnant, as well as monitor the health status of patients who are already carrying a child.
Intrauterine infections
Intrauterine infection (IU) is an infection that can develop in the fetus in the womb. Its source is the maternal organism. In this case, the baby is born sick or infected. In addition, infection is possible during childbirth, when the child passes through the woman’s birth canal.
A blood test for intrauterine infections includes tests to identify the following infectious diseases:
- complex of TORCH infections – toxoplasmosis, rubella, cytomegalovirus infection, herpes virus; these infections cause very severe intrauterine pathologies of the fetus, and most often their presence in a woman is an indication for termination of pregnancy;
- sexually transmitted infections – ureaplasmosis, mycoplasmosis, chlamydia, gonorrhea, trichomoniasis;
- HIV infection, hepatitis B and C viruses, syphilis.
Screening for intrauterine infections is mandatory for all pregnant women.
What are the hidden infections in women?
The list of diseases that can be detected after a laboratory examination includes the pathologies discussed below.
Colposcopy of the cervix - what is it and why is it prescribed?
Herpes virus and cytomegalovirus
Herpetic diseases - herpes simplex and cytomegalovirus infection - are widespread and can occur hidden. They are dangerous for pregnant women, therefore they are included in the list of mandatory tests (complex of ToRCH studies).
Human papillomavirus
An infection caused by the human papillomavirus. Certain types of HPV are provocateurs of oncological pathologies, in particular, cervical cancer. Currently, many countries are vaccinating against HPV types 16 and 18, which most often cause cancer.
Gardnerellosis
Gardnerellosis, or bacterial vaginosis, develops as a consequence of an imbalance in the vaginal microflora. The causative agent of the pathology is a specific microorganism – gardnerella. With the disease, the volume of vaginal discharge increases and it acquires an unpleasant odor.
Candidiasis
Candidiasis, or thrush, is a disease that develops due to an imbalance in the vaginal flora and the intensive proliferation of fungi of the genus Candida. The pathology is characterized by the appearance of cheesy discharge, as well as itching. The disease can manifest itself when the immune system is weakened and large doses of antibiotics are taken.
Mycoplasmosis and ureaplasmosis
These pathologies are provoked, respectively, by pathogens such as mycoplasma and ureaplasma. Taxonomically, these pathogens fall between bacteria, viruses, and fungi, sharing similar and distinct features with each of these classes. The main route of transmission of infection is sexual. Symptoms after infection may not appear for a long time. The disease can manifest itself when the functionality of the immune system decreases, that is, pathogens should be considered opportunistic.
For male patients, infection may be at risk of prostatitis, and for female patients, infection may result in damage to the endometrium and fertilized egg during pregnancy. Because of this, miscarriages, stillbirths are possible, as well as a negative effect on the development of the fetus in the case of normal gestation.
Chlamydia
The causative agent is chlamydia, an intracellular parasite. The disease can be asymptomatic, however, it is also dangerous for women during pregnancy, as it can have a negative effect on the fetus. In addition, the infection can cause infertility.
Gonococci
Gonococci provoke such an unpleasant and dangerous disease as gonorrhea. The pathology manifests itself as an intense inflammatory process, causing symptoms such as itching, profuse yellowish discharge, pain and blood during urination.
What other pathologies should you be aware of?
There are a number of other diseases to consider:
- Actinomycosis. If local immunity is impaired, actinomycetes can cause an inflammatory process on the mucous membrane.
- Trichomoniasis. The symptoms of this pathology include the appearance of copious foamy discharge with an unpleasant odor; the disease is also characterized by itching, discomfort when urinating, and discomfort during sexual intercourse. However, chronic trichomoniasis may not produce significant symptoms. Therefore, after a course of therapy for this pathology, it is necessary to undergo laboratory monitoring several times to confirm the cure.
- Hepatitis (B, C). The causative agents are hepatitis viruses, which can enter the human body through sexual contact. The disease may not make itself felt for a long time, however, it can provoke extremely serious consequences. Therefore, you should undergo regular preventive examinations.
- HIV infection. A dangerous disease, the causative agent of which can be sexually transmitted. To prevent the disease, preventive measures should be followed, excluding unprotected sexual intercourse, the use of unsterile medical instruments and other factors that can provoke infection.
Hidden infections are very insidious and can cause very serious illnesses. For this reason, the importance of regular preventive and clinical examinations is great.
Bacterial infections
Bacteria are single-celled microorganisms with an unformed nucleus. They reproduce by division and have their own metabolism. The most common bacteria are round-shaped (cocci) - streptococcus, staphylococcus, meningococcus, pneumococcus and others. There may also be rod-shaped bacteria in the human body - dysentery, whooping cough, intestinal and other bacilli. Other forms of bacteria are found much less frequently than these forms.
There are opportunistic bacteria. They are normally safe for humans. But when the immune system is weakened or certain disorders are present in the body, opportunistic bacteria turn into pathogenic (disease-causing) bacteria.
The main difference between a bacterial infection and a viral one is a longer incubation period, ranging from 2 to 14 days.
Symptoms
The most common manifestations of bacterial infection are otitis, sinusitis, pneumonia, and meningitis. The most well-known bacterial infections are intestinal infections, tuberculosis, tetanus, diphtheria, whooping cough, gonorrhea, and syphilis.
An experienced doctor can determine the presence of a bacterial infection through a blood test.
Analysis transcript
According to the interpretation of the blood test for bacterial infections, the following changes in indicators are observed in the results of the study.
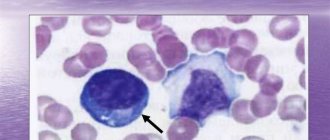
- An increased number of leukocytes - white blood cells, which are responsible for the body's immunity. This increase is observed due to an increase in the number of neutrophils, which are a special type of white blood cell. Neutrophils play a particularly important role in providing the body's defenses and at the same time constitute the most numerous type of leukocytes.
- Shift to the left of the leukocyte formula . This means that the content of neutrophils in the blood increases, and young forms of leukocytes appear - myelocytes and metamyelocytes.
- Decreased concentration of lymphocytes in the blood . Lymphocytes are another type of white blood cell. An increase in the percentage of neutrophils entails a decrease in the percentage of lymphocytes.
- ESR (erythrocyte sedimentation rate) increases. ESR is a nonspecific characteristic that reflects the presence of an inflammatory process in the body.
Diagnostics: what tests are performed for hidden infections in women
Analysis for latent infections can be carried out using several basic techniques:
- Enzyme-linked immunosorbent assay (abbreviated as ELISA). With its help, antibodies to antigens of pathogens of latent infections are determined in the blood. The technique is characterized by high sensitivity and specificity.
- Polymerase chain reaction (PCR). With its help, RNA or DNA of the pathogen is determined in biomaterial (smear from the vagina, urethra, blood, sperm). The technique is characterized by high accuracy and specificity; it allows one to determine the presence of genetic material of an infectious microorganism even in extremely small quantities.
- Bacterial culture with isolating a culture of the disease provocateur and determining its sensitivity to antibiotic drugs. The method is important for selecting the most effective treatment regimen for the disease when it is detected.
- Bacterioscopy. A smear is examined for hidden infections using microscopy.
Deciphering a smear for STIs can reveal gonococci, gardnerella, mycelium and spores of the fungus of the genus Candida, Trichomonas. If gonorrhea is suspected, another study is carried out, in which a smear of biomaterial is examined for gonococci.
What types of blood tests are there for STDs?
Today, there are several types of laboratory blood tests. The appropriateness of each of them will be determined only by the attending physician.
One of the simplest and fastest types is a general blood test . Its disadvantage is the impossibility of determining the type of pathogen. But a general analysis shows the presence or absence of an inflammatory process in the body. It is formed as an immune response to the penetration of a pathogenic microorganism. If the general condition of the body worsens, a general analysis will indicate the development of an inflammatory process.
In addition, one of the most accurate types of diagnostic research is distinguished. This is a polymerase chain reaction. Its essence is that the genetic material of the STD pathogen is repeatedly copied.
Then specialists determine the type of microorganism. In this case, the DNA or RNA of a microorganism is determined in a fragment of pathological material. The advantage of the method is the ability to obtain data even with a small amount of studied material.
PCR will allow analysis to be carried out in the early stages of disease development. This is done even at a minimum concentration of the pathogen.
Antibodies in the blood of STDs can be detected using an enzyme immunoassay. This type of study is based on the determination of antibodies. They are produced by the body in response to antigens of pathogenic microorganisms. When foreign proteins penetrate, the body tries to get rid of them. As a result, immunoglobulins begin to be produced.
There are three types of antibodies:
- IgA
- IgM
- IgG
Most attention is paid to immunoglobulins M and G.
Class M antibodies are the first to appear after infection. After treatment, they disappear.
Antibodies G can be detected later in the active development of STDs.
A special feature is their preservation after the bacteria are completely destroyed. In some cases, this type of immunoglobulin may persist throughout life.
Note! A serological reaction in the first days after infection may not give results.
Then the analysis should be repeated in a couple of weeks. Only in this case will it be possible to obtain a reliable blood test result.
Blood for STDs: PCR for HIV
In urology and gynecology, the PCR method is often used to determine various diseases. PCR is no exception in diagnosing HIV infection.
RNA fragments will be diagnosed in the material. This type of diagnosis has 100% specificity.
The studies do not take much time and are highly sensitive. This makes it possible to easily detect the cause of the disease in a short time. PCR is carried out even during the incubation period.
At that time, the infection had not yet manifested itself in the form of symptoms. The disadvantage of this method is the need for precise sampling of material. The room where the blood is taken is also required to be sterile.
HIV PCR can be performed within a couple of weeks after infection. The result is assessed as positive or negative.
To confirm the research, ELISA diagnostics are additionally prescribed. An analysis is carried out when antibodies to HIV infection appear. Diagnosis is carried out in two ways: serum or blood plasma is examined.
Venous blood is collected in the laboratory.
To obtain a reliable result, it is important to comply with the requirements for the preparation and collection of material. If you receive a false result, you should definitely repeat the study. In addition to the qualitative reaction, a quantitative analysis is also carried out.
It helps to establish the amount of pathogen in the body. The degree of damage is determined.
PCR may be prescribed in several cases.
Most often this occurs when characteristic symptoms appear:
- sudden decrease in body weight
- prolonged diarrhea for more than three weeks
- presence of fever
- swollen lymph nodes
- emergence of dangerous diseases
In this case, you need to consult a doctor and undergo a series of laboratory tests.
Remember! There is no need to engage in self-diagnosis and self-medication.
PCR testing for HIV can take one day.
Blood for STDs: PCR for hepatitis B and C
Hepatitis is an infectious disease that causes liver damage. A characteristic symptom is severe pain in the right hypochondrium. There is a bitterness in the mouth. A characteristic sign of the disease is yellowing of the skin and sclera. The color of urine and feces will change.
To establish the presence of the disease, diagnostics are carried out in the form of screening.
Let's celebrate! After infection with hepatitis C virus, antibodies to the infection are observed throughout life.
PCR allows you to determine the genetic material of the virus in the patient’s blood. Hepatitis C or B can be detected within 5 days after suspected infection.
The presence of hepatitis virus DNA indicates a positive reaction. In this case, treatment should be started immediately. A positive result means that the infection continues to multiply and infect liver cells.
PCR will determine microorganisms in digital equivalent. Indicators are measured in IU per milliliter.
A blood test for hepatitis should be performed before treatment. Taking medications may affect the reliability of the results.
Blood for STDs: PCR for cytomegalovirus
This is one of the most common infections in the world. The causative agent of the disease is cytomegalovirus. It belongs to the herpesvirus family. Infection can occur in several ways.
The following routes of infection are distinguished:
- Sexual contact
- Kisses
- In utero in children
- Blood transfusion
- Organ transplant from an infected person
The first symptoms most often do not appear with this infection. That is why I can mistake it for a regular ARVI.
The most common symptoms of cytomegalovirus are:
- dyspnea
- cough
- chills
- enlarged lymph nodes
- fever
Laboratory tests are used to make an accurate diagnosis. PCR is used to correct the barium molecules in the material.
It is carried out by repeatedly copying the genome of a microorganism.
This makes its identification easier.
The polymerase chain reaction is highly sensitive. This gives a great advantage over other studies.
It becomes possible to identify a microorganism in its latent course.
A positive result indicates the presence of cytomegalovirus in the body. In this case, treatment should be started immediately.
Blood PCR for herpes type 1 and 2
The study allows us to determine the DNA of the virus.
PCR is most often used to diagnose type 2 herpes. This type of analysis helps to identify the virus in its latent stage. It is at this moment that it is important to detect pathology and begin treatment.
The latent form of herpes can lead to a number of complications. A suppressed immune system, together with infection, provokes severe inflammatory processes. As a result, death cannot be ruled out. Therefore, when a diagnosis of herpes is made, drug therapy should be started immediately.
Herpes type 2 is also determined by a diagnostic test of the patient's blood.
At the same time, the presence and quantity of immunoglobulins are studied. G antibodies are usually used for identification.
Pregnant women and people with characteristic symptoms of herpes are referred for detection of this virus.
Antibody concentration indicators have their own interpretation. A result of up to 0.8 means that the person is healthy and no treatment is required.
If the indicator varies from 0.8-1.2, this indicates that the result is questionable. In this case, you should undergo re-diagnosis in a couple of weeks.
If the indicator is 1.2 or higher, the person is sick and requires treatment.
Important! Do not ignore the symptoms, be sure to visit a specialist and get your blood tested.
Antibodies in the blood for STDs
To make an accurate diagnosis and identify the infection, a comprehensive antibody test is performed.
Diseases such as syphilis, HIV, hepatitis, chlamydia, and mycoplasmosis can be examined. They, as a rule, may not manifest themselves for a long time.
The incubation period ranges from a week to two months. For diagnostic testing, only venous blood is donated.
Let's take a closer look at how to get tested for different STDs.
Blood test for syphilis
This sexually transmitted disease occurs as a result of the penetration of Treponema pallidum into the body.
The first sign of syphilis is the formation of chancre. It has the appearance of an ulceration with smooth edges. This formation does not cause pain or discomfort.
If left untreated, secondary signs of syphilis begin to appear. These include polymorphic rashes. They look like a pink papular rash. The rashes are small in size. Early diagnosis is very important.
What types of blood tests are performed if syphilis is suspected?
There are several research methods:
- RIBT
- RPGA
- total antibodies
- RPR
Such analysis methods allow timely detection of infection and control of the treatment process.
One of the main research methods is the search for antibodies to Treponema pallidum. M antibodies appear first in the blood. They mean that the infection is in an acute stage.
The period of manifestation of this type of immunoglobulin is about 14 days from the moment of infection. Next, G antibodies appear. This type of antibody begins to grow rapidly 3-4 weeks after infection.
Their presence indicates chronic infection or a previously transmitted disease.
Blood test for chlamydia
Chlamydia occurs as a result of unprotected sexual intercourse. Characteristic symptoms are discomfort in the lower abdomen.
There is burning and itching in the urethra. After some time, you can detect discharge in the form of mucus with pus. Sometimes symptoms may not appear.
Remember! Advanced infection leads to complications, such as infertility.
The first antibodies appear five days after infection. After a couple of weeks, a second type of antibody appears and tends to grow.
The accuracy of this research method for chlamydia is about 80%. For a more accurate diagnosis, it is additionally recommended to undergo a PCR test.
Blood for STDs: antibodies to ureaplasma
Ureaplasma is an opportunistic flora. Normally they exist in the human body.
Under the influence of a decrease in the functioning of the immune system, their intensive growth begins. As a result, the inflammatory process is activated. In this case, a blood test will help make a diagnosis.
Blood for STDs: antibodies to mycoplasma
Research is carried out in specially equipped laboratories. Mycoplasma affects the genitourinary system and causes an inflammatory process.
The titer of one of three types of antibodies is determined. This is necessary to obtain data on the development of the disease.
Indications for analysis are symptoms of diseases of the urogenital area. Tests are required during pregnancy planning and registration.
Indications for testing for mycoplasma are infertility and unprotected sexual intercourse. Blood for analysis is taken from the ulnar vein.
During the chronic course of mycoplasmosis, G antibodies will appear. After treatment, they circulate in the blood for several months and then disappear.
The doctor will determine the treatment methods. The need for therapy appears when the result is positive. An advanced course of the infectious process can lead to miscarriage and a number of other complications.
Blood for STDs: antibodies to Trichomonas
The disease occurs as a result of infection with the single-celled microorganism Trichomonas. This disease belongs to urogenital pathologies.
May appear without characteristic symptoms. That is why laboratory diagnostics are carried out.
Now the basis of research is to determine the presence of Trichomonas in the blood. Afterwards, the species identification of the microorganism is carried out. Several research methods are used to identify microbes in the blood.
But the most informative is diagnostics with the determination of antibodies. For this purpose, enzyme immunoassay is used. The result form will indicate a negative or positive answer.
Blood for STDs: antibodies to gardnerella
Diagnosis of gardnerellosis is most often carried out in women. Because the opportunistic microorganism Gardnerella provokes bacterial vaginosis.
The bacterium is normally present in a woman's vagina. The growth of the microbe provokes changes in the pH of the environment and causes pathological disorders. To confirm the presence of Gardnerella, blood is tested for antibodies to it.
Diagnostics must be carried out in the following cases:
- the appearance of white discharge with a grayish tint
- presence of burning and itching
- unpleasant fishy odor from discharge
- redness of the mucous membranes and skin
For more accurate diagnosis, PCR for Gardnerella is used. By repeatedly copying the material, the DNA of the microorganism can be easily determined.
A false positive or false negative result is possible. The quantitative method helps to determine how intensively the disease develops.
Additionally, ELISA is used. Its main task is to identify antibodies. After completing the course of therapy, you should definitely be tested for gardnerellosis again.
The presence of gardnerella in men is not the norm. In this case, it is necessary to start treatment.
In women, a minimal amount of bacteria is normal. In this case, you can do without treatment.
Attention! Therapy is prescribed only by a doctor; do not self-medicate.
Blood for STDs: antibodies for candida
Candida diseases are quite common.
The reason is the intensive growth of the fungus of the genus Candida. It can be located both on the skin and mucous membranes. When diagnosing the disease, blood tests for antibodies and a smear from the genital organs are performed.
The smear is examined using microscopy or bacteriological culture on nutrient media. Most often, this is quite enough to accurately identify the pathogen.
In some cases, serological studies are carried out:
- atypical external manifestations of candidiasis
- localization of fungi in a place unusual for them
- abundant spread of candida throughout the body
- pronounced symptoms of general intoxication
Such signs indicate that the disease is atypical. That is why research should be carried out with special attention. Using an enzyme immunoassay, the presence of IgA, IgM, and IgG antibodies is examined.
You should avoid eating a few hours before sampling. This is necessary for the reliability of the results.
If the body functions normally, the result will be negative. The procedure for collecting and processing blood is carried out under sterile laboratory conditions.
How to properly prepare for testing for hidden infections
Before visiting a medical facility to donate biomaterial from the vagina or urethra, you must:
- exclude sexual intercourse for two days;
- within two days, eliminate the use of intravaginal tablets, suppositories and douching;
- do not urinate for two hours before taking biomaterial;
- Women are recommended to take the test on days 4-5 of the menstrual cycle, immediately after the end of menstrual bleeding.
Flora smear in women: interpretation of results
Before visiting the laboratory to donate blood for analysis, you should:
- do not eat for 8 hours (it is recommended to donate blood in the morning on an empty stomach);
- for two days do not drink alcohol and do not eat too fatty, smoked, salty foods;
- do not smoke immediately before donating blood;
- eliminate physical and emotional stress;
- Consult your doctor about the need to stop taking medications.
What infections can be detected by a blood test?
Blood testing for STIs includes taking samples of biomaterial, helps to accurately determine any of the varieties of sexually transmitted diseases of bacterial, fungal and viral etiology known to medicine. Experts divide such pathologies into several groups, depending on the types of pathogens.
The first group includes diseases of bacterial etiology. We are talking about syphilis, gonorrhea, chlamydia, mycoplasmosis, ureaplasmosis, granuloma inguinale, chancre. The second group combines pathologies of a viral nature: anogenital herpes, HIV infection, AIDS, hepatitis B and C, papillomas of the external genitalia caused by the human papillomavirus (HPV), molluscum contagiosum, cytomegalovirus. The third group consists of protozoal infections, the most common of which is trichomoniasis. The fourth group includes pathologies that are fungal in nature.
When diagnosing most of the listed infections, not only blood is used, but also a smear for STIs in men and women. Infections primarily affect the human reproductive organs. In the past, many of them were incurable, now they can be successfully treated, but require a long-term and carefully followed course of therapy, and if left untreated can lead to hormonal disorders, chronic inflammatory processes of the external and internal genital organs, infertility and more serious consequences. Thus, syphilis, if left untreated, destroys the entire body, including the central nervous system and brain. Today, AIDS, hepatitis B and C are incurable, however, when detected at an early stage, they turn into a sluggish form, with which patients can maintain a normal quality of life for a long time. In the matter of timely diagnosis of STDs, blood tests are of decisive importance.
How do they test for hidden infections in women and men?
Universal urogenital probe for collecting biomaterial
During the examination, a gynecologist or urologist takes biomaterial using a sterile disposable instrument. In men, the material is taken from the urethra, and in women - from the vagina, cervix and urethra. After this, either a smear is made and the glass is delivered to the laboratory, or the biomaterial is placed in a disposable tube and also sent for research. The speed of analysis depends on the workload of the laboratory.
Procedure for collecting blood for analysis
They also take a blood test for hidden infections. Blood is taken from the cubital vein, centrifuged, serum is collected and a study is performed.
Preparing for a blood test for STDs
You should know the rules for preparing for research. This will avoid false results.
It is necessary to donate blood for analysis on an empty stomach. Eating food and various drinks will distort the result. In addition, it is strictly forbidden to drink alcohol before the study. It is not recommended to eat excessively fried and peppered foods.
If you plan to take a smear, you must avoid sexual intercourse. Scrapings of the rash may be performed.
Blood can be taken not only from a vein, but also from a finger.
It is necessary to stop taking antibacterial drugs before diagnosis. Medicines can significantly distort the result.
How soon will the results and their interpretation be ready?
The speed of analysis depends on the workload of the laboratory, but on average it takes 1-2 days. The exception is bacteriological tests, which require a longer wait - 5-7 days. The study is deciphered by a specialist. In a healthy state, no infections should be detected. If the presence of a disease pathogen in the biomaterial is confirmed, consultation with a specialist is necessary to prescribe treatment.
Note! After a course of therapy, regular laboratory monitoring is required, which is designed to confirm the effectiveness of treatment and promptly take the necessary measures if complete cure has not been achieved.
PCR tests at a dermatovenerologist
Most often, infectious diseases are diagnosed using PCR. This method is more informative and accurate than microscopy.
With a microscope you can only see candida, gonococci and trichomonas. The remaining pathogens are indistinguishable. In addition, the doctor may confuse gonococci with other microorganisms. Therefore, microscopy is not a 100% accurate test. It is more indicative than confirmatory.
But PCR has a specificity and sensitivity close to 100%. This study produces virtually no false positive or false negative results.
The nucleic acid amplification reaction makes it possible to identify even those pathogens that do not cause any symptoms and are contained in minimal concentrations in clinical material. Any clinical material can be used to perform PCR.
The doctor may take for analysis:
- smears from different organs;
- sperm;
- blood;
- prostate secretion;
- urine.
PCR directly detects the DNA of a microorganism. Therefore, the study is informative only if the clinical material is obtained directly from the area where the infectious agent is located.
PCR allows you to specifically search for a specific bacteria or virus. That is, in the process of diagnosing chlamydia it is impossible to find herpes. If PCR is carried out for chlamydia, then the doctor receives an answer whether this bacterium is present in the body, and in what quantity. This study differs from microscopy. Because, studying the material under a microscope, the doctor may look for gonorrhea, but find trichomoniasis.
When carrying out PCR, the DNA found in the sample is compared with the standard. The nucleotide sequence is used to identify the microorganism. Usually PCR is prescribed for several infections at once.
The most commonly used clinical material for diagnosis remains a smear from the urethra. Although in men, ejaculate and the first portion of morning urine can be used instead.
Infection during pregnancy
Hidden infections are extremely dangerous for the health of mother and baby.
Diagnosis of latent infections in pregnant women is extremely important, since some pathologies are quite dangerous and can lead to undesirable consequences, which include the risk of miscarriage and developmental defects in the baby. Therefore, during pregnancy, a woman must undergo tests several times to identify hidden infections. Timely detection of pathology will prevent the development of serious complications.
Smear for the degree of purity in women: interpretation
Intestinal infections
It is necessary to take a stool test if the following symptoms are detected:
- nausea;
- loose stools, especially signs of blood during bowel movements;
- vomit;
- stomach ache;
- temperature is above normal.
Antibacterial treatment should be prescribed only after pathogens have been identified, so analysis for viral infections is necessary. To identify protozoa, it is important to deliver feces to the laboratory within 30-40 minutes, storing it in a closed container at a temperature of +2 to + 4 degrees Celsius. It is necessary to collect a volume equal to half a teaspoon.
No special preparation is required for the test, however, given that laboratories operate in the morning, it is necessary to ensure defecation. The use of an enema is not allowed. The day before, you should follow the drinking regime and exclude drugs and foods that can lead to constipation. When collecting stool, it is necessary to ensure that no discharge from the urinary canal or vagina (in women) gets into the container (a jar with a screw cap). It is unacceptable to use cardboard or matchboxes to collect feces.
To carry out bacterial culture, a smear is taken from the anus. If the results are negative (causative agents of salmonellosis, dysentery, etc. are not identified), the doctor does not exclude rotavirus infection. There are rapid tests that can make a diagnosis within minutes.
It should be remembered: intestinal infections are transmitted from infected people through dirty hands and common household items. The carrier of the disease may not show signs of the disease. That is why minors and everyone working in children's groups must undergo regular scheduled examinations.