What can be seen with fluorography
This diagnostic method is very common for the early detection of lung pathology. This is an x-ray method that involves reflecting x-rays from the tissues of internal organs. Fabrics of different densities are able to reflect radiation in different ways, which makes it possible to see them in the picture.
What does fluorography of the lungs show? With its help you can see the following changes in the chest organs:
- disturbances in the structure of lung tissue;
- inflammation of the lung parenchyma;
- presence of neoplasms;
- heart and vascular diseases;
- foci of pulmonary tuberculosis;
- proliferation of connective tissue in the lungs;
- the presence of cavities: cysts, abscess (purulent cavity);
- occupational diseases of the respiratory system associated with the accumulation of dust or other harmful emissions in the lungs (pneumoconiosis, anthracosis, sarcoidosis).
Complications
Most often, cirrhotic tuberculosis is accompanied by complications such as:
- pulmonary hypertension - increased blood pressure in the pulmonary artery system (large trunks and small branches);
- cor pulmonale – enlargement of the right chambers of the heart (atrium and ventricle), which occurs against the background of pulmonary hypertension;
- respiratory failure - a violation of the respiratory function of the lungs, which is manifested by a deterioration in the supply of oxygen to them and the release of carbon dioxide from the lung tissue;
- multiple organ failure - dysfunction of various organs that occurs due to oxygen starvation, which, in turn, develops against the background of respiratory failure;
- hematomegaly - enlargement of the liver. Occurs against the background of pulmonary hypertension and redistribution of blood between the pulmonary and systemic circulation;
- splenomegaly is an enlargement of the spleen that occurs for the same reason as hepatomegaly.
Indications for fluorography
This diagnostic method is used both for preventive purposes (once a year) and for certain ailments:
- determining the cause of cough, chest pain, shortness of breath;
- suspicion of pneumonia (pneumonia);
- the presence of pathology of the heart and blood vessels (atherosclerosis, aortic aneurysm, pathology of the heart valves);
- contact with a patient with tuberculosis;
- suspected HIV infection;
- search for foreign bodies in the respiratory tract and upper gastrointestinal tract.
Development mechanism
The first stage of the disease is characterized by the appearance of small pathological foci. They begin to expand, capturing a segment or lobe of lung tissue. In this case, the doctor diagnoses infiltrative tuberculosis of the upper lobe of the left lung (or right). The infiltrate is an accumulation of connective tissue threads, cells from the alveoli, macrophages, and blood leukocytes. When they merge, pneumonia develops.
The next phase (with decay) proceeds with the melting of tissues and ends with the appearance of cavities (cavities). With proper treatment, resorption or scarring of the infiltrate occurs, and a capsule may form around it.
Contraindications to fluorography and x-rays
Although identifying foci of tuberculosis on an x-ray is the most informative way to diagnose this disease, x-ray examination is associated with radiation exposure, and therefore there are a number of contraindications to its implementation:
- child's age under 15 years;
- the patient’s serious condition, in which it is impossible to transport him to the X-ray room;
- pregnant women, especially during the first trimester, since this is when the child’s organs are formed;
- women during lactation;
- respiratory failure with severe course.
Preventive measures and prognosis
Prevention includes a set of the following measures:
- regular medical examination - annually;
- organize quarantine when the first cases of infection appear;
- undergo mandatory vaccination;
- comply with sanitary and hygienic requirements in the home and workplace.
Timely and adequate therapy promotes the resorption of exudate.
The further picture has several development options:
- complete restoration of the affected structures;
- formation of scars in certain areas;
- in the case of predominant changes of a sclerotic nature, an induration field is formed.
A less favorable prognosis is when a capsule forms in the area of infiltration with a high probability of infiltrative-pneumonic tuberculoma.
The progressive form has two development options:
- Caseous pneumonia is the predominance of caseosis over the exudative inflammatory process.
- The decay and formation of cavities, which serves as the next stage of the disease.
In the absence of extensive fibrosis, cavities are effectively eliminated using collapse therapy, which often leads to scarring. Drug treatment with anti-tuberculosis drugs normalizes blood quality parameters.
Differences between fluorography and x-rays
If it is necessary to examine the organs of the respiratory system, many people have a question about what to choose: fluorography or x-ray of the lungs.
Fluorography is a cheaper method, since it requires less film. In addition, you don’t need to use special devices to develop it; the pictures appear immediately on the film. Due to its high availability, fluorography has become widespread during preventive examinations.
However, it is not as accurate and informative as x-rays. Therefore, to make an accurate diagnosis and control the disease over time, it is necessary to conduct a chest x-ray. Another advantage of X-rays is lower radiation exposure, so if X-ray diagnostics are necessary, this method is prescribed for pregnant women and children.
Can pneumonia turn into tuberculosis?
Inflammation in the lungs cannot develop into a tuberculosis infection. When tuberculosis is diagnosed after pulmonary inflammation, it is likely that an incorrect diagnosis of pneumonia was initially made.
If a person is sick with pneumonia, immunity decreases, which creates conditions for infection with Koch's bacillus, which enters the body from patients. But the incubation period of mycobacteria is long; during lung disease, tuberculosis infection does not have time to develop.
Those who have previously had a tuberculosis infection should think about whether tuberculosis may develop after pneumonia. There is a danger of upper lobe pneumonia developing into tuberculosis when tuberculous mycobacteria are already present in the body.
How does lung pathology appear on x-ray?
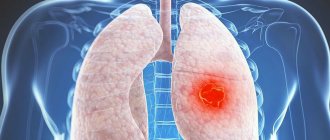
With the development of a pathological process in the lung tissue, the most characteristic radiological symptom is the presence of a shadow in the lung. Therefore, many may have a question about darkening in the lungs on fluorography. What does it mean?
The darkening can be total (cover the entire lung tissue) or local (occupy a small area). Total blackout is a shadow of white light without clear contours, occupying most of the lungs. It can be either one- or two-sided.
Radiologists divide a limited shadow into a focus and an infiltrate. The lesion has a diameter of up to 10 mm, and the infiltrate is more than 10 mm. The infiltrate does not have clear contours and most often occurs with pneumonia (inflammation of the lungs), pleurisy (inflammation of the pleura - the membrane surrounding the lung).
When answering the question of what is darkening of the lungs on fluorography, it is also worth separately highlighting the symptom of a single round shadow. As a rule, it is a lesion measuring 10-15 mm and can appear with the following diseases:
- tuberculoma;
- peripheral tumor;
- abscess;
- cyst;
- artery aneurysm (sac-like protrusion of its wall).
Multiple round shadows may be a manifestation of how tuberculosis looks in the picture. They are also characteristic of cancer metastases to the lungs.
Features of the anamnesis
A history of pneumonia includes previous episodes of hypothermia, alcohol abuse, viral infection, or influenza. Frequent lung infections plague smokers.
Predisposing factors for infection with Koch's bacillus include poor nutrition and living in a damp, cold climate.
If you are surrounded by a tuberculosis patient at work or at home, then the person is also at risk.
Tuberculosis manifests itself:
- hollowness of the subclavian and supraclavicular fossae, which is caused by insufficient nutrition;
- swelling of the face;
- atrophy of the respiratory muscles;
- decreased lung volume;
- lag of the affected side of the chest when breathing;
- narrowing of intercostal spaces;
- deformation of the fingers in the form of “drum sticks” with expanded end phalanges;
- convex shape of nails (“hour glass”).
While examining the patient, the doctor determines the condition of the lymph nodes. With pulmonary tuberculosis, the cervical, axillary, and thoracic nodes can become inflamed.
Tuberculosis disease is characterized by temperature variability. The difference between pneumonia and tuberculosis is that the increase in temperature during tuberculosis infection is moderate, not exceeding +38°C, and with pneumonia, severe fever develops.
Types of tuberculosis
The way tuberculosis looks on X-rays directly determines the type of disease.
The following radiological types of tuberculosis are distinguished:
- infiltrative;
- cavernous;
- fibrous-cavernous;
- disseminated;
- cirrhotic;
- primary tuberculosis.
Classification, types and phases of the disease
Phthisiatricians distinguish five main types of infiltrates depending on the type and location of the mass. Treatment tactics and strategies differ depending on these types. These include:
- Round. Localization occurs in segments 1, 2 and 6. On an x-ray it looks like a rounded figure, which in some cases has an area of disintegration. The boundaries are clearly visible.
- Cloud-shaped. Has fuzzy contours and weak intensity. Often turns into caverns.
- Regional (periscissuritis). Divided in the central part by a groove. The shape is triangular, with one of the corners turned towards the lung, and the other outward.
- Lobit. Occupies a large area, sometimes constituting a full share. The image shows areas of decay.
- Lobular (lobular). Several parts are concentrated around the source of decay.
The disease can develop in different directions. In medical practice, it is customary to distinguish two of them:
- Involutive. In this case, the patient’s chances of recovery are high - the situation is characterized by positive dynamics, the positive results of therapy become noticeable 4-6 months after its start. The intensity of symptoms decreases, and the pulmonary structure begins to normalize.
- Progressive. The clinical picture shows a sharp and stable deterioration of the condition. The lesions enlarge and merge. The disease continues to develop at an accelerated pace, and its companions are diseases that reduce the body’s immune defense.
The second direction is dangerous because symptoms may disappear for a short period of time, which patients associate with cure. The main mistake is stopping taking prescribed medications.
Treatment depends on what phase of development the disease is in:
- Resorption phase. At this stage, positive dynamics are observed. The rotting processes stop, and the affected area begins to overgrow. Reducing the lesions leads to an improvement in the condition.
- Compaction phase. The infiltrate accumulates and forms tissue compactions covered with fibrous fibers.
- Dissemination phase. It is a latent form in which deterioration in well-being is attributed to a cold and fatigue. Small foci are formed, which are located next to the infiltrate.
- Decay phase. It is considered the most dangerous of all those described above. Cavities formed into one clot can disintegrate into parts, which begin the inflammatory process again.
There are situations in which the immune system cannot cope with damage to the body and maintain it in a satisfactory condition. Then caseous pneumonia develops, which threatens the formation of many foci that occupy the entire lung area.
Infiltrative form
This is the most common form of tuberculosis, occurring in more than 60% of cases. It is characterized by widespread necrosis (death) of lung tissue. Depending on what fluorography of the lungs shows, several subtypes of infiltrative tuberculosis are distinguished:
- round infiltrate - darkening of an oval or round shape in the upper parts of the lungs, most often under the collarbone;
- cloud-like infiltrate - a shadow of a homogeneous structure with uneven boundaries;
- marginal infiltrate - the shadow has the shape of a triangle, the apex of which is directed towards the root of the lung;
- lobular infiltrate - is a group of fused foci of varying density;
- Lobit is a large shadow that covers an entire lobe of the lung and has a heterogeneous structure.
Classification and phases of development of pathology
Experts divide this disease into the following clinical and radiological variants:
- Cloud-like infiltrate, which X-ray shows as a weak homogeneous shadow that does not have clear outlines. This form of tuberculosis pathology is characterized by rapid decay of lung tissue and the formation of new cavities.
- A round lesion, which an x-ray shows as a rounded focus, has clear boundaries. As a rule, the localization of the lesion is in the subclavian zone.
- Lobular infiltrate, the radiography of which is characterized by an eclipse of irregular shape, formed as a result of the fusion of several lesions. Very often such foci are formed with decay in the center.
- Volumetric cloud-like infiltration of a triangular shape. With this option, the infiltration process affects the interlobar pleura, which in some cases leads to the development of tuberculous pleurisy. With a cloud-like infiltrate, x-rays show a predisposition to decay and the formation of cavities.
- Focal infiltrative tuberculosis affecting the entire lobe of the lung.
If we take the size of the lesion as the basis for the classification, we distinguish small (with a size of 1-2 cm), medium (from 2 to 4 cm), large (from 4 to 6 cm) and widespread (over 6 cm) lesions. X-rays will help determine the size of the lesion.
As for the classification of pathology by type of infiltrate, the following groups are distinguished:
- A typical infiltrate with a homogeneous focal lesion area, the size of which reaches several centimeters.
- The soft-focal form, which looks like a darkening on an x-ray and represents the initial stage of pneumonic changes.
- Hilar infiltration, when the lymph node of the lung root is damaged.
It is the type of infiltrate that is of great importance in diagnosis - according to it, the doctor determines the strategy of therapeutic action. However, treatment of infiltrative pulmonary tuberculosis is impossible without establishing the degree of development of the pathology. In this regard, experts identify the following phases of this pathology:
- resorption;
- compaction;
- lung collapse;
- contamination.
In the first phase, the lesion is reabsorbed, and the resulting cavity is covered with scars. Even if the infiltrate does not completely resolve, you can notice a decrease in its amount in the organ cavities.
The compaction stage is characterized by the fact that the infiltrate is converted into dense tissue that contains fibrous fibers. Tuberculosis without decay poses a danger to the patient, since even in the absence of symptoms, the lesion may open at some point, as a result of which the development of the pathological process will begin again.
Infiltrative tuberculosis in the phase of decay and contamination poses the greatest danger. The infiltrate disintegrates and cavities form in the lungs. In the decay stage, pulmonary tuberculosis is contagious, and the patient requires especially careful care and separate housing with a more serious approach to hygiene issues. requires compliance with all these conditions for the patient. Otherwise, this is fraught with the development of serious complications. In the phase of seeding or dissemination, multiple foci are formed in the area located close to the infiltrate.
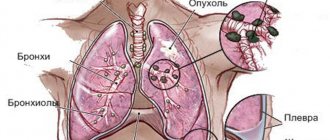
Cavernous form
Cavernous tuberculosis on x-ray is characterized by the presence of cavities, or caverns. They are formed during necrosis and breakdown of lung tissue. With a prolonged course of the disease, connective tissue grows around the cavity, then another form of tuberculosis occurs - fibrous-cavernous.
All cavities in tuberculosis can be divided into several groups depending on their structure:
- encapsulated - the cavity has a wall of three layers (capsule);
- sanitized - the cavities do not contain pus and remain after recovery;
- elastic - cavities have suppuration inside, and their wall consists of two layers;
- fibrous - the formation of a connective tissue membrane around, which indicates a transition to the next form.
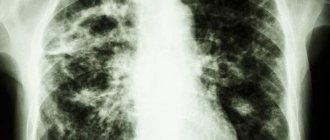
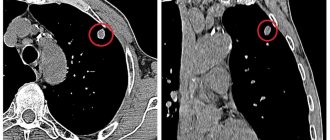
On X-ray, the cavernous type of tuberculosis looks like this:
- a white rounded shadow (darkening), in the center of which black lung tissue is identified (clearance);
- clear contours of the shadow;
- there may be a so-called path to the root of the lung.
The most common location of cavities is the upper parts of the lungs, under the collarbone.
Differences in clinical manifestations
There are many differences between these diseases. Here are the main ones:
- Pneumonia, as a rule, begins acutely and with a sudden rise in temperature, up to febrile levels. It rises sharply and falls sharply, which is manifested by profuse sweating. Tuberculosis begins gradually. The body temperature is usually not high (low-grade), it rises cyclically. Sweating is also common, but it mainly occurs at night.
Symptoms of pneumonia
- With pneumonia, the skin of patients is cyanotic, as gas exchange is impaired as a result of the accumulation of exudate in the alveoli. The skin with consumption is pale. Lobar pneumonia, like tuberculosis, is also characterized by a blush on the cheeks.
- Pneumonia is a rapidly progressing infection, so the general intoxication syndrome is quite pronounced compared to tuberculosis. It manifests itself as: significant headache, weakness and muscle pain, joint pain, decreased blood pressure, nausea and even vomiting.
- Pneumonia is characterized by a varied auscultatory pattern. Either weakened vesicular breathing is heard, or when the bronchi are involved in the inflammatory process, bronchial breathing is heard. The initial stages of the development of the disease are also characterized by the presence of dry wheezing, which is then replaced by wet wheezing (medium bubbling or fine bubbling).
Pathological bronchial breathing
This disease is also characterized by crepitus. In tuberculosis, auscultation is not particularly indicative. Breathing is often vesicular, rales are either absent or a small amount of moist rales is heard, crepitus is not typical.
Fibrous-cavernous form
Is evidence of a chronic tuberculosis process. Deformation of the tissue of the lung and upper respiratory tract (trachea, bronchi) occurs. This course of the disease is characterized by alternating exacerbations (with cough, hemoptysis, shortness of breath) and remission, when nothing bothers the patient.
The description of images of tuberculosis in the fibrous-cavernous form has the following features:
- a cavity with a thicker and more pronounced wall than in cavernous tuberculosis;
- displacement of the trachea towards the formation of a cavity;
- deformation of the pulmonary pattern;
- placement of cavities in the upper sections.
Forecast
The prognosis for cirrhotic pulmonary tuberculosis is different. Death is inevitable within several years from the moment of diagnosis. The prognosis can be improved if the described disease is detected in time and the progressive proliferation of connective tissue in the lungs is prevented.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
1, total, today
( 41 votes, average: 4.10 out of 5)
Tuberculosis during pregnancy: risks for mother and fetus, treatment
Coxsackie virus, Coxsackie epidemic in Turkey 2020: transmission routes, symptoms, treatment and prevention
Related Posts
Disseminated form
This form of tuberculosis can be divided into acute, subacute and chronic. As a rule, it develops acutely with the rapid spread of tuberculosis bacilli throughout the body.
There is another classification depending on the method of spread of mycobacteria:
- hematogenous - X-rays show larger lesions located in the upper parts of the lungs;
- lymphogenous - medium-sized lesions located mainly in the lower sections;
- lymphobronchogenic - characterized by unilateral lesions in the lower parts of the lung.
The way tuberculosis looks in the picture depends both on the nature of its spread and on the severity of the process. The most characteristic subtype of disseminated tuberculosis is miliary tuberculosis. It is an acute, most often hematogenous infection.
Its main signs on x-ray are listed below:
- a large number of small lesions, several millimeters in diameter;
- lesions are evenly distributed throughout the lung field;
- sometimes the lesions merge;
- the roots of the lungs are somewhat raised;
- sometimes the volume of lung tissue becomes smaller.
Signs and diagnosis of the disease
The cirrhotic form of tuberculosis has a wave-like course, in which periods of exacerbation alternate with remissions. The severity of symptoms depends on the location of the lesion and its size. If cirrhotic changes are localized in one of the segments or upper lobes of the lung, symptoms are often mild or completely absent. During the period of remission, the patient is bothered by slight shortness of breath and attacks of dry cough. During an exacerbation, in most cases, symptoms do not increase.
Severe symptoms are observed when the damage is localized in the lower lobes of the lungs or when there is a large area of the cirrhotic area. Then the symptoms resemble a purulent form of bronchitis:
the patient develops a severe cough, during which purulent sputum is expelled,
- the disease is accompanied by shortness of breath, reminiscent of asthma, and hemoptysis, an increase in body temperature to 38-39 degrees is observed,
- symptoms of intoxication appear - general weakness, body aches, headache,
- During auscultation, moist rales are heard,
- if the damage affects all lobes of one or both lungs, the patient develops pronounced constant shortness of breath, the heartbeat accelerates, and the skin turns blue.
When the process worsens, a person becomes infectious, releasing many mycobacteria into the external environment.
Pressure increases in the pulmonary circulation, so such patients are at risk of rupture of pulmonary vessels and bleeding. As a result of blood entering the respiratory tract, aspiration pneumonia develops. Over time, signs of heart failure increase. The patient has:
- limbs swell,
- liver enlarges
- Fluid begins to accumulate in the abdominal cavity.
Long-term purulent intoxication contributes to the development of visceral amyloidosis and chronic renal failure, which often cause death.
Diagnosis includes a doctor’s examination and additional examinations. During the inspection, the following is discovered:
- pallor of the skin and mucous membranes,
- blueness of fingertips. The finger phalanges resemble drumsticks, and the nails resemble wristwatch glass,
tachycardia and low blood pressure.
If the cirrhotic areas are in one lung, the doctor notes:
- asymmetry of the chest,
- during the respiratory act, lag of one half of it,
- dullness of sound during percussion is noted,
- weakened breathing,
- wheezing is heard in the affected area and above it, which intensifies with exacerbation of the tuberculosis process.
The main method for diagnosing the disease is chest x-ray. The X-ray picture is determined by the primary form of the disease. If cirrhotic tuberculosis occurs against the background of an infiltrative or fibrous-cavernous form of tuberculosis, darkening of varying intensity with clear boundaries can be seen in the pictures.
Dense calcified lesions are more intensely darkened. Inside them, areas of light color are often found, having a round or oval shape - bronchiectasis. In some cases, slit clearings are visible. These are residual cavities.
Thickening of the pleura is also observed. The remaining areas of the pulmonary parenchyma have increased airiness, the cause of which is emphysematous swelling. Identical changes are found in a healthy lung.
If the cirrhotic process occurs against the background of other forms of tuberculosis localized in the middle lobe of the lung tissue, “middle lobe syndrome” can be seen on x-rays.
Approximately in the middle of the lung, a darkening with clear contours is visible. In cirrhotic tuberculosis, which developed against the background of a disseminated form, areas of darkening are detected in the upper half of both lungs.
The pleurogenic form of cirrhosis on x-ray is manifested by a decrease in the size of the affected lung. In addition, the image shows a displacement of the mediastinal organs towards the pathological focus and an increase in the airiness of the remaining pulmonary parenchyma.
Sputum examination is also carried out. During the period of exacerbation, Mycobacterium tuberculosis is detected in it. During remission, Koch bacilli are often absent from the sputum. Sputum culture is needed to detect nonspecific microflora. Its presence indicates active inflammation.
Tuberculin diagnostics and bronchoscopy are performed very rarely, since in cirrhotic tuberculosis their results do not have significant clinical significance. In rare cases, spirometry is prescribed.
Cirrhotic form
This type of tuberculosis process is characterized by large-scale destruction of lung tissue and the growth of connective fibers in its place.
On x-ray, the cirrhotic form appears as follows:
- Massive high density darkening, looks like a bright white shadow;
- reduction in the volume of the affected lung;
- porous appearance of the pulmonary pattern in the lower sections;
- displacement of the root of the lung and the shadow of the mediastinal organs to the painful side.
Causes of cirrhotic pulmonary tuberculosis
The direct cause of the development of the disease is other types of tuberculosis, and their cause, in turn, is Mycobacterium tuberculosis.
This pathology does not occur in all patients - some are cured, others die. But if the tuberculosis process went through all its stages of development, then sooner or later it would end in cicatricial degeneration of the lungs.
Factors that contribute to the faster occurrence of the described pathology are:
- elderly age;
- accompanying illnesses;
- smoking;
- hypoxia (oxygen starvation) of tissues against the background of other diseases - in particular, those in which the lumen of the feeding blood vessel decreases.
Primary tuberculosis
This form of tuberculosis affects children or the elderly. There are three subtypes:
- tuberculosis of unknown localization;
- tuberculosis of intrathoracic lymph nodes;
- primary tuberculosis complex.
In the first subtype, despite the presence of symptoms, changes in the lungs cannot be detected on x-ray. Therefore, further examination is necessary to determine the localization of the pathological process.
In the second subtype, the mediastinal lymph nodes are affected: parabronchial, paraaortic, paratracheal. The way tuberculosis looks in the picture directly depends on the location of the affected lymph nodes:
- characterized by expansion of the root of the lung with blurred edges;
- there may be heterogeneity in the lung fields.
Primary tuberculosis complex is determined on x-ray in the presence of the following three signs:
- “path” that goes to the root of the lung (lymphangitis);
- root expansion associated with inflammation of the lymph node (lymphadenitis);
- a high-density focus in lung tissue that occurs due to the deposition of calcium salts (Hohn's lesion).
Treatment of cirrhotic pulmonary tuberculosis
The most important task in cirrhotic pulmonary tuberculosis is to support respiratory function. Practitioners define a complex task in simple words as follows: “It is necessary to preserve what is.” This means that the scarring processes are irreversible, so their development must be stopped, and the remaining functioning tissue must be protected from damage.
The main purposes for cirrhotic pulmonary tuberculosis are:
- anti-tuberculosis drugs;
- immunostimulants;
- vitamins;
- non-steroidal anti-inflammatory drugs - to eliminate nonspecific inflammation;
- mucolytics - to facilitate sputum discharge.
note
With massive growth of connective tissue, the lung loses its functionality, so its affected part is surgically removed.
Differential diagnosis of tuberculosis
Typically, when diagnosing tuberculosis using x-ray, it is necessary to be able to distinguish it from lung cancer and pneumonia. Often there is practically no difference in the images of pneumonia and tuberculosis, especially with the infiltrative form. However, there are some differences. Pneumonia is usually a unilateral lesion, while tuberculosis in most cases affects the lung tissue on both sides.
In addition, in case of pneumonia, the infiltrate is localized in the lower parts, and in case of tuberculosis - in the upper parts. The infiltrate is more pronounced in tuberculosis; there are often foci of destruction and dissemination.
It should also be noted whether the images show cancer different from tuberculosis. Sometimes this is quite difficult to do, especially with focal forms of tuberculosis. A number of the following signs will help with this:
- the cancer shadow is intense, with more blurred contours;
- the shadow of cancer in most cases has a homogeneous structure;
- the growth of the tuberculosis process, if there is no dissemination, is limited to the pleura, and therefore does not grow into the adjacent lobes of the lung;
- Cancer can spread to adjacent lobes.
Diagnosing tuberculosis using x-rays is quite difficult, and only a doctor can make a final diagnosis and prescribe effective treatment. After all, tuberculosis is not a death sentence!
Cirrhotic pulmonary tuberculosis: what is it?
Cirrhotic pulmonary tuberculosis develops after a certain time from the onset of another type of tuberculosis. The described disease is actually the final stage of such a process and can appear in a period from several years to tens of years from the moment this pathology is first detected in a patient.
note
The disease is a kind of indicator that the tuberculosis process was not pronounced, mycobacterium tuberculosis did not provoke destruction of the lungs, and the detected disorders of the lung tissue were rather chronic.
In some regions, cirrhotic pulmonary tuberculosis occurs in approximately one patient in ten with any tuberculous process in the lungs. But regions were also identified in which, among one hundred patients with any form of pulmonary tuberculosis, the described pathology occurred in only one. Such statistics cannot be regarded as the most accurate indicator of morbidity: some patients could die before experiencing the later consequences, which include cirrhotic pulmonary tuberculosis.
Treatment options
Treatment of infiltrative pulmonary tuberculosis has some features. Patients must be treated in an anti-tuberculosis hospital, since this disease is extremely contagious to others. The course lasts 2-3 months, after which maintenance treatment is carried out for 3-4 months until the infiltrates are completely resolved. The patient must follow all doctor's recommendations and take medications regularly. The use of traditional medicine can aggravate the course of the disease.
Drug therapy
This disease is treated with the following medications:
- first-line anti-tuberculosis drugs: Isoniazid, Pyrazinamide, Rifampicin;
- reserve agents: Prothionamide, Rifabutin, Kanamycin;
- hepatoprotectors: Karsil, Essentiale, Heptral;
- immunomodulators: Bioaron, Imiquimod, Inosine;
- glucocorticoids: Kenacort, Metipred, Medrol;
- anti-inflammatory drugs: Nimesulide, Ibuprofen;
- analgesics: Analgin;
- biogenic modulators: Aloe extract, Plazmol.
If the disease is particularly severe, the doctor prescribes several medications at the same time. After recovery, a course of anti-relapse chemotherapy is required. If no positive result is observed during treatment for 3-6 months, the doctor reviews the treatment regimen, adjusts the dosage of drugs and may replace some drugs with stronger ones.
You need to contact a pulmonologist if treatment does not cope with the pathology. This type of tuberculosis has a large number of clinical forms, so the methods of exposure must be complex. In difficult cases, surgery is performed.
Surgery
With infiltrative tuberculosis in the decay phase, a decision may be made to perform an operation - collapse therapy. During this type of surgery, air is injected into the pleural cavity to cause collapse of the affected lung. Due to the decrease in the volume of this organ, cavities and other lesions collapse, and the process of tissue restoration also accelerates, since the lung is at relative rest.
There is rapid healing and a delay in the flow of toxic substances from the affected areas into healthy tissue. As a result, the overall intoxication of the body is reduced.
In some cases, such a procedure can cause the development of the following complications:
- pneumopleuritis;
- the occurrence of air embolism;
- lung injury with the development of pneumothorax;
- pleurisy;
- subcutaneous emphysema.