Functions of the spleen
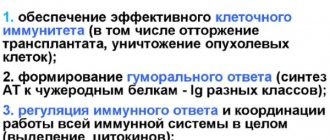
The main task of this organ is to filter blood and fill the body with a sufficient amount of it. There are other functions:
- control of blood flow from overload - when running fast, it starts to prick in the side, this is how the spleen is triggered;
- removal of outdated red blood cells;
- protective function, neutralization and filtration of harmful substances and viruses;
- immunoglobulin synthesis;
- control of the metabolic process in which iron is produced in the body.
Most often, ultrasound of the spleen is performed in conjunction with an examination of the abdominal organs. But in some cases it is necessary separately. Why and for what purpose is an ultrasound examination of the spleen performed?
Ultrasound of the spleen in adults and children
Ultrasound examination is based on the action of ultrasonic waves, which are completely harmless. Efficiency is slightly lower compared to MRI
, and others, but there are no restrictions. There are no contraindications to ultrasound for either children or adults. Ultrasound of the spleen can be done at all stages of pregnancy, in infants from the first days of life and in any patient several times throughout the disease, since ultrasound does not use any radiation technologies. The doctor decides how often an ultrasound of the spleen should be done. When it comes to ultrasound of the spleen, preparation for the procedure has no special requirements.
Ultrasound of the spleen
is an effective and, from a financial point of view, affordable research method, therefore, if the spleen hurts, ultrasound can recognize the normal size in adults. Based on the deviations, the doctor will prescribe effective treatment.
Indications for the study
When doing an ultrasound of the abdominal organs, the specialist is obliged to examine the spleen. But there are reasons why only ultrasound of the spleen is performed. The doctor prescribes a study if there are:
- blood diseases;
- diseases of the gastrointestinal tract;
- infectious diseases;
- abdominal trauma;
- suspicion of cancer;
- suspicion of spleen disease;
- anomalies/pathologies of the spleen.
Thus, ultrasound of the spleen may be indicated for:
- the appearance of bitterness in the mouth;
- constant heaviness in the left hypochondrium;
- feeling of discomfort after eating;
- increased gas formation;
- girdling pain attacks in the right and left hypochondrium.
When is it prescribed?
There are many indications for ultrasound examination of this organ. They are:
- suspicion of the formation of malignant tumors;
- injury to the body in the organ area;
- leukemia and similar neoplastic pathological processes;
- the presence of infectious diseases: typhus, various types of sepsis, syphilis, tuberculosis;
- abnormal factors in development or functioning;
- suspected portal hypertension.
Preparation
In order to obtain reliable research, preparation is required for the procedure. Foods that contribute to gas formation in the intestines should be excluded from the diet. These include fresh vegetables and fruits, legumes, and foods containing yeast. Enterosorbents are prescribed to the patient within 2-3 days.
On the eve of the spleen ultrasound, you should cleanse the intestines with an enema. The study is carried out on an empty stomach. The last meal should be seven to eight hours before the test. Patients with diabetes are allowed a light breakfast.
For what diseases and conditions is it performed?
Examination of the spleen using ultrasound makes it possible to identify various diseases in the early stages of development, which include:
- cystic formations;
- volumetric processes of malignant and benign nature;
- abscesses;
- necrosis of organ tissue;
- traumatic tissue damage to an organ with the formation of a hematoma;
- diseases of the body's lymphatic system;
- developmental anomalies.
Early diagnosis by ultrasound of the spleen, especially with closed abdominal injuries, will allow timely treatment of the pathological process and avoid various serious complications.
Carrying out the procedure
An ultrasound of the spleen lasts from fifteen to twenty minutes. The patient lies on his back, the body is freed from clothing. The specialist applies a gel that improves the conductivity of the beam to the left upper abdomen. During the procedure, you may need to turn on your right side, hold your breath for a while or take a deep breath, and lie down on a special cushion. All these movements and manipulations are necessary due to the specific location of the organ in order to conduct detailed studies. The test results are ready almost immediately after the procedure.
The essence of the study, its varieties
The essence of the method of ultrasound examination of an organ is to obtain a fairly clear image of the tissues of the spleen using an audio signal reflected from its surface and recorded as a picture by the sensors of the device.
Ultrasound of the spleen is performed using special linear, convex and sector probes. The organ is examined from the back through the left side. And if the spleen is enlarged, then it will also be visible from the abdomen. A good ultrasound diagnostic result is also possible with the patient in an upright position.
Spleen norms according to ultrasound: transcript of the study
What does the study show, what are the norms of the spleen according to ultrasound in adults and children, what data is recorded by the diagnostician? The healthy organ is located in the upper left part of the abdominal cavity. The diameter of the splenic vein does not exceed 0.5 centimeters. The structure of a healthy organ should be of a uniform, fine-grained structure. The shape of the spleen resembles a crescent; a change in shape indicates a disease. The heterogeneous structure of the organ can be a symptom of benign tumors. Any deviation from the norm, excess size, or impaired echogenicity are signs of the disease.
What is the size of the spleen according to ultrasound in adults:
- length 8-14 cm;
- thickness 3-5 cm;
- width 5-7 cm;
- weight of a healthy male/female organ – 190-200 g/150-152 g.
We also note that the thickness of the maximum cut is 40-50 square meters. cm.
It should be remembered that the above dimensions of the spleen (normal according to ultrasound) are average indicators; the parameters may differ in each individual case.
What is the size of the spleen according to ultrasound in children?
Their spleen norms vary depending on age. In general, there are only two indicators, length and width.
In a newborn baby:
- length - 40 mm;
- width - 38 mm.
Children from one to 3 years old:
- length - 68 mm;
- width - 50 mm.
Children from 3 to 7 years old:
- length - 80 mm;
- width - 60 mm.
Children from eight to twelve years old:
- length - 90 mm;
- width - 60 mm.
Children from twelve to fifteen years old:
- length - 100 mm;
- width - 60 mm.
Clinical interpretation of liver ultrasound results
SonoAce Ultrasound Magazine
Contains current clinical information on ultrasonography and is aimed at ultrasound doctors, published since 1996.
Introduction
Ultrasound examinations (ultrasound) are often the first in a series of diagnostic searches for suspected liver pathology, determining the choice of other techniques. Improvements in ultrasound diagnostic technologies have led to the fact that in some cases it has become possible to abandon other radiological examinations. But this also increases the responsibility of the specialist and requires a clinical interpretation of the results obtained, without reducing the description to the recording of “echo-positive” and “echo-negative” formations. The main share of ultrasound in outpatient settings is performed on the abdominal organs. And the liver is the first thing that a specialist tries to visualize in this case. Liver diseases can be suspected based on complaints, clinical picture, laboratory data, but they are often detected by chance. The latter applies, first of all, to children, in whom the proportion of congenital pathologies is higher than in adults. The reserve capacity of the liver is incredible, so the doctor’s task is to identify pathology before it becomes clinically significant.
General provisions
Embryogenesis of the liver and its vessels, anatomy. In early ontogenesis, the liver, gallbladder and bile duct arise as a single outgrowth (hepatic diverticulum) in the caudal part of the anterior duct. This formation grows ventrally into the septum transversum, which is the mesoderm between the developing heart and the midgut. The liver bud grows very quickly, occupying most of the abdominal cavity in the first 10 weeks. During this period, the sizes of the right and left lobes of the liver are the same, but due to oxygenated blood from the hepatic vein, the right lobe quickly overtakes the left in size and weight. From the 6th week, the liver is a hematopoietic organ, and from the 12th week it synthesizes bile. A small caudal process on the hepatic diverticulum gives rise to the gallbladder, and its stalk gives rise to the cystic duct. From the cord running from the hepatic and cystic ducts to the duodenum, the common bile duct is formed. During the embryonic period, blood enters the liver through the umbilical vein, which passes along the free edge of the ligamentum falciforum into the left branch of the portal vein. This part v. portae connects to the hepatic vein through the ductus venosus, then blood enters the right atrium. Thus, the ductus venosus is a large venous shunt that bypasses the liver, thanks to which the bulk of the blood from the placenta flows directly to the heart. This is the only route through which the catheter can be passed. If the catheter, when probing the umbilical vein, enters the right branch of the portal vein, thrombosis, obliteration and portal hypertension develop. After the birth of the child, the umbilical vein is obliterated and turns into the round ligament of the liver (ligamentum teres). Ductus venosus transforms into ligamentum venosum. In the first hours after birth, these structures can be visualized as canalicular. Later, the ligamentum teres is visible as a dense structure extending from the left side of the portal vein. If intrahepatic pressure increases (in cirrhosis), the round ligament of the liver is recanalized. Portal blood begins to flow from the liver to the navel, resulting in varicose veins (caput medusae). Anomalies of the inferior vena cava are possible, but they are extremely rare. Among these rare defects, the most common is the left-located inferior vena cava, which independently flows into the right atrium through the coronary sinus. Possible underdevelopment of the hepatic segment of the inferior vena cava with blood drainage through the vv system. azygos et hemiazygos. The hepatic vein drains independently into the right atrium. It is possible for the inferior vena cava to double, with the left vein being significantly smaller in diameter than the right. Knowledge of these features is especially important in pediatric practice, since a significant part of pediatric pathology is congenital.
Location features
(The author expresses gratitude to Medison for the equipment provided. Figures 2-4 are also provided by this company)
.
When starting your workday, check the condition of your equipment. Make sure the sensor set allows you to complete all studies. Ensure that the referral outlines the indications for the study, formulates the purpose and objectives, and presents the main clinical, laboratory and instrumental results. In a conversation with parents and the child (if he can formulate his problems), clarify all unclear points. Look at the patient as a doctor, and not as a performer with a device. Critically evaluate previous data and formulate your testimony. Have a clear work plan: the period during which the child is calm and allows the procedures to be carried out is short.
For ultrasound of the liver, spleen, and upper abdomen, a convex sensor is most suitable. The viewing angle is large, and the near-field deformation is minimal. The linear sensor is suitable for visualizing small structures. Doppler sonography is necessary if vascular anomalies or hemangiomas are suspected.
Scanning is best done with the child in the supine position with maximum inhalation or exhalation (depending on the child’s characteristics). When inhaling, the lungs push the liver, gall bladder and spleen below the costal arch, displace the colon, increasing the acoustic window. In older children, examination through the intercostal spaces or in a lateral projection is sometimes required. Intercostal access is optimal when the liver is located deep in the hypochondrium. To avoid false conclusions with non-standard approaches, the researcher must remember the changing topography of the organ, violations of the usual relationship with it of the kidneys, inferior vena cava, and intestines. If during the examination of the liver doubts arise about the condition of the gallbladder or biliary tract, and the child is not sufficiently prepared, it is better to complete the examination and repeat it after preparation. The most important advantage of ultrasound over other non-invasive imaging methods (radiography, magnetic resonance imaging - MRI or computed tomography - CT, retrograde cholangiopancreatography - RP) is the ability to repeat the study as often as dictated by the clinic.
Sonographic picture of a normal liver.
Normally, a child's liver is homogeneous. The nature of signal processing is chosen depending on the purpose of the study (Fig. 1a, 1b). The liver capsule is thin and echogenic. The echogenicity of the liver parenchyma is higher than that of the renal cortex parenchyma. The medullary tissue of the kidneys is darker than the liver parenchyma. The ventral edge of the liver is thin and sharp. As the size of the liver increases, it becomes rounded. A frequent indication for ultrasound is a suspicion of an increase in liver size. There are many formulas for calculating liver size, including volumetric ones. The latter are used mainly for scientific purposes or in specialized clinics. The size and configuration of the liver are quite variable. With routine studies, liver size can be assessed qualitatively. The right lobe of the liver extends to the lower pole of the kidney, but if there is a Riedel lobe (a normal variant), then it is slightly lower. In children 1 year of age, the left lobe extends beyond the midline during transverse scanning; in older children, it extends to the aorta. With hepatomegaly, the left lobe extends all the way to the spleen, moving it down. Displacement of the spleen may cause an erroneous conclusion about splenomegaly. Thus, the liver consists of right and left lobes. In addition, there is a caudate lobe. The liver lobes are divided into segments. Simplified - the right lobe has anterior and posterior segments (the border is the right hepatic vein). The left lobe consists of medial and lateral segments (the border is the left hepatic vein). Each segment has its own blood supply. Therefore, with Budd-Chiari syndrome (obstruction of the hepatic veins), the segments increase in size and their echogenicity increases. Knowledge of liver segments is also important for accurate localization of space-occupying lesions.
Rice. 1.
Echogram of the liver in normal mode and in MRI reconstruction mode.
A)
Echogram of the liver of a 12-year-old teenager in normal mode. Note that even at 12 years of age, the round ligament of the liver (arrow), which arises from the left side of the portal vein, has a canalicular appearance (lumen inside).
b)
Echogram of the liver of the same teenager in MRI mode. Multiple small echoes, most likely originating from connective tissue, were removed. The parenchyma and vessels themselves are clearly visualized.
Hepatic veins
carry blood from the liver to the inferior vena cava and right atrium. Three-phase Doppler curve. In diastole, the wave is directed towards the liver; in systole, two short, low waves have the opposite direction. Factors determining wave amplitude:
- increased liver density reduces amplitude;
- normal fluctuation changes with heart failure, expansion of the inferior vena cava;
- extrahepatic formations and ascites, compressing the liver and veins, change the fluctuations of the Doppler curve.
Portal vein
brings blood from the intestines and spleen. At the porta hepatis it divides into right and left branches. The total diameter of the vein varies depending on age, body position (standing or lying down), and depth of breathing. For practical purposes, we can assume that in children under 10 years of age the diameter is v. portae is about 8 mm, after 10 years - 10 mm (see table). The walls of their intrahepatic sections are highly echogenic and stand out well against the background of the parenchyma. Wall density is used as a standard for assessing the density of liver parenchyma. In chronic liver pathology, its density approaches the density of the walls of the intrahepatic branches of the portal vein. The Doppler wave is monophasic, fluctuations are determined by respiration and cardiac output. Among the anomalies of the portal vein, its agenesis, duplication and preduodenal portal vein are known. The latter is often combined with the reverse arrangement of internal organs, annular pancreas, duodenal stenosis or other anomalies.
table 2
. The diameter of the portal vein in children of different age groups.
| Age, years | 1 | 3 | 5 | 7 | 9 | 11 | 13 | 15 |
| Median, mm | 3,3 | 4,5 | 5,8 | 7,7 | 8,0 | 8,2 | 8,7 | 8,9 |
| Oscillation limits, mm | 2,9-5,7 | 3,5-6,9 | 4,3-7,6 | 4,5-8,5 | 4,9-9,4 | 5,1-10,0 | 5,6-10,1 | 5,7-10,6 |
Hepatic artery
carries oxygenated blood from the aorta. The pulsation of the Doppler curve corresponds to the cardiac cycle.
Private problems
Liver changes in newborns and children of the 1st year of life
are similar to its changes in older children, but their spectrum is somewhat different. Hepatomegaly is the most common reason for ultrasound examinations in newborns.
Causes and echographic picture.
- Metabolic liver diseases
(glycogenosis, etc.). The liver is enlarged in size and its echogenicity is increased. - Congestive heart failure.
The echogenicity of the liver is increased. The veins of the liver and the inferior vena cava are dilated. - Congenital hepatitis.
By the time of birth, the liver usually has increased echogenicity. - Hemangiomas and hemangioendotheliomas
are the most common local formations in the liver in children 1 year of age; in 80% of cases they manifest themselves in the first 6 months of life. Formations can be single, multiple or diffuse. Multiple small hemangiomas are hypoechoic; solitary hemangiomas are usually hyperechoic, as in adults. At the same time, lesions can be detected in the spleen. Calcification is observed in 13-17% of cases. Cavernous hemangiomas may appear as rough, irregularly shaped cystic lesions. A thorough Doppler analysis is required to identify feeding and draining vessels and arteriovenous shunts. - Neuroblastoma
(4S neurobastoma). It accounts for up to 50% of all cases of neonatal tumors. Median age at diagnosis was 22 months. Up to 80% of all cases are detected during the period of distant metastases. Echographically, the enlarged liver looks like it is infiltrated with metastases, and the primary focus in the adrenal glands is detected in only 40-50% of cases.
Diffuse liver changes in children
can be caused by both systemic and local pathological processes.
The echographic picture in most cases is not specific, combined with hepatomegaly and often jaundice. Diffuse changes in the liver usually occur in combination with hepatomegaly. The exception is cirrhosis of the liver, which in advanced stages leads to a decrease in liver size. In addition, diffuse changes in the liver are usually combined with its hyperechogenicity. Exceptions include acute liver edema and acute hepatitis
. Against the background of the hypoechoic liver parenchyma, the walls of the veins of the portal system are especially clearly visible.
In case of diffuse changes in the liver, it is necessary to determine its size, the nature of the surface (smooth, bumpy) and edges (sharp, rounded), the condition of the spleen, pancreas, kidneys, liver vessels, and lymph nodes.
Fatty liver
- the result of fat accumulation in hepatocytes. The echogenicity of the parenchyma increases, the pattern of the veins of the portal system is erased. The contrast between the liver parenchyma and the kidney is sharp. The severity of the changes depends on the degree of fatty infiltration. Fatty infiltration is observed as a result of chemotherapy and steroid therapy, with malnutrition, obesity, cystic fibrosis, tyrosinemia, Wilson-Konovalov disease, glycogenosis, etc. Fatty infiltration can also be focal. The focus of fatty infiltration can be of any size and shape, which simulates a tumor.
Cirrhosis
- not an independent disease, but the outcome of many liver diseases, against which the development of hepatocellular carcinoma is possible. In an acute process, fatty infiltration is first recorded. Later, granularity of the parenchyma appears. The process can be micronodular, in which the entire liver parenchyma changes, and macronodular, in which nodes with a diameter of 1 cm or more are visible in the altered parenchyma. The parenchyma is heterogeneous due to hypoechoic foci of regeneration. Fibrosis forms as strands of connective tissue, so the attenuation of the beam is less than with fatty infiltration. The liver decreases in size, and the left and caudate lobes increase compensatoryly. With the macronodular type of cirrhosis, the edge of the liver becomes uneven. Increased density of the liver leads to its rigidity and impaired blood flow. The usual three-phase wave along the hepatic veins can turn into fluctuating or monophasic. As an additional sign of cirrhosis, ascites is indicated (Fig. 2).
Cystic fibrosis
is transmitted in an autosomal recessive manner and is registered among Caucasians with a frequency of 1:3000-1:2500 live births. The cause of the disease is a disruption in the transport of ions from the epithelial cells of the exocrine glands with the formation of thick secretions, obstruction of hollow organs, infection and the development of sclerosis. Liver damage is characterized by macrofocal fibrosis.
Rice. 2.
Echogram of the liver with cirrhosis.
Portal hypertension
- inability of the portal system to freely transport blood to or from the liver. The resulting excess pressure leads to an enlargement of the spleen and the appearance of varicose veins of the portal system and the opening of collaterals. The basis of diagnosis is the identification of splenomegaly, varicose veins, and collaterals. There are three types of portal hypertension:
- subhepatic - the most common variant in childhood. May be idiopathic, the result of catheterization of the umbilical vein, ascending infection (omphalitis; appendicitis with phlebitis of the superior mesenteric artery flowing into v. portae, and thrombosis of the latter);
- intrahepatic. Cirrhosis with obstruction of intrahepatic branches v. portae;
- suprahepatic. Veno-occlusive disease is a partial or complete occlusion of the small hepatic veins, usually reserve for the larger veins, with blockage of blood flow through the liver. In children, it usually occurs after hematopoietic stem cell (bone marrow) transplantation, radiotherapy or chemotherapy. The term “Budd-Chiari syndrome” is often used as a synonym, although this is not entirely true. The term “Budd-Chiari syndrome” is commonly understood as a blockade of blood flow through the hepatic veins during hypercoagulation. Therefore, the term veno-occlusive disease is more universal. Vascular occlusion usually begins with intrahepatic venules. The veins flowing into the inferior vena cava may still be preserved for some time, which can cause a false negative diagnosis. Sonographic diagnosis is difficult. Ascites, thickened gallbladder walls, and atypical blood flow through the portal vein are detected. In severe veno-occlusive disease, the hepatic veins have a small diameter and are poorly visualized.
The echographic picture depends on the level of obstruction. With subhepatic portal hypertension v. portae is practically not visualized, but its cavernous transformation (portal cavernoma) is clearly visible. Cavernous transformation - many small collaterals bypassing the thrombosed v. portae. It develops in the next 1-3 weeks after thrombosis. According to Doppler ultrasound, portal blood flow is depressed and may be reversed. Collateral channels open. In total, at least 20 such channels have been described, but the following are of clinical significance and are easily identified by ultrasound.
- Esophageal and gastric veins
are identified easily and most often. On longitudinal scanning, the gastroesophageal junction is located immediately to the left of the aorta. Color Doppler scanning reveals varicose veins around the lower esophagus and along the undersurface of the liver. Some veins are located in the wall of the esophagus, others along its surface. The latter serve as a source of bleeding and are clearly detected by esophagogastroscopy. - Splenorenal collaterals
form from the hilum of the spleen and conduct blood into the left renal vein. Echographically they look like an additional vessel between the spleen and the left kidney in combination with an enlarged renal vein. This is an optimal shunt: there is no bleeding from it. - Paraumbilical collaterals
are rarely found in children and only in cases of cirrhosis. They originate from the left branch of the portal vein and extend to the navel. Blood is drained through the epigastric veins into the external iliac. It is these veins that form the caput medusae. Another sign of opening of paraumbilical collaterals is thickening of the lesser omentum. To identify this phenomenon, a longitudinal scan is performed at the level of the celiac artery. Normally, the distance from the celiac artery to the lower surface of the liver (the thickness of the lesser omentum) is 1-1.5 times the diameter of the aorta. If there are collaterals in the lesser omentum, its thickness is 1.7 or more times the diameter of the aorta. - An arterioportal shunt
connects the hepatic artery and the portal venous system. Its hemodynamic significance varies greatly. With a large discharge, portal hypertension and heart failure occur due to the large stroke volume of the left ventricle (a sharp reduction in the time of blood return to the heart). Occurs with tumors, vascular anomalies, as a result of injury due to unsuccessful liver puncture.
Focal changes in the liver
can be benign or malignant. Benign focal liver lesions include cysts, abscesses (purulent, fungal), hydatid disease (echino-, alveococcosis), hematomas, mesenchial hamartoma, hemangioma.
True cysts
are rare in childhood. They can be present in polycystic disease, therefore, if a cyst is detected in the liver, and even more so multiple cysts, it is necessary to examine all parenchymal organs. A true cyst is anechoic, its wall is not visualized, and the phenomenon of increased sound behind the cyst is clearly visible. Cysts are usually detected by chance; they are asymptomatic until they reach large sizes and do not displace or compress the liver structures. Small cysts are located along the periphery of the liver and are much better detected by CT than by ultrasound. Secondary cysts form as a result of a hematoma or abscess. Such cysts have heterogeneous contents and a thick wall.
Abscesses are pyogenic, fungal, amoebic
have common echographic manifestations. Pyogenic and fungal abscesses are typical for children with primary immunodeficiency (especially chronic granulomatous disease), HIV infection, and chemotherapy. Abscesses are usually localized in the posterior part of the right lobe and can be multiple or single. Echographically they may look like:
- small echo-negative formations;
- the bull's eye phenomenon, i.e. round echo-negative formation with an echo-dense center;
- target liver. Because abscesses can be very small, high-frequency probes are required.
Hydatid liver disease
- echinoid alveococcosis. The incidence among children increased by 2.9 times (“Distribution of parasitic incidence across the territory of the Russian Federation” on the website www.rusmedserv.com). Echographically, echinococcosis reveals a cyst with a distinct wall and a very thin echo-negative rim around it. The daughter hydatids are internally defined as small echo-positive floating formations. The capsule of an old hydatid cyst may become calcified. (They try to explain the most common localization of echinococcus in the liver by the discrepancy between the size of the parasite and the diameter of the vessels, presenting the liver as a sieve. In fact, echinococcus is selectively fixed in the liver because its capsule is built of five-membered sugars, and the pentose cycle is most intense in the liver, i.e. e. Echinococcus is fixed where there are optimal conditions for its development. And the fact that the pentose cycle occurs most intensely in the liver also has great biological meaning: the liver, being perhaps the main depot of glycogen (built from six-membered sugars, competes with it only muscles), provides its energy metabolism with five-membered sugars, without wasting carbohydrates consumed by other organs. In the same way, the erythrocyte, which carries oxygen, itself lives due to anaerobic metabolism. The platelet, whose task is to die at the right moment, is not a living cell, but only a fragment of a cell. There are many such examples. And if after all this seemingly narrow medical knowledge we do not come to the idea of a higher expediency, then how will we hear the voice if we do not want to hear it.)
Liver hematoma
should be excluded for any injury, especially abdominal and automobile trauma. In cases of recent trauma, the hematoma appears as a solid echogenic formation. Gradually, due to necrosis, a pseudocyst is formed.
Liver hemangioma
- the most common benign tumor-like formation of the liver. A small hemangioma, due to the many small cysts and septa that create the effect of sound reflection, looks like an echogenic formation (Fig. 3). With large hemangiomas, episodes of thrombosis are possible with a deficiency of platelets in the periphery and a tendency to hemorrhage.
Rice. 3.
Hemangioma of the liver.
Mesenchymal hamartoma
usually detected in children during the first 2 years of life and debuts as a painless formation in the abdominal cavity. It accounts for 7-8% of all liver tumors in children. Hamartoma arises from the mesenchyme of the periportal tract; inside the tumor, hepatocytes, components of the bile ducts, blood vessels, and mesenchyme are found, but without lymphatic tissue. Due to the accumulation of fluid in the mesenchyme, cysts arise. The different ratio of tissue and cysts led to the identification of two types of hamartoma: predominantly stromal and predominantly cystic. The echographic picture of mesenchymal hamartoma is extremely variable. The hamartoma is well demarcated from the liver tissue, usually located in the right lobe, large in size, and contains many septal cysts.
Liver adenomas
are rare in children. They occur in children with glycogenosis (especially type I), glucose-6-phosphatase deficiency, galactosemia, Fanconi anemia, aplastic anemia (in the latter case, treated with androgens). Echographically, a solitary hypoechoic formation is recorded, in some cases it is isoechoic.
Focal nodular hypertrophy
- primary liver tumor without capsule. It is a hyperplastically regenerating node of hepatocytes, Kupffer cells, separated by fibrous cords. Characteristic of focal nodular hypertrophy is the presence of a central stellate field (scar) with proliferating bile ducts and blood vessels radiating from it. Focal nodular hypertrophy is more often detected in women, but can also be found in children of any age. Estrogens accelerate the growth of education. Echographically, the tumor is detected accidentally, looks like a well-circumscribed formation, which can be hyperechoic or isoechoic to varying degrees. In 50% of cases a halo is recorded. The formation may be located on a stalk at the edge of the liver.
Intrahepatic calcifications
are rare (Fig. 4). They are typical for an infectious process, especially granulomatous (tuberculosis, brucellosis, histoplasmosis, coccidioidomycosis), cytomegaloviruses, toxoplasma, pneumocystis, hydatid disease, hemangioma, hemangioendothelioma, malignant tumors (calcifications of the radial ray type are characteristic of hepatoblastoma), trauma, vascular calcification, disease Caroli.
Rice. 4.
Calcification in the liver parenchyma with a typical acoustic shadow phenomenon.
Malignant liver tumors
occupy 3rd place in prevalence after Wilms tumor and neuroblastoma. They account for 5% of all childhood malignant tumors. 65-70% of liver tumors in children are malignant. All liver tumors manifest as mass formations in the abdominal cavity. The role of echography is to clarify the localization of the formation, provide data for a preliminary diagnosis and create conditions for the next stages of diagnosis (MRI, angiography, etc.).
Hepatoblastoma
- the most common liver tumor. It accounts for 47-50% of all childhood malignant liver tumors. Originates from fetal hepatocytes. The average age of patients at the time of diagnosis is 18 months (range of fluctuations is from 0 to 3 years). Girls get sick more often. It manifests with an enlarged abdomen, hepatomegaly, and often with symptoms of an acute abdomen. Possible osteopenia with bone fractures, hypoglycemia, hypercholesterolemia. In 90% of cases, the level of α-fetoprotein is elevated. Echographically, the tumor looks like a fairly clearly limited formation, often massive. Inside the tumor there may be foci of calcification and necrosis. According to Doppler ultrasound, the tumor is well vascularized. Hepatoblastoma quickly grows into the hepatic artery, inferior vena cava or covers them in the form of a dense coupling (Fig. 5, a, b).
Rice. 5.
Echogram of a liver tumor in normal mode and in MRI reconstruction mode.
A)
Echogram of a liver tumor in normal mode. The tumor is not visualized clearly enough.
b)
Echogram of a liver tumor in MRI mode. The structure of the tumor and its boundaries are visible quite clearly.
Hepatocellular carcinoma
in children, histologically it is completely similar to that in adults. Tumor cells are histologically very similar to normal hepatocytes, which makes diagnosis difficult. Affects children aged 10-12 years. It accounts for 20% of all malignant liver tumors in children. Predisposing factors are biliary atresia, familial cholestasis, hepatitis B, obesity, glycogenosis type I, hereditary tyrosinemia. Manifests with hepatomegaly, jaundice, anorexia, and a significant increase in the level of α-fetoprotein. Echographically, the tumor can be hypo- or isoechoic, multifocal, solitary (giant in size), diffuse (affecting the entire liver). Sometimes a thin echo-negative rim-halo is recorded around the tumor, which is an echographic reflection of the capsule. Central tumor necrosis with the formation of false cysts is possible.
Undifferentiated embryonal sarcoma (malignant mesenchymoma)
is a rare tumor consisting of undifferentiated spindle cells and mainly affects adolescents. It accounts for 5% of all malignant liver tumors in children. It manifests itself, like all liver tumors, with a mass formation in the abdominal cavity, fever, exhaustion, while the concentration of α-fetoprotein does not change. Echographically, the tumor can be presented as either solid masses with dense calcifications and the phenomenon of acoustic shadowing, or cystic formations with multiple internal septa. These pseudocystic cavities are formed due to hemorrhages and necrosis. Angiography confirms hypervascularization of the tumor.
Metastases.
The liver, as a result of the complexities of its blood supply, is more predisposed to the appearance of metastases in it than any other organ. Tumor cells are usually introduced with the bloodstream through the portal system (for example, from intestinal tumors), through the hepatic artery (tumors of the lungs or breast), and through the lymphatic system. Less commonly, metastasis occurs along the peritoneal surface (ovarian cancer). In the latter case, the initial metastasis is localized subserosally. In contrast, with hematogenous metastasis, the foci are located centrally. Small peripheral lesions are difficult to detect echographically, as they may be hidden by a rib shadow or near-field artifact. Metastases can be hyper-, hypoechoic (lymphoma metastases are the most hypoechoic, they are multiple, very tender), isogenic, heterogeneous (due to necrosis or hemorrhages). But it is impossible to talk about the origin of metastases based on their acoustic properties according to ultrasound data. The stage of the disease should be clarified using MRI or CT.
Metastases on ultrasound are usually solid, the edges are not clearly defined. Large metastases may contain fluid (necrosis) or mucin in the center (ovarian cancer metastasis). As a result of chemotherapy, calcifications may appear in the metastasis. In cases of changes in the texture of the liver (expansion of intrahepatic bile ducts, consequences of chemotherapy, cirrhosis as an outcome of hepatitis), identifying metastases is very difficult. According to Doppler ultrasound of the vessels, there are no metastases inside. In large metastases, rare small vessels may appear along the periphery. In the presence of ascites in advanced stages of cancer, it is possible to detect metastases on the surface of the omentum or peritoneum.
Conclusion
Ultrasound is used to diagnose and monitor liver diseases, as well as in treatment using invasive ultrasound-guided procedures. At the same time, it should be remembered that the liver changes with the pathology of many other organs, for example, with kidney diseases, and it is impossible to establish the causes of changes in the morphology and function of the liver without a thorough systemic analysis. To do this, along with examining the gallbladder and pancreas, do not forget to scan the retroperitoneal, subdiaphragmatic spaces and the small pelvis. If you do not work next to the device as a doctor, then even with the most golden stars on your shoulder straps, you will not rise above a paramedic.
SonoAce Ultrasound Magazine
Contains current clinical information on ultrasonography and is aimed at ultrasound doctors, published since 1996.
What do deviations from the norm mean?
The value of this analysis lies in the fact that it helps to prove or disprove the presence of injuries to the organ itself, the appearance of neoplasms, inflammatory processes, anomalies/pathologies of organ development.
Deviations from the norm in the size of the spleen in adults:
- the presence of fluid in the abdominal cavity, unclear contours of the organ indicate damage, rupture of the spleen tissue;
- the organ is enlarged in size, during examination it appears light, with a homogeneous structure - an inflammatory process, splenitis;
- the presence of spots in the structure of the spleen - the inflammatory process ended with necrosis of the internal tissue;
- uneven contour, uneven echogenicity of the organ - a sign of hematoma;
- thickening/thinning of organ tissue – splenic infarction;
- hypoechoic structure of the organ - inflammation of the organ;
- the size of the organ is larger than normal, convex contours, a pointed edge, increased parenchyma density, enlarged lymph nodes in the area of the organ's hilum - leukemic infiltration.
Here is only a small part of the information that is given when deciphering an ultrasound of the spleen. Only an experienced specialist can give an accurate explanation of the analysis, catch all the smallest changes in the structure of the organ, and determine this or that disease.
Where is the organ located and what are its functions?
The spleen has a flat oval shape. The organ lies at the top of the peritoneum on the left, next to the pancreas and the left kidney behind the stomach. Twenty percent of people have an extra lobe. It is not always located next to the main organ. Statistics are known when it was in the scrotum. Rare cases of structural features have been described in which this organ was completely absent (asplenia). This is not a deviation from the norm, especially since the anomaly does not manifest itself in any way. It happened that when the main lobe was completely removed, an additional lobule took over its functions and grew larger.
During the growth of the fetus in the womb, the spleen works for hematopoiesis, and after the birth of the child, it stops. The adult spleen is a filter that absorbs bacteria, diseased red cells and other pathological particles. The organ produces bodies that increase the body's resistance to infections. It accumulates iron needed for hemoglobin. If the body needs additional blood, the spleen has a reserve.
Preparation for ultrasound of the spleen
The main task of the preparatory stage is to prevent excessive formation of gases. If this is not done, the loaded bowel will make examination difficult. For this purpose, you should stick to a diet for three days before the session. You will need to exclude from the diet:
- legumes, peas;
- sweets;
- fresh white bread;
- vegetables that have not undergone heat treatment.
You should stop eating 9 hours before the procedure. Doctors recommend taking enterosorbents (Filtrum, Smecta) in the evening to neutralize gases. The study is carried out on an empty stomach, with the exception of diabetics.
List of indications for the procedure
An ultrasound is done when a number of abnormalities are detected, the main one of which is splenomegaly. In a healthy state, the organ is located under the arch of the ribs on the left and does not protrude from under them. The diseased organ is enlarged and can be felt behind the costal margin. The procedure is determined by the following goals and conditions:
- determination of organ size, developmental anomalies;
- detection of neoplasms;
- pain in the lower back, side, left side of the back, shoulder blade;
- nausea;
- pressure drop;
- liver diseases (cirrhosis, hepatitis and others).
Particular attention is paid to injured patients with diseases of the blood and lymph nodes. Trauma can disrupt the integrity of the organ, while its capsule remains intact. The membrane stops bleeding and then bursts. Internal bleeding begins, which threatens the patient with many complications. Cancer patients are subject to mandatory examination, since scanning reveals the location of the tumor, metastases, and enlarged lymph nodes. Monitoring of the condition of the described area is indicated for severe infectious diseases: sepsis, tuberculosis, typhoid fever.
Prevention
Diseases of other organs can provoke inflammation of this one. If during a cold there is pain under the rib on the left side, this is a distress signal from the spleen. That is, it is exhausted and cannot cope with its functions in the body.
Liver diseases, viral diseases, tuberculosis can be the culprits of a diseased spleen. In this case, you should fight the underlying disease that weakens this organ. In some cases, the cause of pain in the spleen may be the presence of parasites in it - echinococcus. If timely treatment is not started, a cyst may form in the organ, and in severe cases, tissue rupture may occur.
In the case when spleen tissue ruptures, it is possible to save the organ in rare cases, in 1% out of 100. To avoid such situations, to prevent rupture:
- heavy physical activity is contraindicated;
- it is necessary to comply with bed rest for acute respiratory infections, acute respiratory viral infections;
- you need to avoid stressful and emergency situations on the roads;
- Do not lift heavy things;
- Pregnant women are advised to wear a bandage to avoid injury to the spleen.
Even if the spleen does not cause concern, regular examination of the abdominal organs once a year will not be superfluous. This way you can protect yourself from late diagnosis of any ailments.