What is being studied?
The object of study of the lipid spectrum in medicine is the following indicators: total cholesterol or cholesterol, triglycerides, lipoproteins of various densities.
Total cholesterol (cholesterol)
This indicator is basic in assessing lipid metabolism and, in addition to the lipid profile, is also checked during a routine biochemical blood test. Total cholesterol (TC) or cholesterol (CS) is a component that is part of the cell membrane and is responsible for its structural and strength properties.
In addition, it is involved in digestion and plays a key role in metabolic processes and hormone synthesis. Cholesterol enters the body through food products exclusively of animal origin, or is produced by the body itself, mostly in the liver.
In blood plasma, this substance is in a free state or combined with complex proteins (lipoproteins). Depending on the density of fats contained in these proteins, separate types of lipoprotein fractions are distinguished.
High density lipoproteins
High-density lipoproteins (HDL) have the ability to bind “bad” cholesterol, removing it from the general bloodstream and transporting it to liver cells for subsequent excretion in bile. The action of HDL is called antiatherogenic because they prevent the formation of atherosclerotic “plaques”.
The normal value of this indicator indicates that HDL performs its useful function - it protects blood vessels from being blocked by “bad” cholesterol and reduces the risk of developing lipid metabolism disorders.
Low density lipoproteins
Low-density lipoproteins (LDL or LDL) consist of 70% cholesterol and perform the function of transporting it. Their unfavorable effect lies in their ability to penetrate the walls of vessels of any diameter due to their small size.
By changing the structure of the vessel wall, they interfere with normal blood flow. Elevated LDL levels indicate a high likelihood of atherogenic arterial damage and lipid imbalance, while total cholesterol may remain normal.
There is another lipid profile indicator that is used to interpret the results - very low density lipoproteins (VLDL). This type of lipoprotein mainly consists of triglycerides, their function is to transport fat particles to the peripheral organs of the immune system. They have an atherogenic effect, as they promote the deposition of lipids on the inside of the vascular wall.
Triglycerides
Triglycerides (TG) come from foods containing large amounts of animal fat. They are the main energy storage for cells and are mostly localized in fatty tissue. Despite their energy function, an increase in TG adversely affects the activity of the heart and blood vessels.
The amount of incoming TG must be completely spent on energy production, otherwise their excess accumulates in adipose tissue or is involved in the production of additional cholesterol.
Atherogenic coefficient
The atherogenic coefficient (AC) is calculated based on the obtained values for the main parameters of the lipid profile. The formula for its calculation is as follows: KA = (X – HDL)/LDL.
The value of the coefficient (normally 3-3.5) represents the ratio of atherogenic to non-atherogenic fractions. Its growth indicates an imbalance in fat metabolism. The higher the KA value, the higher the risk of pathological changes caused by atherosclerotic damage to blood and lymphatic vessels.
Reasons for the downgrade
A drop in level indicates several possible violations.
- Malignant processes. Tumors of any location. Mainly when located in the digestive tract and organs of the reproductive system. Kidneys.
- Starvation. A long-term lack of adequate nutrition leads to an understandable result. Lipids simply do not enter the body in sufficient quantities. If there is a fat layer, this phenomenon can be delayed.
- Infectious lesions. Up to sepsis.
- High concentration of thyroid hormones. Accompanied by poisoning of one's own systems.
- Pulmonary diseases of different types.
- Burns. The larger the affected area, the more significant the problem.
A blood test for the lipid spectrum shows changes in organs and systems indirectly; in any case, auxiliary techniques will be required for clarification.
How to prepare?
The results of a lipid profile will be reliable if the influence of external factors is minimized.
When preparing for analysis, there are a number of mandatory restrictions that should not be neglected:
- 24 hours before the test, it is forbidden to consume fatty foods and alcoholic drinks, and 4 hours before the test, refrain from smoking. The last meal is allowed at least 12 hours before the procedure. Drinking clean water is allowed.
- The day before the test, limit physical activity and emotional stress; during the procedure, also try not to be nervous and relax.
- If you feel physically and emotionally tired, reschedule the procedure a couple of days ahead.
- You should not adhere to a special lean diet before the examination; eat as you are used to.
- It is not recommended to take the test after radiography, rectoscopy (examination of the rectum), or physical therapy. In this case, you should postpone the examination for several weeks. Data will be unreliable for three months after a heart attack, injury or surgery.
- Be sure to tell your nurse and doctor about the medications you are taking, as some may significantly affect your results.
The results of the lipid profile will be different during pregnancy, in acute infectious diseases, chronic pathologies of the urinary system, and diseases of the endocrine glands.
How is the analysis itself carried out?
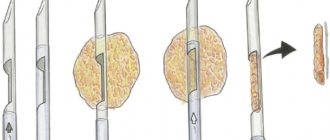
The patient's venous blood is used for analysis. Blood donation takes place in the morning, on an empty stomach. The resulting serum is subjected to a centrifugation procedure, after which it is sent to the laboratory for detailed study.
Studying the biomaterial and preparing a conclusion takes no more than 24 hours. There is a special device - an express lipid profile (status) analyzer, with which you can carry out a shortened diagnosis in just 5 minutes.
For persons with a confirmed diagnosis of atherosclerosis, doctors recommend examining the lipid spectrum of the blood every six months.
The role of lipids
Lipids are found in all cells of the human body. They are insoluble in water. Some of these substances constantly circulate in the blood; therefore, they are of great importance for medicine and are combined into the general concept of “blood lipid profile”.
Functions of lipids:
- Structural. Glycolipids, phospholipids, cholesterol are the most important components of cell membranes.
- Thermal insulation and protective. Excess fat is deposited in subcutaneous fat, reducing heat loss and protecting internal organs. If necessary, the lipid supply is used by the body to obtain energy and simple compounds.
- Regulatory. Cholesterol is necessary for the synthesis of adrenal steroid hormones, sex hormones, vitamin D, bile acids, is part of the myelin sheaths of the brain, and is needed for the normal functioning of serotonin receptors.
Tables of normal indicators
The following data is considered to be the general norms for an adult:
| Parameter designation | Norm |
| X (cholesterol) | 3.4 - 5.6 mmol/l |
| HDL (high density lipoprotein) | 1.03 - 1.55 mmol/l (not less than 1 mmol/l) |
| LDL (low density lipoprotein) | 1.71 - 3.37 mmol/l |
| TG (triglycerides) | up to 2.25 mmol/l |
| KA (atherogenic coefficient) | 2,2 — 3,5 |
It is important to remember that reference values will depend on the technical equipment of the laboratory. Minor deviations of the results from generally established standards are allowed.
In adult women and men
| Lipidogram indicator | Age, number of years | Norm, mmol/l | |
| Men | Women | ||
| Total cholesterol (cholesterol) | Up to 65 | 2,8 — 5,9 | |
| Over 65 | 3,6 — 7,1 | ||
| HDL | Up to 40 | 0,88 — 2,12 | |
| 40-60 | 0,72 — 1,84 | 0,96 — 2,35 | |
| Over 60 | 0,98 — 1,94 | 0,98 — 2,48 | |
| LDL | Up to 40 | 1,71 — 4,45 | 1,94 — 4,45 |
| 40 — 60 | 2,25 — 5,26 | 2,31 — 5,44 | |
| Over 60 | 2,15 — 5,44 | 2,59 — 5,8 | |
| Triglycerides | 20 — 40 | 1,7 — 2,25 | |
When deciphering the results of a lipid profile, you should pay attention to the person’s age. During reproductive age, HDL levels in women will be higher than in men. Consequently, the risk of developing atherosclerosis for women in this age period is minimal.
After the onset of menopause, hormonal changes occur in a woman’s body, as a result of which the level of cholesterol increases and the risk of atherosclerotic vascular damage significantly increases.
In children
Value standards for children will differ from those established for adults.
| Lipidogram indicator | Child's age | Norm, mmol/l |
| Total cholesterol (cholesterol) | First month of life | 1,3 — 4,4 |
| From 2 months to a year | 1,5 — 4,9 | |
| From 1 year to 14 years | 2,8 — 5,2 | |
| HDL | Up to 14 years old | 0,9 — 1,9 |
| LDL | 1,6 — 3,6 | |
| Triglycerides | 0,3 — 1,4 |
Increased cholesterol levels in children under 14 years of age are less common than in adolescence, young adulthood, or adulthood. However, in cases where a child has constantly high cholesterol and has a family history (close relatives of the child are diagnosed with hypercholesterolemia, coronary atherosclerosis, heart attack, stroke, etc.), a lipid profile is required.
It should be taken into account that until the age of two, this analysis is not informative, because At this time, there is an active process of formation and growth of tissues that need large amounts of fats absorbed from food.
During pregnancy
During pregnancy, changes occur in hormonal metabolism: on the one hand, sex hormones are intensively produced in a woman’s body, on the other hand, the production of the enzyme responsible for the breakdown of fats and their processing decreases.
This leads to an increase in cholesterol and LDL, their concentration during this period increases by 1.5-2 times. At the same time, the level of HDL is the same as the values established as the norm for non-pregnant women, and virtually does not change throughout the entire pregnancy.
The standards established for pregnant women include the following values:
- the level of total cholesterol should not exceed 6.5 mmol/l;
- the LDL norm is 1.9 - 5.5 mmol/l;
- HDL norm is 0.8 - 2.1 mmol/l;
- TG norm is 1.7 - 2.7 5 mmol/l.
Decoding the results
The results of a lipid profile should only be deciphered together with a doctor, since any deviations in its values from the norm are signs of possible disorders.
Increased performance
An elevated level of total cholesterol or hypercholesterolemia most often indicates a high risk of developing atherosclerosis in a patient. The reasons for this may be external or internal.
External reasons:
- excess fatty foods in the diet;
- obesity caused by low mobility, lack of physical activity;
- bad habits.
Since a large proportion of cholesterol is produced by internal organs, and only a fifth comes with food, an increase in its content may be due to internal reasons: hereditary diseases, age-related changes, acquired pathologies (diabetes mellitus, renal failure, thyroid diseases, cholestasis, hepatitis and cirrhosis of the liver, pancreatic diseases and others). In case of dysfunction of the pancreas, intestines, pathologies of the liver and gallbladder, a stool lipid profile is additionally indicated.
A pathological increase in HDL levels above 2.2 mmol/l, despite their positive role in the regulation of fat metabolism, can be caused by genetic pathologies of lipid metabolism, intestinal oncology, and severe physical activity. In other cases, moderately elevated HDL levels indicate a low risk of developing vascular diseases.
High values of LDL and triglycerides, related to the upper limit of normal, warn of a high risk of atherosclerotic vascular damage. While a pronounced excess of the norm indicates an existing cardiovascular disease - atherosclerosis of the cerebral and peripheral arteries.
Triglyceride concentrations may also increase for the following reasons:
- coronary heart disease (CHD), myocardial infarction, arterial hypertension;
- increased calcium levels;
- diabetes;
- obesity;
- chronic alcoholism;
- thrombosis of cerebral arteries;
- viral hepatitis;
- nephrotic syndrome.
The atherogenicity coefficient shows the general picture of the state of fat metabolism. If the key elements of the lipid profile are elevated, its level will be 3-4 units; a significant excess of the norm - 5 or higher - requires medical supervision and corrective measures, as it indicates the progression of serious pathologies, such as:
- atheromatosis and calcification (advanced forms of atherosclerosis);
- ischemia of the heart and internal organs;
- multifocal or diffuse brain damage;
- kidney diseases;
- circulatory disorders in the extremities.
Decreased performance
Hypocholesterolemia (lower cholesterol) is caused by fasting, following a lipid-lowering diet, or diseases such as:
- arthritis (rheumatoid form);
- increased thyroid function;
- infectious lesions of a generalized nature;
- malignant anemia;
- impaired absorption capacity of the small intestine;
- extensive burns (burn disease);
- heart failure.
A decrease in HDL concentration is a harbinger of atherosclerotic vascular damage. The cause of this may be infections of bacterial or viral etiology, endocrine pathologies, kidney and liver diseases, hepatic encephalopathy, hereditary disorders of lipoprotein metabolism.
A decrease in atherogenic lipoprotein fractions below normal limits is extremely rare. If all other indicators of the lipid profile are normal, then a moderate decrease in LDL has a positive effect on the condition of blood vessels and indicates that there is no risk of developing heart disease.
A decrease in triglycerides is observed in autoimmune neuromuscular disorders, chronic pulmonary obstruction, ischemic stroke, pathologies of the endocrine system, and the use of certain medications (for example, progestins, heparin, vitamin C and others).
Let's sum it up
A lipidogram is a popular method for diagnosing many diseases of the cardiovascular system; for example, cardiologists are able to fairly accurately assess the risk of a heart attack or other diseases that appear due to high levels of “bad” cholesterol.
The specialist should classify you as a risk group; the frequency of subsequent preventive lipidograms depends on this!
Here are common diseases that can be avoided if this analysis is carried out in a timely manner:
- Stroke;
- Liver diseases;
- Heart attack;
- Kidney diseases;
- Atherosclerosis.
These diseases can be prevented without any problems if you are careful about your health.
Who is most susceptible to high cholesterol?
Elevated cholesterol levels are caused by the following factors:
- Lifestyle;
- nutrition;
- age;
- heredity;
- diseases.
The relevance of this problem does not lose its importance among people who lead a sedentary lifestyle, are overweight and have an unhealthy diet. Foods containing large amounts of animal fats contribute to the growth of cholesterol. These products include: egg yolk, butter, margarine, mayonnaise, lard, sausages, offal - liver, brains, kidneys. Smoking and drinking alcoholic beverages also have an adverse effect on the structure of the vascular walls, thinning them and promoting the formation of atherosclerotic deposits.
With age, metabolism slows down, which leads to a decrease in the rate of elimination of fat metabolism products and the deposition of cholesterol particles on the walls of blood vessels.
Elevated cholesterol levels are characteristic of some hereditary and acquired diseases, such as:
- hereditary hyperlipidemia;
- diabetes;
- rheumatoid arthritis;
- renal failure;
- gout;
- changes in the pancreas leading to pancreatitis, etc.
For what pathologies is it prescribed?
Biochemistry of an extended analysis for cholesterol with a lipid profile is prescribed for diagnosis or control of treatment of such pathologies:
- Cardiac angina and myocardial infarction;
- In the post-infarction period;
- Systemic atherosclerosis;
- For jaundice that does not have a hepatic etiology;
- Failure of kidney organ cells;
- Pancreatic oncology;
- Pathology glomerulonephritis;
- For diabetes mellitus;
- Pathology pancreatitis;
- Disturbances in the functionality of the thyroid gland - hypo or hyperthyroidism;
- Excess body weight;
- Chronic stage of alcoholism;
- Weight loss - anorexia;
- Gouty disease;
- Burns over a large area of skin;
- Disturbance in hematopoiesis - megaloblastic anemia;
- Myeloma disease;
- Taking contraceptives for a long time;
- Infectious sepsis.
Taking contraceptives for a long time