The radiographic research method was originally used to study the musculoskeletal system. It allows you to obtain data on the structure and functioning of bones and joints during a person’s life. X-rays of joints and bones are the main way to study them in normal and pathological conditions. It allows, for example, to detect early changes in the endplates of the epiphysis, or in the subchondral layer of bones, which is important when studying dystrophic changes in joints, which occur quite often.
Doctors examining an x-ray
Features of X-ray anatomy of the skeleton
The radiographic picture of the skeleton is not unchanged. It is dynamic and depends on the gender and age of a person, his anatomical features and state of health. Thus, in newborns, the bones do not have ossification nuclei at their ends, and the articular surfaces consist of cartilage, which is not visible on x-rays. This makes their joint spaces appear to be very wide.
Pathological changes that occur in the musculoskeletal system in various diseases are extremely polymorphic, which makes the radiological signs of diseases very diverse. The same diseases, depending on their stage and individual characteristics of the patient, cause different symptoms, and pathologies that are quite distant from each other, on the contrary, sometimes have very similar symptoms.
Therefore, the assessment of radiographs should be carried out only taking into account the clinical picture of the disease and the patient’s anamnestic data.
Description of radiographs for arthrosis
Radiography makes it easy to detect arthrosis, and modern digital radiography machines can detect it in the initial stages. However, in some cases, magnetic resonance or computed tomography may be additionally performed to clarify some of the nuances of the disease.
Arthrosis looks different on an x-ray, depending on the duration of its course and the area of the lesion. To complete the picture, several x-rays in different projections are often required.
Is arthrosis visible on an x-ray, and how often is this method used?
X-ray diagnostics allows in most cases to easily determine the presence of arthrosis of various joints in a patient. If the severity of the disease is small, then x-rays can reveal it by indirect signs.
X-ray procedures are the standard for primary diagnosis of patients with suspected arthrosis. X-rays can be used to identify the disease in its early stages. Although initially, when the disease has not yet developed strongly enough, mistakes are possible. In this case, it is better to use computed tomography.
The procedure is suitable for visualizing different groups of joints, including the spine. The joints of the knee, hand, foot and hip area are best visualized.
Osteoarthritis of the finger joints on x-ray
Arthrosis is shown both by a modern digital X-ray machine and an old one (still Soviet-made). If possible, it is recommended to undergo the examination on new equipment.
How accurate is x-ray diagnostics and how does it show arthrosis?
X-ray diagnostics currently remains the simplest and most accessible (it is carried out in every clinic) method of examining patients with arthrosis.
It visualizes the disease quite informatively and allows one to determine its location and extent. This is a frequently used method for diagnosis in patients who first consult a doctor with relevant complaints.
It can be performed on patients of any age group, regardless of health status.
X-rays should be considered in the diagnosis of arthrosis as a method of surgical examination. X-rays can reveal the disease both by indirect and direct signs. For example, indirect signs include specific types of inflammatory processes in joint tissue. This will appear as a shadow in the photo.
Often the image shows osteophytes and osteosclerosis, which are compaction of bone tissue or proliferation of bone tissue. These defects are characteristic of arthrosis even at the initial stages (although in rare cases they can be a consequence of other diseases).
To better visualize the hip joints specifically, the patient undergoes separate radiography (this is only necessary for examining the hip joint). The problem is that this method increases ionizing radiation on the patient’s body.
radiography only as part of primary diagnosis : CT is used to identify more precise nuances of the disease. X-rays are also good as part of dynamic observation (monitoring) of the course of the disease during its aggressive treatment.
What forms of arthrosis can be seen in the picture?
Usually the disease is easily identified. It is possible to identify age-related, traumatic, infectious and autoimmune subtypes of arthrosis. Arthrosis caused by damage from chemical toxins, inflammatory processes, and metabolic disorders in the patient’s body is clearly visible.
Osteoarthritis of the knee joints on an x-ray
In some cases, even banal age-related arthrosis may be missed in the image. This happens rarely, and is usually because the disease is in the early stages.
How to determine arthrosis from an image?
In the initial stages, the disease is usually detected by indirect signs:
- Moderate narrowing of the gap of the examined joint.
- The presence of pinpoint calcifications on the outer edge of the acetabular cap (in the case of diagnosing hip joints).
- Moderate subchondral osteosclerosis.
- Sharpening of the edges of the fossa of the femoral head (in the case of diagnosing hip joints).
Signs visible on an x-ray of advanced arthrosis:
- significant narrowing of the joint space;
- severe subchondral osteosclerosis;
- compaction of bone tissue;
- presence of subluxation;
- sometimes free intra-articular bodies are noticeable (relevant only for diagnosing coxarthrosis);
- reduction in the volume of the articular surface with its flattening;
- aseptic necrosis processes in the femoral head (during the diagnosis of hip joints);
- the presence of various forms of osteophytes located along the edges of the articular surfaces;
- significant deepening of the acetabulum (when diagnosing hip joints).
How and where to take an x-ray for arthrosis?
The X-ray diagnostic procedure for suspected arthrosis is carried out in the same way as for any other disease or injury. That is, a regular x-ray is taken.
The only caveat: if you suspect arthrosis of the hip joints, it is better to use mobile X-ray devices. This is necessary so that the patient remains in the most comfortable position for him during the examination: this way the pathological focus can be better examined.
Osteoarthritis of the knees on digital radiography
The procedure can be performed both in a public medical institution and in a private one. There is not much difference, but it is recommended to look for a clinic that performs digital x-ray diagnostics. Old X-ray machines can also visualize arthrosis, but with much worse information and accuracy.
How much does a photo cost?
The cost varies depending on the group of joints examined. The differences in cost for different groups of joints are not very large, but they still exist.
Source: https://kostromskoj-kraj.ru/opisanie-rentgenogrammy-pri-artroze/
Methodology for conducting X-ray examination of the musculoskeletal system
Radiation examination of bones and joints should be carried out as prescribed by the attending physician. Indications for it include almost all injuries of the musculoskeletal system. Also, radiography should be performed if systemic diseases are suspected, especially with an autoimmune component.
Positioning of the patient depends on the area of study
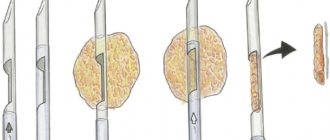
The basis of the diagnostic search is radiography of bones and joints, performed in two projections perpendicular to each other. The correct image should show the entire bone and adjacent joints, or a joint and adjacent sections of two bones, if the purpose of the shooting was to diagnose articular pathology.
What protective mechanisms are activated during deforming gonarthrosis?
When the elasticity of the cartilage tissue of the joint decreases, the load is redistributed in the adjacent areas of the bone. The following changes are observed:
- bone tissue is replaced by connective tissue, which cannot perform a supporting function;
- the curvature of the articular surfaces of the bones is rebuilt;
- osteochondral growths are formed.
The above changes are compensation aimed at reducing the load on the articular cartilage.
However, the higher the degree of compensatory response of the body, the lower the amount of motor ability in the knee.
Features of the use of radiographs in the diagnosis of joint diseases
If such images cannot clearly identify pathological changes or damage, then additional images are taken in oblique projections, targeted images. It is possible to use additional diagnostic methods - linear tomography, computed tomography, magnetic resonance imaging.
In the event of injury, all patients who do not have life-threatening injuries and are conscious are subject to X-ray examination in the radiology room. Otherwise, mobile X-ray units are used.
How often can X-ray diagnostics be done?
With classical radiography, the radiation dose is 30% of the maximum permissible radiation dose per year. As a rule, doctors do not recommend taking x-rays more often than 2 times a year. The exception is when the digital X-ray scanning method is used. When using modern devices, the radiation dose is usually 10 times less, which makes it possible to take x-rays 3-5 times a year.
Doctors also advise against using an X-ray machine if the diagnosis can be made using less harmful tests. If the pathology of the joint is obvious, then a computed tomography or ultrasound examination may be sufficient to clarify the diagnosis.
Main symptoms of joint pathology
The main sign of joint damage on an x-ray is considered to be a narrowing of the joint space. If it is uniform, then most likely there is a degenerative condition of the joint cartilage. Uneven narrowing of the joint spaces is a sign of a variety of arthritis, and occurs due to the destruction of the subchondral parts of the bone and the end plates of the epiphyses.
Ankylosis of the left knee joint
With fibrous ankylosis, on the contrary, the end plates completely disappear, and with the bone form of ankylosis, the transition of the bone beams from one epiphysis to another is visualized. In case of injury, joint dislocations often occur. Their x-ray picture is quite recognizable - the images reveal a displacement of the head of one of the bones, which is absent in the glenoid cavity. This condition is called complete mismatch of the articular ends of the bones. Here it is important to monitor whether the dislocation is complicated by the separation of bone fragments from the articular ends.
These fragments can prevent the bone from moving back normally. In addition, there is a possibility of subluxation. It is diagnosed when there is partial discrepancy between the articular surfaces. An additional sign is a wedge-shaped joint space.
Principles of treatment
At the moment when the articular surfaces have not yet undergone fatal changes, but only minor degenerations, conservative treatment is applied. It is based on the following principles:
- physical therapy exercises without absolute vertical load - the doctor will prescribe the correct (!) set of trainings, which will improve metabolic processes in the joint and make it possible to stop pathological progression;
- losing weight through diet - losing weight is very important for overweight and obese people, because extra pounds put pressure on the joint, making it difficult to function normally;
- exclusion of physical activity , in which the bone joint functions in an enhanced impact mode (running, team sports, jumping, etc.);
- the use of non-steroidal anti-inflammatory drugs to relieve pain and swelling (Ibuprofen, Diclofenac, Voltaren, Indomethacin, etc.);
- the use of drugs to stimulate the production of synovial fluid and replenish osteochondral components with useful substances (chondroprotectors, hyaluronic acid);
- wearing special orthotic devices, orthopedic shoes;
- prescription of physiotherapeutic procedures (cryotherapy, ozokerite and paraffin applications, UHF, ultrasound, phonophoresis, etc.).
There are no statistics confirming that overweight people have more joint problems. But common sense has not been canceled, there is a big difference when you have 65 kg on your knees. or 110...
If the disease is characterized by a severe course or the conservative approach does not give positive dynamics, there is a need for surgery. Today, orthopedic surgeons carry out unique interventions (stage 2-4), in which the diseased knee joint or a separate part of it is replaced with an endoprosthesis, a biocompatible artificial analogue of a biological joint. We invite you to familiarize yourself with our videos and photos, which perfectly demonstrate the features of the procedure and its benefits.
Attention! It is impossible to cure this disease conservatively. Serious destruction cannot be corrected either by popular intra-articular injections or even by stem cell transplantation. Therefore, do not hope that newfangled minimally invasive and non-invasive techniques will magically help restore damaged hyaline cartilage, which, due to physiological characteristics, is not capable of regeneration. Alternative and official conservative medicine can only slow down unfavorable pathogenesis, and even then mainly only in the early phase of its development.
Endoprosthetics is the only orthopedic method that can relieve the patient from hellish pain and disability caused by gonarthrosis. There is currently no alternative to it! Replacement of the knee joint with a durable implant is carried out in the surgical department of orthopedics at a specialized clinic. Let us draw your attention: in order to achieve the most complete recovery after knee replacement, you should definitely undergo a special course of a rehabilitation treatment program.
With correctly performed implantation surgery and impeccable rehabilitation (it lasts on average 3-4 months), a person returns to a full life. Of course, he will need to follow simple rules so that the new knee joint can function without problems for at least 15 years. What is most remarkable is that 15 years is not the limit. Modern endoprosthetic knee designs, as shown by clinical observations of patients who have undergone this operation, in most cases last 20-25 years.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Bone changes that occur in joint pathology
In the case of destructive joint diseases, radiographic images reveal foci of destruction of bones and periarticular tissues. They look like small lesions in the places of attachment of the joint capsule and its ligaments to the bony surfaces of the epiphyses. In this case, the articular contours become uneven, in some places they become thinner, and sometimes they become sclerotic, forming a characteristic “motley” picture.
Focal destruction of articular tissues causes disruption of the blood supply and nutrition of the epiphyseal areas of the bones, which die, forming necrosis. Their separation leads to the formation of sequesters. When the active processes of arthritis fade, small destructive foci are replaced by bone tissue, their compaction with sclerotic limitation of large foci. This picture is especially typical for tuberculous arthritis.
Arthritis (purulent) of the right elbow joint
Causes of gonarthrosis
The main causes of arthrosis of the knee joint include:
- Violation of metabolic processes;
- Pathological changes in blood circulation and increased capillary fragility;
- Excess body weight, which leads to increased axial load on the joint;
- Traumatization of the knee joints (torn ligaments, menisci, fractures, cracks);
- Past inflammatory diseases (rheumatism, arthritis);
- Excessive stress on joints that athletes are exposed to. Most often, tennis players, football players, track and field athletes, and gymnasts suffer from gonarthrosis;
- Hormonal and endocrine disorders;
- Old injuries that are inadequately treated or for which treatment has not been completed;
- Congenital anomalies of the structure of joint tissues;
- Hereditary factors.
The main diseases diagnosed using radiation examination
Radiography plays an important role in the diagnosis of osteoarticular felons. They look like typical purulent arthritis - rapidly progressive and uneven narrowing of the joint space, multiple foci of destruction in the articular surfaces, regional osteoporosis, increased joint volume. When performing osteoscintigraphy, an increase in the concentration of radiopharmaceuticals in the periarticular parts of the bones is noted. When using sonography, destruction of articular cartilage is noted, which is confirmed by computed tomography.
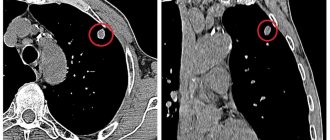
Rheumatoid arthritis has become widespread in recent years. This is a systemic autoimmune disease with a chronic, relapsing course that primarily affects the joints. It has a progressive course and is accompanied by disturbances in the immune response. In the initial stages of the disease, the abnormalities are at the microscopic level, and radiographs are indistinguishable from normal. In such cases, a bone scintigram is used to assess the lesion, showing increased accumulation of radiopharmaceuticals in the area of the affected joints.
The second picture shows stage III rheumatoid arthritis.
However, as the disease progresses, the radiographic method becomes more informative, and radiological diagnostic data are used for the stage classification of arthritis.
The images reveal compaction of the periarticular tissues, an unexpressed decrease in the width of the joint gap and signs of incipient osteoporosis in the bones. Subsequently, such manifestations are accompanied by erosive lesions, which are small marginal defects located at the articular ends of the bones. Together with a violation of the integrity of the end plate, these defects are the main signs of rheumatoid arthritis on radiographs. Subsequently, the joint space continues to narrow, which leads to loss of hand function. The severity of osteoporosis increases, joint dislocations develop.
X-ray of the knee joint description
Have you been trying to heal your JOINTS for many years?
Head of the Institute for the Treatment of Joints: “You will be amazed at how easy it is to cure your joints by taking the product every day for 147 rubles ...
Read more "
The X-ray method is recognized as one of the safest. The radiation used during the study does not accumulate in bones and tissues.
OUR READERS RECOMMEND!
Our readers successfully use Sustalaif to treat joints. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
Radiologists distinguish two types of images:
- Overview – reflect the condition of a large part of the body. When examining the condition of the knee joint, survey photographs help determine whether the pathological process has spread to the entire bone.
- Targeted – provide information about the condition of a specific area of the joint or joint as a whole.
An X-ray of the knee joint shows the condition of the bone, as well as soft tissue and muscles. New generation equipment reflects the condition of the tendons. Cartilage, due to its structure, does not show up on an x-ray. Its thickness can be determined by the distance between the bones that form the joint.
An X-ray of the knee joint is performed in two projections - straight and lateral. The mandatory use of both projections is explained by the complexity of the structure.
Anatomically, the knee is covered from the front side by the patella or kneecap. The information obtained from the direct projection image makes it possible to identify suspected pathologies that explain the patient’s condition.
The lateral projection provides information about the correctness or error of the diagnosis.
Additionally, if the specialist suspects a malfunction of the patellofemoral joint, axial images are taken. This type of study involves bending the limb at the knee as much as possible.
In particularly difficult cases, additional images are prescribed at angles of 15, 45 and 150°. They show the degree of limitation of the proper functioning of all elements of the joint.
Plain X-ray of the knee joint
This type of examination is usually performed in two projections - first from the front side of the joint, and then from the side. The need for an additional image arises due to the complex structure of the knee joint. On the front side it is covered by the patella, which overlaps the overall image.
An external or internal lateral image shows the condition of the kneecap, and it also helps eliminate doubts regarding the detected pathological object. Having seen it in one image, we will determine its exact location in another.
Any photograph of the knee joint is targeted, that is, it depicts only a small area of the skeleton. It is known that any human joint consists of a section of bone that is covered with cartilage tissue. Since the rays easily pass through the cartilage, we do not see it on the x-ray. Therefore, the joint space seems so wide, as if there is nothing between the bones.
Indications for the study
An X-ray of the knee joint allows you to evaluate the thickness and structure of the bones that form the joint.
We do not see the cartilage, but the underlying bone plate will react to its damage - in the form of areas of thinning or thickening, as well as unevenness of its contour.
When assessing the joint cavity, you can see a change in its normal shape and structure, as well as the presence of protruding bone growths (osteophytes).
Depending on the purpose of the study, the picture is taken in one or two projections. But an x-ray can never be bypassed - only after it are more complex diagnostic methods (CT, MRI) performed.
- Traumatic damage to the joint - fractures, acquired dislocations or deformities. Pain, changes in shape and impaired joint mobility are signs that accompany any injury. Here, pictures are taken in two cases - to confirm the diagnosis and to monitor the treatment.
- Violation of the normal structure of the joint - congenital diseases (osteopathy, osteodystrophy).
- Detection of articular cartilage damage based on the condition of the marginal bone plates. In this case, the choice is between two diseases. Arthritis occurs as a result of the inflammatory process, and arthrosis deformans occurs as a result of systemic disorders in the human body.
- Diagnosis of tumors - already on an x-ray, they suggest the approximate origin of the oncological process.
A general and mandatory indication is any suggestion of injury or disease of the bones that form the joint.
Preparation
It is necessary to understand that x-rays of the knee joint are not an ideal diagnostic method. But any pathology will be determined already on it. Further research is needed only to determine the method of treatment.
- There is no need to come for the procedure on an empty stomach, and no special diet is required.
- You should be aware that when taking x-rays, the doctor may ask you to take a certain position of your body or leg. It may be inconvenient, but it is worth following the recommendations - this will allow you to take a more accurate and informative picture.
- During the procedure, at the doctor’s command, you must hold your breath and not move.
Execution technique
The quality and information content of the image is greatly influenced by the incorrect position of the patient on the table and his movement during the procedure. Usually these conditions are prevented by pain in the joint area. To reduce it, use painkillers and warm the limb.
First, the patient is placed on the manipulation table in a supine position. After pointing the device, the first picture is taken - in direct projection. For any diseases, except injuries, this is enough.
https://www.youtube.com/watch?v=TFFfRgSYLNE
If a fracture or dislocation is suspected, an additional radiograph is taken - a lateral one. For this, the patient is either turned onto his healthy side, or, if this is not possible, the leg is abducted and done in a lying position.
What changes can you see?
Normally, in a direct photograph we will see the articular ends of the tibia and femur. They will be of the same density and without visible defects (cracks or splinters). Their surfaces and protrusions correspond precisely to each other. The joint space is the same width and symmetrical on both sides, without any particles or outgrowths inside.
- In case of a fracture, damage of varying sizes and lengths will be determined. Against the background of white and opaque bone, they are depicted as dark stripes running in the transverse direction.
- Dislocation is characterized by displacement of bone surfaces relative to each other. The kneecap is most often damaged; a lateral view is required for diagnosis.
- Congenital diseases are manifested by an asymmetrical structure of the joint. One of its parts may be too small or, conversely, have additional growths.
- Inflammatory and dystrophic diseases are characterized by a decrease in the width of the joint space. The bone plates adjacent to it become thinner and become uneven. Depressions and osteophyte outgrowths appear on their surface.
- A tumor is a round or irregularly shaped mass that grows from the bone or surrounding tissue. Around it there are noticeable areas of destruction and compression of tissue.
Description of the knee joint
The body pays close attention to the health of the knee joint. The knee is a joint with a complex structure that combines the patella, femur, and tibia. It is quite large and often suffers from injuries, inflammatory and degenerative diseases.
The ligaments responsible for the integrity and stability of the joint are the anterior and posterior cruciate, medial and lateral, patellar and transverse ligaments. They are located in the knee cavity and prevent the leg from moving excessively forward or backward. The kneecap, or patella, is connected to the thigh muscles by tendons.
The articular surfaces of the bones are covered with hyaline cartilage; the menisci, crescent-shaped cartilages located between the tibia and femur, are also built from similar tissue. The knee joint has several synovial bursae (bursae) filled with fluid.
When is a knee x-ray prescribed?
X-ray anatomy of the knee joint makes it possible to determine structural changes that occur due to bone damage or a pathological process. The bone tissue is clearly visible on the x-ray. The degree of visualization of soft tissues and ligaments depends on the rigidity of the image. Cartilage damage can be judged by the distance between the surfaces of the bones included in the joint.
The doctor prescribes an x-ray in the following cases:
- knee injury with suspected fracture, crack, rupture of knee ligaments;
- inflammatory process caused by infection or allergic reaction;
- chronic pain syndrome;
- pain, crunching when moving;
- partial limitation of movements in the knee or complete immobility.
The examination is also necessary to determine the degree of degenerative-dystrophic diseases, to identify congenital defects, before surgery for endoprosthetics.
What does an x-ray reflect?
Most pathologies can be detected using an X-ray of the knee or other joint, which is recorded and shown in the image. There is only one drawback, and it is that the method will detect only noticeable deviations.
So, if the damage is minor, even a fracture, the picture may simply not show it. This happens if the radius bone of the arm is broken or cracked. The radius is small, rather thin, and does not appear so clearly.
And often X-rays do not help to say unambiguously about the presence of a fracture or crack.
If we talk about knee joints, then a lot depends on the qualifications of the specialist. The bottom line is that the knee joint has an extremely complex structure; a certain amount of knowledge and practice is required from a specialist to determine the pathology.
First of all, you need to know that the presence of supposedly empty space between the bones is the norm, indicating the health of the joints. This space is not empty, but cartilage tissue. It’s just not visible in the picture, since it transmits X-ray rays perfectly.
But only on the condition that there are no pathologies.
However, at the moment when density in this zone appears in the picture, this already indicates destructive processes. Most often, when a description is made, it refers to the presence of arthrosis of the knee joint.
This is a deforming pathological process that can completely destroy the knee joint and deprive the patient of the ability to walk. The difficulty of arthrosis is that it is often an autoimmune process, and it is almost impossible to stop and reverse it.
Joint diseases cannot be fully cured. The best result is the establishment of long-term remission and maintenance of a calm phase.
But photographs, including those with a load, show not only deformations. The joint itself does not hang in the air, it is surrounded by tissue. He also has a periarticular “bag”; in case of pathologies, fluid accumulates there.
Then a darkening of the gap is also created, as well as in the presence of cracks and swelling in the tissues. Some photos show varying degrees of abnormalities and it seems that it can be self-diagnosed.
However, we pay special attention: treatment and diagnosis are carried out only by a specialist.
What can x-rays reveal?
It is generally accepted that x-rays have a more harmful effect on the body than ultrasound diagnostics. This is true.
In some cases, doctors prescribe ultrasound for preventive purposes - to assess the size, shape and functioning of certain organs, to identify the early stages of certain diseases, as well as to obtain a picture of the health of a pregnant woman and the baby growing in her womb.
Radiography cannot be used frequently even to monitor the development of severe pathologies. It is completely contraindicated for pregnant women, as it can cause irreparable harm to the fetus.
Medical specialists do not recommend that patients undergo an X-ray of the knee for preventive purposes; only a doctor can give a referral for such a study. This is due to the fact that the joint tissue receives a daily dose of radiation during analysis.
It can negatively affect the normal functioning of the limbs.
It is necessary to immediately undergo diagnostics using X-rays if the following appears in the area of the knee joint:
- pain;
- swelling:
- swelling:
- redness;
- elevated temperature,
- joint deformities;
- signs of bone displacement.
X-ray of the knee joint can reveal the presence of fluid in the joint tissues; it also qualitatively diagnoses the condition of the cartilage.
You need to know: if nothing is visible in the image between the bones (where the joints should be), this means that the articular tissues are normal and there are no pathological changes or destructive processes dangerous to health; When there is swelling or fluid in the area of the knee joint, it will become visible on an X-ray of the knee joint.
But it will not be possible to accurately determine bone density using such diagnostics, however, x-rays will show the shape and structure of the bones and help determine the pathologies progressing in them. X-rays of the knee area can also detect bone tissue disorders.
If bone tissue in a particular area of the body begins to deteriorate and become thinner, x-rays will detect this deviation, therefore this research method is used as one of the effective ways to detect osteoporosis.
Source: https://shejnyj.asustav.ru/narodnye-sredstva/rentgenografiya-kolennogo-sustava-opisanie/
Systemic diseases affecting joints
There are also a number of diseases that include seronegative arthritis syndrome:
- Systemic lupus erythematosus.
- Periarteritis nodosa.
- Scleroderma of various origins.
- Gout.
- Reiter's syndrome.
- Arthritis with psoriasis.
- Ankylosing spondylitis.
They are difficult to recognize and differentiate between each other if you use only one approach to studying the patient. Therefore, to make a correct diagnosis, a comprehensive study and use of both radiological data and objective examination, laboratory tests and a careful study of the medical history are necessary.
Additional research methods
MRI of the knee joint
If necessary, sonography can be used. It shows thickened joint membranes, the presence of free fluid in the joint cavity, changes in the density of articular cartilage, periarticular edema and the presence of synovial cysts. MRI and computed tomography are also used. These techniques make it possible to assess the condition of the tissues that surround the joint and judge the prevalence of the pathology, its danger and the rate of progression.
Joint examination methods
The first is a survey, in the language of the aesculapians, anamnesis collection. The main symptom for diseases of the joints of the upper and lower extremities is pain. The joint, along with mechanical functions, performs the function of a receptor field, that is, it contains receptors that perceive and transmit “distress signals” to our brain.
Therefore, joint pain is of a reflex nature, which means that joint pain should be considered not only based on the biomechanical characteristics of the musculoskeletal system, but also from the position of the reflex nature of pain. Pain receptors are located in the fibrous and synovial layers of the capsule; their irritation can be caused by functional overload of the joint or the reaction of the synovial membrane to inflammation and injury.
The nature of the pain syndrome is one of the differential diagnostic signs that helps to distinguish one disease from another. Rheumatoid arthritis or an inflammatory process in a joint is characterized by an “inflammatory” nature of pain - it arises or increases at rest, at night, and subsides with movements in the joint.
Osteoarthritis is characterized by “mechanical pain,” that is, pain that occurs or intensifies during load on the joint and subsides with rest. The pain usually appears some time (minutes or hours) after exercise, and continues for several hours or days even after the exercise has stopped.
The pain at the first manifestation of osteoarthritis is not as severe as with arthritis, although as the disease progresses it becomes persistent. Therefore, an experienced doctor, to a certain extent, even by the nature of the pain and its persistence, can determine the severity of the disease as a whole.
As a result of pain, protective tension in the periarticular muscles is formed, limiting mobility in the joint.
A feeling of stiffness in the joints is a common complaint of patients with joint diseases.
Stiffness is usually characterized by difficulty in the first movements - the phenomenon of a “frozen” joint after a period of rest, limited range of motion in the affected joint. Stiffness usually occurs only in the affected joint and lasts several minutes, due to thickening of the joint capsule.
Prolonged morning stiffness is observed with rheumatoid arthritis, the development of synovitis (effusion in the joint) or reactive arthritis. Thus, the duration and severity of morning joint stiffness reflects the degree of local inflammation.
Joint pain is a common symptom not only of joint diseases, but also of other pathologies that have a different etiology. For example, constant, debilitating “bone pain” is characteristic of tumor metastases to the bone. Any acute and chronic infection, intoxication, neuroendocrine disorders (diabetes mellitus, thyrotoxicosis) can cause joint pain of varying duration and intensity.
Upon examination, you can identify the following signs of joint disease. Swelling and smoothness of the contours of the joint are observed when there is effusion in the joint (synovitis), or when there is swelling of the joint capsule or periarticular tissues.
Despite the emergence and development of modern diagnostic methods, X-ray examination remains the most common method in the clinical practice of orthopedists. This method is quite informative, accessible, safe and economical.
- narrowing and unevenness of the joint space;
- subchondral osteosclerosis (hardening of bone areas adjacent to cartilage);
- the presence of osteophytes (marginal bone growths in the joint area - what is called salt deposition);
- areas of ossification of the joint capsule and ligaments (deposition of calcium salts into the periarticular tissues);
- periarticular marginal bone defects;
- subchondral cysts (cyst-like cavities in areas near a joint).
DETAILS: Morning stiffness in the leg joints
Arthroscopy is a direct visual examination of the joint cavity. A video camera, light source and manipulator instruments are introduced into the joint cavity under anesthesia. Arthroscopy allows you to examine the structure of the joint and the surface structure of the cartilage, conduct a targeted biopsy (take a section of joint tissue for examination), as well as low-traumatic therapeutic surgical procedures.
Radioisotope scintigraphy. The joints are examined using osteotropic radiopharmaceuticals (pyrophosphate) labeled with a radioactive substance 99m Tc. These drugs accumulate in places of active metabolism in bone and connective tissue, especially intensively in inflamed joints, as can be seen on joint scintigrams.
Thermography (thermal imaging) is a method for studying the intensity of infrared radiation in tissues. Using this method, the temperature of the skin in the joint area is remotely measured, which is recorded on photographic paper in the form of a contour shadow of the joint. The method allows one to judge the activity and dynamics of inflammatory joint damage.
Magnetic resonance imaging (MRI). The method is based on studying the magnetic field of the patient’s joint tissue. The main advantages of the method include: non-invasiveness, harmlessness (no radiation exposure), three-dimensional nature of the image, no overlay of bone tissue on the image, the highest accuracy of the image of various joint formations.
Sonography (ultrasound examination). The method is used to assess soft tissue pathology, identify fluid in the joint, and visualize cartilage and superficial bone structures.
Computed tomography (CT). The method is most informative for assessing the bone structure of the articular ends of bones in various parts of the joint.
Additional and special research methods for each patient are determined individually by the attending physician, based on the principle of maximum information content and minimal invasiveness.