The shoulder joint is the most complex bone joint - unlike the knee joint, it has a more complex anatomical structure, as well as greater functional and motor capabilities. That is why, if a person experiences pain in the shoulder-scapula region, he should seek medical help from a qualified orthopedist.
An experienced specialist can suspect a particular pathological process without prescribing expensive diagnostic methods - during a clinical examination of the patient, conducting specific tests. However, it is possible to clarify the diagnosis only after an instrumental examination of the patient - fluoroscopy, magnetic resonance imaging or ultrasound scanning.
In many medical institutions, the mandatory algorithm for examining patients with pathological changes in the structures of the shoulder includes x-ray examination. However, nowadays everyone knows that the radiation method is highly informative only for traumatic injuries of bone tissue. When there are changes in the soft tissues of the joint, X-ray diagnostics provide the doctor with insufficient information.
When studying the musculoskeletal system, practitioners prefer sonography. Extensive experience has shown that to identify most pathological processes in the joint connecting the shoulder girdle with the upper limb, this non-invasive study using ultrasound waves should be used. In our article, we will provide information on in what cases an ultrasound scan of the shoulder joint should be performed, on the features of preparing and performing the procedure, and what problems are identified during diagnosis.
When is it prescribed?
It is advisable to perform an ultrasound of the shoulder joint if:
- autoimmune diseases;
- traumatic lesions (including when there is discomfort in the shoulder and forearm);
- preventive examination;
- diagnosed or suspected systemic disease;
- the initial stages of the disease, which is not possible to determine with an X-ray machine;
- identifying articular cartilage pathology on x-ray;
- painful movements or reduction in their volume;
- swelling of tissues in the shoulder area;
- such a diagnosis as “bursitis”;
- congenital dislocation of the hip or joint dysplasia, as well as suspicion of these pathologies;
- suspicion of a Becker cyst or its rupture;
- the need to establish the nature of the injuries;
- diagnosing the causes of the appearance of blood or other fluid in the joint cavity;
- planning the puncture or after it.
Survey objectives
Ultrasound of the shoulder joint is used for minimally invasive procedures - local injection therapy, bubbling of the subacromial bursa, puncture and aspiration biopsy. But its main goal is to detect various pathologies. Ultrasound examination of the shoulder is prescribed in the following cases:
- when the patient complains of pain at rest and (or) during movement;
- with limited range of motion, hardening of soft tissues, development of swelling;
- if an inflammatory process is suspected as a result of injury or destructive-degenerative changes, as well as for their differentiation;
- for diagnostics at the initial stage of pathology, when tissue destruction cannot be detected using radiography or magnetic resonance imaging;
- to study the course of deforming arthrosis, osteoporosis, rheumatoid arthritis to establish the stage of the pathology, the degree of its progression, and detect complications that have arisen;
- to assess the effectiveness of conservative treatment, tissue healing after surgery, before deciding on the need for minimally invasive or invasive surgery;
- to determine the advisability of additional instrumental studies - arthroscopy or scintigraphy.
Recently, ultrasonography has become actively used in axillary blockades with intravascular injection of local anesthetics. Their frequent complications are systemic toxic reactions and the formation of extensive hematomas. Puncture can also lead to temporary spasm of the artery and absence of its pulse, and sometimes occlusion of the axillary vein. The use of ultrasound control allows you to visualize each nerve, vessel, and needle position.
Ultrasonography is recommended by the American and European Societies of Regional Anesthesiologists and Pain Therapy Specialists for performing peripheral neuraxial blocks. Using ultrasound, you can control medical procedures, prevent the development of complications, and reduce the amount of anesthetic used.
What will the examination show?
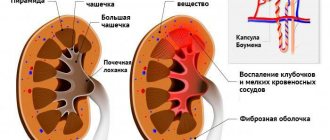
Ultrasound examination of tendons, ligaments and joint tissue will allow timely detection of signs of such common diseases as:
- Epicondylitis is an inflammatory-degenerative lesion of the elbow joint.
- Synovitis is inflammation of the synovial bursa.
- Reactive arthritis is inflammation of the joints resulting from an infection.
- Tendonitis or tenosynovitis are inflammatory processes in the tendons and their membranes. Clinically they appear as hypoechoic areas of irregular shape.
- Synovial cysts are characterized by enlargement of the affected joint.
- Cartilage erosions are part of immune-inflammatory processes, irreversibly changing joints.
- Effusion in the joint capsule is characterized by the accumulation of biological fluid in it.
- Injury due to wear or bruising of one of the four muscles that make up the rotator cuff.
- Fracture – with a change in the surface of the humerus.
- Bursitis is one of the types of inflammation of the synovial bursa, leading to changes in the structure and size of its walls.
- Partial separation of the ligaments located between the collarbone and scapula is characterized by incomplete disruption of the structure of the ligament.
- Damage to the labrum – the attachment point of the biceps ligaments and tendons.
- Rupture of the cartilaginous connection means separation of the cartilage from the area of fixation.
- Rheumatoid arthritis - on the monitor screen the doctor will record an abundance of bone tissue defects, as well as atrophy of adjacent muscles and, possibly, fluid accumulation in the joint capsule.
Important! With the development of diagnostic technologies, it has become clear that damage to the labrum often accompanies shoulder injuries.
Advantages and disadvantages of ultrasonography
The ultrasound imaging method has a greater number of advantages compared to radiography and magnetic resonance imaging. Ultrasonography is non-invasive, does not cause pain to the person being examined, is easy to perform and is accessible. No ionizing radiation is used to obtain images, and the cost of the diagnostic procedure is relatively low.
During an ultrasound, the soft tissues of the shoulder joint are carefully examined - muscles, tendons, bursae, ligaments and joint capsules. These elements cannot be seen during routine x-ray examination. The undoubted advantage of ultrasonography is the ability to diagnose in real time. This is relevant when examining the joint structures of the shoulder, as it allows you to evaluate the work of muscles and tendons with an increase or decrease in motor activity. The diagnostician often immediately makes all the adjustments and determines on the spot the type of contents of the cavity according to the following parameters:
- establishing the degree of its compressibility;
- identification of the nature of vibrations under mechanical influence.
Many clinical trials have been conducted to compare the effectiveness of methods for diagnosing pathological changes in the shoulder joint. In addition to the fact that ultrasound examination is technically simple and inexpensive, its advantage over MRI is that it does not use magnetic field energy. Ultrasonography can be used when examining patients with implants (eg, pacemakers).
Ultrasound of the shoulder joint is used to diagnose pathologies in patients with claustrophobia, since it does not involve the patient being in a confined space.
MRI and ultrasonography of the shoulder joint have not become interchangeable diagnostic techniques. When prescribing each of them, the doctor assumes a specific goal and task. Ultrasound also has certain disadvantages that limit its use:
- difficulties in the penetration of ultrasound through bone tissue;
- visualization of external structures only.
Therefore, ultrasound is not used to evaluate the status of any intra-articular joint injury. Magnetic resonance imaging allows you to obtain high-quality images of all elements: the capsule with the glenohumeral ligament, the cartilaginous lip, the hyaline cartilage on the heads of the humerus and the articular cavities of the scapula. The muscles and tendons surrounding the joints are clearly visualized.
Another advantage of ultrasonography over MRI is the possibility of a detailed study of articular structures, which makes it possible to differentiate tendinositis and tendinitis through the use of Doppler mapping.
| Benefits of ultrasonography of the shoulder joint | Disadvantages of Ultrasound |
| A small number of contraindications (individual sensitivity to the gel used) | Superficial assessment of bone structures |
| Get results in real time | Inability to fully visualize ligaments and tendons |
| Painless procedure | — |
| Possibility of assessing the condition of the joint in motion | — |
| Availability and relatively low cost | — |
| Lack of necessary preparation stage | — |
MRI, ultrasound or x-ray?
Which is better: ultrasound or MRI of the shoulder joint? If there is no need to determine fractures, then ultrasound is a more informative method than x-rays and much less expensive than MRI.
Important! It is optimal to carry out ultrasound examination of joints for pathologies of the cartilage pad or tissue, joint capsule, muscles, and ligaments.
In this case, MRI is even inferior to ultrasound examination.
Compared to X-rays, ultrasound is not only a procedure that shows a more complete picture of the disease, but also does not carry a radiation dose to the body. However, if you need to diagnose the skeletal system and identify cracks, fractures or dislocations, the doctor usually chooses a CT scan or x-ray due to the greater information content of the images.
Indications for examination
Scanning parts of the human body using ultrasonic waves makes it possible to detect pathological processes in the early stages of their development and promptly begin treatment measures. Ultrasonography plays a special role in such medical fields as rheumatology, which deals with the treatment of spondyloarthropathy, reactive and rheumatoid arthritis, systemic lupus erythematosus, etc.
Of course, ultrasound cannot provide reliable information about the condition of parts of the shoulder joint located at a far distance from the surface of the body and identify foci of inflammation that affect only part of the articular joint. However, with the help of ultrasound diagnostics it is possible to assess the condition of tendons, cartilage, muscles and ligaments. This cannot be done with fluoroscopy.
Diagnostic arthroscopy
Ultrasound scanning is an absolutely safe procedure for the human body. Practitioners prescribe it with a certain frequency for existing pathologies of bone and joint tissue to monitor the ongoing course of treatment, assess the dynamics of the condition of the shoulder at rest and during movement.
Ultrasound of the shoulder joint is performed:
- for injuries;
- autoimmune pathologies;
- detection of osteochondropathy on radiography (damage to the musculoskeletal system associated with tissue nutritional disorders);
- systemic diseases;
- the patient has complaints of swelling and hardening of the tissues of the shoulder of unknown origin, pain in the joint, limitation of its movement and change in shape;
- preparation for puncture or surgical intervention.
People whose professional activities involve a serious load on the joint system (musicians, athletes, dentists, loaders, builders, mechanics) should periodically undergo diagnostics of the shoulder joint
Preparation
Before the procedure, there is no need to follow a diet or stop taking your usual medications. However, before a study that includes puncture of the fissure space of the joint, it is necessary to clarify the need to discontinue diuretics.
Reference! Ultrasound of the shoulder does not require any special preparation.
When going for an ultrasound, take with you the existing test results or x-rays, or MRI scans taken previously. If you plan to undergo an examination at a municipal clinic, you must take an insurance policy and a referral from your attending physician. If the procedure is scheduled at a private medical center, then a wallet with a certain amount will be useful.
Causes of pain in the shoulder joint
Traumatic injuries
Pain in the joint is a consequence of falling on your arm, twisting your shoulder, or a sharp jerk or blow.
Occurs due to household, street and sports injuries. Less commonly formed in industrial accidents, falls from heights, and road traffic accidents. Swelling is noted, bruising and abrasions are possible. A bruise of the shoulder joint develops upon impact. The pain at the time of injury is moderate and subsides fairly quickly. Swelling is moderate or insignificant, limb function is preserved, limited due to pain. A dislocation occurs when you fall on a straight arm or get hit. There is a very sharp pain combined with a clicking sound. High pain intensity persists until reduction. The shoulder joint is deformed, and there is a depression at the site of the humeral head. Movement is impossible.
A fracture of the head or neck of the humerus, or separation of the greater tubercle, occurs with an impact or fall on the shoulder. Intense explosive pain is typical, sometimes a bone crunch is heard. The pain does not subside over time. To avoid increased pain, the patient holds the sore arm with the healthy one. Severe swelling, diffuse cyanosis are detected, deformation, pathological mobility, and crepitus are possible. Movements are severely limited.
Tears and tears of the rotator cuff are accompanied by sharp pain radiating to the neck, forearm, and hand. Depending on which muscle is affected, the pain intensifies when trying to lift, abduct or rotate the arm. If movement is impossible, this indicates a complete rupture of the tendon; if it is possible, but sharply painful, this indicates a partial rupture.
Soft tissue diseases
Bankart injury occurs in the long-term period after anterior shoulder dislocations and is characterized by severe tugging, burning or cutting pain when trying to move the arm back, combined with a feeling of instability of the joint, a conscious limitation of movements for fear of re-dislocation.
Tendopathies develop in other diseases of the shoulder joint, after injuries. Initially, they are characterized by short-term pain at the peak of the load. Then aching or nagging pains begin to bother you with moderate and light exertion, at rest, at night. With calcific tendinosis, a crunching sound is heard during movement.
With adhesive capsulitis, the pain syndrome appears without connection with external causes, gradually increases over 2-4 weeks, intensifies at night, when lying on the sore shoulder. The pain is chronic, constant, exhausting, preventing any movements, including passive ones. Pain gradually decreases and disappears within 10-14 months along with a progressive limitation of range of motion.
Acute myalgia of the deltoid muscle develops against the background of injury, infection, significant physical activity, and exogenous intoxication. Accompanied by local aching, pressing, bursting pain. The pain increases sharply with muscle tension, forcing the patient to search for a comfortable position of the limb.
Degenerative joint lesions
Arthrosis of the shoulder joint is characterized by chronic diffuse pain with a predominant localization in the depths of the joint. At first, the pain is periodic, not intense, dull, aching, pulling, and appears at the beginning of movements, after significant exertion. Subsequently, the pain becomes longer lasting, sometimes burning, tugging, or encircling. They persist at rest, occur at night, are accompanied by a crunching sound, and are combined with increasing limitation of mobility.
With arthrosis of the acromial clavicular joint, pain is felt above the shoulder joint, in the distal part of the shoulder girdle. The pain is chronic, has the same dynamics as with arthrosis of the shoulder joint, but is distinguished by a clear localization and more superficial location, intensified by pressing on the acromial end of the clavicle, bringing the bent shoulder towards the body.
Synovial chondromatosis occurs after injury or without external causes, and is characterized by wave-like dull pain of moderate intensity, often worsening at night. Short-term severe shooting pains and sudden restrictions of movements are possible due to blockade of the joint by chondromic bodies.
Aseptic necrosis of the humeral head (Hass disease) is rare; at the initial stage it manifests itself as intermittent dull pulling or pressing pain during movements. Over the course of about a year, the duration and intensity of the pain gradually increases, then the pain appears at rest, and the function of the limb is limited.
Inflammation of hard structures
With arthritis of the shoulder joint, the pain is diffuse, dull, nagging, and occurs after an injury, against the background of an infectious or rheumatic disease. At first, the pain is weak, intermittent, intensifying in the evening, after physical activity. Then - long-term, medium intensity, remaining at rest. When infected, the pain becomes sharp, jerking, shooting, pulsating, and is combined with symptoms of general intoxication.
Hematogenous osteomyelitis usually occurs in childhood, affects the upper parts of the humerus, is manifested by local bursting, tearing, boring pain, which quickly intensifies to unbearable, combined with symptoms of intoxication, chills, and a sharp deterioration in general condition. With post-traumatic osteomyelitis, the clinical manifestations are similar, but develop more slowly and occur against the background of open fractures.
Inflammatory diseases of soft tissues
Acute aseptic bursitis of the shoulder joint is manifested by moderately severe arching diffuse dull pain, swelling, and slight hyperemia. When transitioning to a chronic form, the pain decreases; with the development of infectious bursitis, it intensifies, becomes sharp, twitching, pulsating, deprives you of night sleep, and is combined with an increase in edema, hyperemia, increased body temperature, and signs of general intoxication.
Tendonitis forms after tears of the rotator cuff or due to overload. The patient experiences pain when trying to move the arm to the side (damage to the supraspinatus muscle), turn the shoulder outward (inflammation of the infraspinatus or teres minor muscle), or place the arm behind the back (subscapularis tendinitis). The pain is moderate or not intense, aching or nagging.
Synovitis is a complication of injuries and other diseases of the joint, characterized by a dull arching pain that gradually intensifies over several days, correlating with an increase in the volume of the joint (amount of fluid). When the effusion suppurates, the pain is acute, twitching, intense, exhausting, accompanied by disturbances in the general condition.
Autoimmune pathologies
In rheumatoid arthritis, both joints are often involved. The mild form is characterized by intermittent weak pain of a pulling or pressing nature and morning stiffness. Moderate activity of the autoimmune process is manifested by periodic, prolonged dull, pressing, aching or bursting pain at rest and during movement, and prolonged stiffness. In the severe form, diffuse wave-like intense pain is observed, intensifying at night, constant stiffness, persistent synovitis, weakness, and hyperthermia.
With systemic lupus erythematosus, pain in the shoulder joints is often symmetrical, although unilateral damage is possible. In mild cases, the pain is dull, local, pulling or aching, and quickly disappears. In severe cases, the pain is progressive, wavy, diffuse, disrupting night sleep, combined with swelling, redness, and synovitis. Lesions of the skin and internal organs are noted.
Rheumatism is manifested by severe but short-term migrating pain in the shoulder and other joints, which occurs 1-2 weeks after an acute infectious disease. Variability is typical - the pain can be throbbing, burning, baking or dull, pressing, pulling. They persist for several days, then disappear or sharply weaken.
Tumors
Benign tumors (non-ossifying fibromas, osteochondromas, chondromas) have a long-term course, are asymptomatic, and are characterized by intermittent, low-intensity local pain, which remains at approximately the same level for many months or years. As neoplasia increases, synovitis occurs and a hard lump is felt in the joint area.
With malignant neoplasia, the pain is initially dull, vague, fuzzy, dim, and sometimes intensifies at night. The pain quickly progresses, becoming diffuse, sharp, bursting, burning, tugging, cutting. Accompanied by swelling, deformation, and general impairment. At an advanced stage, the pain is unbearable, exhausting, and can only be relieved with narcotic analgesics.
Neurological causes
Pain in the shoulder joint is often caused by pathology of the cervical spine. Typical are “lumbago” – sudden sharp pain that often radiates throughout the arm, from the shoulder to the fingertips. There may be mild pain spreading from the neck to the shoulder. A distinctive feature of the pain syndrome is the preservation of range of motion. Possible neurological causes of pain associated with damage to the spinal column:
- osteochondrosis;
- disc herniation;
- spondylitis;
- spondyloarthrosis;
- spondylosis deformans;
- spinal stenosis.
Pain in the shoulder joint, shoulder girdle, and upper arm can be caused by superior plexitis (Duchenne-Erb palsy). One-sided shooting pain is observed with pressure on the supraclavicular and subclavian areas, limitation of movements, and sensory disturbances.
Other reasons
In diseases of the internal organs, referred pain occurs in the shoulder joint due to the presence of myofascial trigger points. The following pathologies cause pain:
- cardiovascular system: ischemic heart disease, pericarditis;
- chest organs: pneumonia, pleurisy, mediastinal tumors, Pancoast cancer;
- abdominal organs: gastric and duodenal ulcers, cholecystitis, cholangitis, hepatitis, cirrhosis, fatty hepatosis.
Pain in the shoulder joint sometimes occurs with depression and some mental disorders. In diabetes mellitus, it has an organic basis due to the increased likelihood of developing tendinitis, capsulitis, and other minor rheumatological diseases. It can be provoked by taking anabolic steroids (due to necrosis of the clavicle and acromion process), corticosteroid drugs (due to necrosis of the humeral head).
How do they do it?
The patient frees from clothing not only the area of the joint being examined, but also the collarbone, as well as the scapular area.
Reference! The doctor invites him to take a seat on the couch: during the examination, the patient sits and his hands lie on his knees.
Method of performing ultrasound of the shoulder joint:
- The doctor begins the examination from the synovial bursa and tendon complex and ends with determining the condition of the nerve fibers.
- During the procedure, the patient moves his arm back, to the side, or rotates his limb at the request of the diagnostician, ultimately bringing it closer to the body.
To complete the examination, the image of the joint is visualized in several planes. Sometimes, for the purpose of comparative diagnosis, there is a need to examine a healthy joint.
In the video below you can see the procedure for performing an ultrasound of the shoulder joint using a specific example:
The duration of the manipulations is from 15 to 20 minutes, upon completion the patient receives a report with a detailed description of the condition of the joint.
The principle of studying the articular apparatus using ultrasound
Ultrasound is based on the principle of operation of the sonar system - when sound waves collide with an obstacle, its reflection forms an echo. Detailed analysis of reflected waves allows one to evaluate the location, size, shape and consistency of objects. When performing an ultrasound of the shoulder joint, the ultrasound probe sends high-frequency waves that penetrate the joint structures. Special sensitive equipment detects, records reflected vibrations and visualizes them on the monitor.
Ultrasonography is considered a highly informative method for examining bone and cartilage tissue. That is why it is used to diagnose destructive-degenerative pathologies and rheumatological diseases, determine the degree of bone damage due to prolonged compression and bruises, identify the early stages of the inflammatory process and disorders of the normal structure of the soft elements of the shoulder.
Norms and decoding
In a normal state, a little fluid can be observed only in the inner layer of the articular capsule of the long head of the biceps; it should not be anywhere else. There should also be no external signs of damage in the area being examined. The normal length of the brachial nerve is 4.6 mm wide and 2.3 mm long.
What might be included in a research protocol? The following ultrasound signs are characteristic of joint pathology:
- With defects in the rotator cuff, that is, the four muscles responsible for joint mobility and stabilizing the shoulder, tissue tears, both partial and complete, can be observed. Depending on how far the torn parts are removed, there are several degrees of rupture.
- Humeral fractures are characterized by unevenness and fragmentation of the surface of the bones, as well as a violation of the integrity of the bone tissue.
- With tendinitis or tenosynovitis, the tendon will have a hyperechoic structure with a hypoechoic rim.
- Bursitis is characterized by an increase in the joint capsule and a change in the structure of its walls. The formation of calcifications and heterogeneity of the echostructure is possible.
- With joint tears, the doctor will see a larger-than-usual distance between the two bones at the location of the tear.
- The formation of joint effusion of any etiology, damage to the articular labrum, which accompanies most traumatic injuries, and ruptures of cartilage tissue are clearly visible on ultrasound.
- With rheumatoid arthritis, erosive defects of bone tissue may appear that have an irregular shape and sharp edges. Additionally, inflammation of the muscle septa, atrophy and the formation of fluid in the joint cavity can be detected.
How the research is carried out
The patient's position during ultrasonography is lying or sitting on a couch with arms down. The patient completely exposes the affected arm. The doctor is located in front of the desired area.
If it is necessary to perform an ultrasound of the left shoulder joint, the patient sits with his left shoulder in front of the doctor, who then applies a special contact gel to the skin. Comparison of results sometimes requires examination of the healthy arm.
The sensor is installed on the shoulder area, moving along its entire surface, capturing the level of the shoulder blade. The angle of inclination varies depending on the joint structures. During the examination, the diagnostician may change the position of the hand, ask to raise it up, or turn it outward. This will improve visualization.
Description of shoulder ultrasound in video:
Contraindications
Completely harmless and atraumatic, the ultrasound diagnostic method is successfully used even in pediatrics, for the youngest patients. There is currently no scientifically based evidence of the harm of the procedure.
Difficulties can only arise if movements in the joint are difficult or impossible.
In addition, there are specific circumstances in which it is better to postpone the procedure:
- the patient has a rash or other manifestations of skin diseases at the site of the proposed examination;
- there is a large shoulder wound;
- there are any acute diseases.
Research technique
Of course, there are an endless variety of potential techniques, but there are basic shoulder ultrasound techniques that all physicians should adhere to. It is important to be aware of “tendon anisotropy” during ultrasound examination of the shoulder joint. Therefore, each tendon must be scanned in several projections and each has its own technique. Ultrasounds of the left and right shoulder joints are performed similarly to each other.
Biceps tendon
Patient position: arm in neutral position, elbow flexed 90 degrees, forearm supported (palm up). The long head of the biceps tendon is depicted in the bony groove as it passes under the transverse humeral ligament in both transverse and longitudinal sections.
Normal findings: The tendon should be located in the bony groove with minimal fluid around it (the tendon sheath communicates with the shoulder joint), and the tendon fibers should be seen without tears, irregularities, or thickening.
Visualized pathology of the biceps tendon: long head, dislocation of the biceps tendon, or subluxation, tendinopathy, effusion in the shoulder joint.
Subscapularis tendon
Patient position: The arm is held in the same position as above and rotated outward, pulling the subacular tendon into it. Image planes: The subscapularis tendon should be traced both longitudinally and transversely. During longitudinal: the transducer is placed in a transverse position (medially) over the humeral head with the transducer marker away from the patient's torso. The probe is then moved from top to bottom to access the three parts of the tendon, i.e. the upper, middle and lower fibers. Dynamic examination: by internal and external rotation of the arm while the sensor remains motionless, possible tendon damage can be assessed; as shown by bunching the tendon during internal rotation as it passes under the coracoid formation. Transverse images: By rotating the probe 90 degrees (now in the craniocaudal direction) toward the patient's head, the short axis of the three parts of the tendon can be assessed by slowly lifting the probe from its insertion to the lesser tuberosity and the medial one. Imaging pathology: supraspinal tendinopathy, long head biceps tendon dislocation or subluxation.
Supraspinatus tendon
Patient position: internal rotation and extension of the shoulder. The supraspinatus tendons should be traced both longitudinally and transversely. Most ruptures occur in the most distal portion and therefore this area should be explored with caution.
Normal Findings: The tendon is parallel to the curved contour of the humeral head, flattening as it inserts into the greater tuberosity, it has a fibrillary pattern, the subacromial bursa should be considered as one thin hyperechoic line parallel to the tendon, the presence of fluid (secretion of the hyperechoic line by hypoechoic fluid) is abnormal as and thickening of the bursa.
Imaging pathology: supraspinal tendinopathy, galvanic rotator cuff tendinitis, subacromial bursitis.
Infraspinatus tendon
Image Planes: The infraspinatus tendon should be traced both longitudinally and transversely. Normal results: separation of the infraspinatus tendon from the supraspinatus tendon is difficult, so much so that a random cut is used at a distance of 1.5 cm from the anterior edge of the supraspinatus; i.e., the first 1.5 cm of the rotator cuff is designated as the supraspinatus tendon, and the next 1.5 cm is the infraspinatus tendon. The thickness of the posterior rotator cuff is significantly less than the anterior rotator cuff (3.6 vs. 6 mm), and therefore thinning should not be interpreted as partial tears.
Imaging pathology: tendinopathy, including ruptures.
pros
Unlike some other diagnostic tests, ultrasound does not harm the body : there is no radiation exposure, so ultrasound can be performed even on infants and pregnant women. The value of the method also lies in the fact that you can be examined using ultrasound as often as necessary.
An ultrasound machine makes it possible to clearly examine the cartilage, joint tissue and vessels responsible for the blood supply to this area. The study is not fraught with any side effects; it has almost no contraindications. An additional plus is the affordable price of the study, compared to other diagnostic procedures (especially CT and MRI).
Features of ultrasound examination
Ultrasound of the movable joints of the skeleton bones can be done without prior preparation. The only point that requires discussion with the treating specialist is the advisability of discontinuing the diuretic before diagnosis when planning collection of synovial fluid. Ultrasonography is an absolutely harmless and safe procedure that is performed even on newborn babies. The only thing that makes its technical implementation difficult is the limited movement of the bones of the shoulder joint.
To conduct the examination, the patient needs to remove clothes and provide access to the joint, scapula area, supraclavicular and subclavian areas. The progress of the procedure consists of the following actions by the patient and the sonologist:
- The patient sits on a rotating chair and places his arms bent at the elbows - the shoulder joint is examined in this position, the condition of the head of the biceps, obtained in a transverse and longitudinal section of the plane, muscle fibers with hyperechoic properties, and synovial fluid filling the joint cavity are assessed.
- The patient withdraws his arm and turns it with his hand up - the subscapularis muscle is examined.
- The patient places his hand behind his back - the tendons of the connective tissue plate surrounding the outside of the bones (periosteum) and hyaline cartilage are examined.
- The doctor moves the ultrasound sensor closer to the axis of the body, and the patient brings his hand to the body - the glenohumeral joint, the anterolateral surface of the joint, the round minor muscle, the tendons of the inner shell of the joint (subosteum), the back of the articular labrum, the junction of the clavicle and acromion (humeral) are scanned. process of the scapula).
This examination scheme is standard - a similar technique is used to diagnose most pathological processes.
Ultrasound scanning allows you to detect changes in the tissues and synovial fluid of the shoulder joint, as well as accurately diagnose inflammatory processes and tumor formations
Reviews
Basically, ultrasound of joint tissue receives only positive reviews: patients are satisfied with the accuracy and volume of information, as well as the speed and quality of the procedure.
It happens that the information obtained from ultrasound needs to be supplemented with data from magnetic resonance therapy.
The fact is that ultrasound diagnostics is not the most accurate way to assess the condition of the joint. Some cases may require different research methods.
And if you do not need to identify pathology or track the dynamics of the process, but clarify the nuances of the disease, then you should prefer ultrasound to magnetic resonance imaging.
The essence of the method
The ultrasound technique is based on sound waves emitted from a transducer, which are then returned back from underlying structures based on the density of that structure. The computer interprets the returning sound waves and creates images that reflect the quality and density of the tissue from which the waves return. When the sound waves are bounced back quickly and with great force, like hitting a bone, an intensely white image (“hyperechoic”) appears on the screen. When sound waves encounter a substance that transmits the waves easily and they do not return like air or liquid, a dark image (“hypoechoic”) is displayed on the screen.
Does ultrasound have contraindications?
This research method has practically no contraindications, the main ones include:
- Presence of skin rashes. Skin diseases such as acne, eczema, psoriasis can serve as an obstacle to a full-fledged study. They may become wet and cause pain for the patient.
- Cuts, abrasions and hematomas on the epidermis. The presence of damage to the upper skin also complicates the examination of the joint. The gel can get into the wound and cause an inflammatory process, the patient experiences pain. It is better to postpone this procedure until the damage has completely healed.
- Acute pain in the shoulder joint. Some diseases of this area can manifest as severe inflammation; pressing on the epidermis with a sensor can cause severe pain in the patient. In this case, you will have to use computed tomography.
- Allergic reaction to the composition of the gel. Sometimes patients have this reaction. In this case, the patient needs to undergo examination in a different way or purchase a hypoallergenic gel before the ultrasound.
Everything you wanted to know about shoulder ultrasound can be found in this video:
Progress of the procedure
The patient is in a sitting position, with his arms down. The doctor is located opposite the patient so that there is access to the shoulder area. The sensor is initially positioned perpendicular to the midline of the body. In this position, the following anatomical formations can be found in the area of the shoulder joint:
- biceps;
- biceps tendon;
- head of the humerus;
- deltoid;
- subcapsular muscle.
By moving the sensor up and down, changing the angle of its inclination relative to the body, you can examine its components in more detail on an ultrasound of the shoulder joint.
Once all required landmarks have been detected, the sensor is rotated parallel to the midline of the body. This is how ultrasonic waves travel along the biceps tendons.
Similar to the previous position, the bright hyperechoic head of the humerus is clearly visible. Above it are the fibers of the subcapsular muscle, and even higher is the biceps tendon. In this position, the doctor notes how the tendon connects to the joint.
To evaluate structures lengthwise and crosswise, the doctor rotates the surface of the sensor, changes the area of study and the angle of inclination. Clinically significant structures are:
- coracoid process;
- coracoacromial ligament;
- collarbone;
- intra-articular fluid;
- subdeltoid and subacromial bursae;
- supraspinatus muscle;
- capsular ligament.
The technique involves assessing echogenicity, clarity of contours, the presence of uncharacteristic inclusions in tissues, volume and size of formations.
An important diagnostic point is to perform an ultrasound of the shoulder when the patient’s arm position changes. The doctor may ask you to lift the limb up, move it back, or rotate the surface of the arm and hand to the right and left. For ease of manipulation, a rotating chair is used. To exclude bilateral damage, the doctor conducts an examination of a healthy joint.
Indications for use
Ultrasound of the shoulder joints is recommended in the following cases:
- the presence of pain and stiffness of unknown etiology in the shoulder;
- compaction of the tissues that make up the shoulder;
- change in the shape of the shoulder joint, its redness, swelling;
- suspected shoulder injury;
- dynamic monitoring of the progress of treatment;
- control examination during medical examination of patients;
- determining the need for radiography, MRI, scintigraphy;
- clarification of the state of anatomical structures before surgical interventions, punctures of the shoulder joint.
The high safety of the procedure virtually eliminates the presence of contraindications. The only limitation is severe pain in the joint, which can intensify when the sensor presses on the damaged area. In this case, it is rational to use other diagnostic methods, most often radiation.