Cytological analysis (from the Greek “cytos” - cell) is a study of the number, structure and shape of cells and intercellular components obtained from a living organism under an optical microscope. It allows you to identify pathological changes in the early stages and clarify their localization quickly enough, unlike other instrumental methods.
Cytological analysis is one of the most common diagnostic methods in gynecology and obstetrics.
Cytological analysis: what is it in gynecology
In a women's health clinic, various fluids (vaginal and menstrual discharge, urine) and (more often) the surface layers of cells that are taken from various parts of the reproductive system are subjected to cytological examination.
For example:
- vulva;
- vagina;
- cervix and cervical canal (internal canal of the cervix);
- internal cavity of the uterus;
- fallopian tubes;
- ovaries.
For cytology of the external parts (up to the uterus), freely exfoliated layers of cells are required, so this study is a fairly painless, quick (from several minutes during surgery to several days during a routine examination) and mass methods recommended for annual routine examination of women over 18 ( subject to the onset of sexual activity) or 30 to 65 years.
Representatives of risk groups for oncology are examined 2 times a year; cancer patients undergoing treatment and endocrinological patients – more often, according to indications.
To study the cellular composition of deeper organs, additional measures are required:
- endoscopy (uterus);
- organ punctures;
- swabs and impressions obtained during laparoscopy, open incision or during surgical operations.
Cytology smear includes the examination of the superficial (epithelium) and middle (mesothelium) layers of organs, as well as other included components, and is used to solve several problems.
They are:
- Assessment of hormonal status: study of the function of the ovaries and other glands; identification of decreased or increased production of individual hormones; searching for the causes of menstrual irregularities or infertility; Establishment of risk groups for oncology according to the degree of disturbance of estrogenic activity.
- Evaluation of the effectiveness of hormonal therapy.
- Search for atypical (not typical for the norm or this phase of the cycle) cells for the purpose of: diagnosing inflammation; detection of infections (including oncogenic forms of cytomegalovirus and papillomavirus); detection of precancerous and cancerous conditions.
Cytology analysis in gynecology helps to identify atypical cells, for example, cytomegalovirus.
- Assessment of the course of pregnancy: identification of dysbiosis; detection of inflammation; diagnosis of hormonal disorders; detection of damage to the membranes; diagnosis of fetal hypoxia; diagnosis of miscarriage, post-term pregnancy and intrauterine fetal death.
- Monitoring the effectiveness of anti-cancer therapy (based on the degree of damage to malignant cells).
- Monitoring the dynamics of wound healing.
- During operations to assess the nature of the pathology, the presence of tumor cells around the remote site and other urgent tasks.
Cytology analysis in gynecology is one of the most informative studies (for example, when establishing hormonal activity, cytology successfully competes with a blood test), however, the degree of its reliability is directly dependent on the qualifications of the doctor taking the material, on the strict adherence to the rules of staining and sample preparation and on the correct choice of fence location.
Therefore, the method requires systematic repetition, and if deviations are detected, supplementation with a comprehensive examination.
Types of cytological tests
Cytological analysis has been known in gynecology since the beginning of the 20th century, when the Greek physician Georgios Papanikolaou first used it for the early diagnosis of cervical cancer. Several new methods have now been developed that show improved reliability.
The procedure for carrying out manipulations when collecting material remains common to all these types; the differences relate to the methods of preparation, processing and analysis of the sample taken.
For example:
- The Papanicolaou test (PAP or PAP test) is the most common in the world and economically quite low-cost method, including alcohol fixation and step-by-step staining of the sample. Papanicolaou fixation helps prevent cell deformation, and the use of different dyes helps distinguish their types. The introduction of the Pap test into routine screening made it possible to reduce the increase in the incidence of cervical cancer by 80% (provided that regular examinations are observed). The reliability of the method for detecting dysplasia and cancer is about 60%.
- Romanovsky staining (Leishman modification) is a variation of the PAP test developed in Russia. The method requires highly qualified and experienced morphologist researchers.
- Liquid cytology is a more modern and more reliable research method that does not require a complex multi-stage staining procedure and minimizes manual work. Therefore, with liquid-based cytology, the likelihood of sample spoilage during preparation is minimized. The method includes keeping in a stabilizing liquid medium and subsequent centrifugation; Staining for liquid cytoanalysis requires the use of special dyes. The sensitivity of the liquid version of the analysis reaches 95%. The method also allows you to determine one of the markers of the presence of papillomavirus and conduct DNA studies. The liquid test is used mainly for the diagnosis of atypical cells in oncology, since due to the removal of many components of the sample during centrifugation, the value of the method for studying other diseases decreases.
- Rapid cytology – used for urgent assessment in the absence of the necessary fixation and staining components. The smear is applied to a dry glass slide, dried and immediately examined. The method has a high error.
The examination of the prepared sample is traditionally carried out visually by a cytologist using a powerful microscope, but in recent years hardware analysis has also appeared.
Differences between cytological and histological analyzes
Sometimes diagnosticians need to study not individual cells, but their relative position and the nature of the intercellular space. In this case, the patient is sent for histology (from the Greek “histos” - tissue) - collection and further examination of a small fragment of tissue (structurally and functionally related group of cells).
Features of histological examination:
- refers to biopsy methods;
- requires more complex training;
- carried out in a hospital;
- carried out under anesthesia;
- differs in a more labor-intensive aiming technique when taking;
- requires complex processing of selected material;
- hardware study required.
Tissue sampling is not indicated in the presence of very small foci of the detected lesion.
Histology is commonly used to diagnose human papillomavirus (HPV) and the level and stage of cancer.
Types of oncocytology
Oncocytology is performed by three diagnostic measures:
- Cytology with Leishman staining is a widely used method. It is used in most cases in antenatal clinics.
- Pap test (Papanicolaou smear) - the technique has gained popularity in private laboratory institutions and abroad. The degree of reliability of this diagnostic method is significantly ahead of the first type. The analysis shows a complex level of staining of the smear.
- Liquid cytology is a modern diagnostic method. Equipment for diagnostics is available in rare laboratories. The technique guarantees increased information content and reliability. Biotissues are collected into a special microflora (liquid) for further examination. The cells are then purified and concentrated to a fine, smooth surface. This way, the mucous epithelial tissues do not dry out when transported to a medical facility for microscopy. Thanks to this property, the accuracy of the resulting information increases.
The first two points are actively used by gynecologists and oncologists during examinations of patients. For the procedure you will need two glasses. One is designed for the analysis of the exocervix, and the other is for the analysis of the endocervix. To prescribe a referral for diagnostics, the doctor indicates the data of adults:
- FULL NAME;
- age;
- address;
- established diagnosis;
- period of the last menstrual cycle;
- chosen treatment technique;
- biopsy site.
The biomaterial is collected using a cytobrush. The prepared products are placed in personal packaging and sent to the laboratory within two days.
Differences between cytological examination and analysis for tumor markers
Tumor markers are specific protein molecules that can be produced by both altered and healthy cells of the body in the presence of disorders.
For example:
- inflammatory process;
- benign formations;
- when smoking;
- when taking medications;
- during pregnancy, menstruation and other physiological changes;
- depends on age.
Therefore, the marker test is also not 100% reliable. The analysis requires examination of venous blood, urine and other fluids.
The objectives of the study are similar to the cytology analysis:
- identifying the presence of a tumor and determining its nature (oncological or benign);
- assessment of the effectiveness of anticancer therapy;
- search for metastases and relapses.
Testing for tumor markers is used for women at risk for cancers of the reproductive system, digestive system and other organs and is not used for preventive examination. Sometimes the method is used to clarify the results of a cytological test.
Many tumor markers identify different diseases, so this test requires a comprehensive examination.
The advantage of the test for gynecology is the ability to determine changes in organs above the cervix (ovaries, uterus, fallopian tubes). The test for tumor markers requires more careful preparation of the patient due to the high sensitivity of the test subjects to physiological fluctuations.
Differences from microbiological analysis (smear for flora)
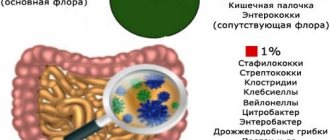
A smear from the vagina, cervical canal, urethra and rectum for microflora (pathogenic, symbiotic and opportunistic microorganisms) is performed through manipulations similar to a smear for cytology, and is included in a routine gynecological examination, recommended for every woman every six months.
Usually both types of smears are taken at the same time. Microbiological analysis may require culture on a nutrient medium. Microscopy for bacterioflora is carried out using another staining method (Gram staining).
Indications
Cytology analysis in gynecology is part of the screening examination of the adult female population in many countries of the world. A routine cytology test is mandatory for all women over 18 (this age decreases with earlier onset of sexual activity) and under 65 years of age.
At an older age (due to a decrease in estrogen levels and a decrease in the reliability of the result), a smear is prescribed at the discretion of the gynecologist. The group of special attention includes women over 30 years of age.
For women of screening age, in the absence of positive test results (that is, in the absence of detected pathologies, stage 1 cytogram) for 2 years, the planned date is postponed every 2 years, with a negative result within 3 tests - for 3 years.
Indications for unscheduled cytological examination may include:
- pregnancy planning;
- before installing an intrauterine device;
- frequent change of sexual partners;
- use of hormonal contraceptives and other sex hormone preparations;
- irregular periods or amenorrhea (lack of menstruation);
- infertility;
- heavy or unusual vaginal discharge;
- itching, burning and other unpleasant sensations in the genital area;
- genital herpes and condylomas;
- presence of cancer patients among ancestors and relatives;
- the presence of provoking factors (smoking, frequent alcohol consumption, living in environmentally unfavorable areas, early onset of sexual activity, weakened immunity, the presence of other viral diseases, a history of genital cancer);
- frequent childbirth (from 2) and abortions;
- history of radiation exposure, including radio wave therapy;
- obesity;
- cervical erosion;
- diabetes.
Causes
Doctors associate the appearance of the disease in question with several risk factors. They must be detected promptly at every gynecological examination. Atypical endometrial hyperplasia occurs when there is an imbalance in hormones (gestagens decrease, estrogen levels increase). The reasons for this phenomenon are considered:
- tumor of the ovaries responsible for the production of hormones;
- follicular atresia. This condition provokes a lack of ovulation;
- hyperactivity of the adrenal cortex (Cushing's disease);
- disruptions caused by hormone treatment. Tamoxifen has a particularly negative effect;
- increased activity of the pituitary gland due to the production of gonadotropic hormone.
Doctors often detect adenomatous hyperplasia against the background of certain hormonal imbalances:
- hypertension;
- obesity;
- thyroid diseases;
- diabetes;
- liver damage accompanied by slow utilization of estrogen (cirrhosis, hepatitis).
Test portability
A screening cytological study is carried out on cells no further than the outer part of the cervical canal and is a non-invasive method.
Taking freely exfoliated cells from the vagina does not cause discomfort; the patient experiences some discomfort when taking material from the surface of the cervix and from its canal, however, this procedure is short-term and also does not involve penetration into the deep layers.
To reduce discomfort, the gynecologist can pre-warm the instruments in hot water. This study is rightfully considered a trivial medical procedure and should not cause concern.
Women who are forced to undergo frequent smears for cytology (for example, cancer patients) get used to these manipulations very quickly, which should serve as excellent evidence for women who avoid this test due to fear of pain or possible complications.
Preliminary preparation
The reliability of the results of a cytological examination largely depends on proper preparation and a well-chosen time for visiting a gynecologist.
A smear should not be taken under the following conditions:
- the presence of an identified inflammatory (general or local) condition;
- during menstruation, a week after its end and the same amount before the start;
- during pregnancy - according to indications;
- less than 2 days after the previous gynecological examination or colposcopy;
- less than 2 days after the last sexual intercourse, douching or use of any vaginal products (medicines, lubricants, ultrasound gels and the like);
- earlier than a few hours after visiting the toilet;
- less than a week after finishing antibiotics.
What does an inflammation cytogram mean and how to treat it?
Usually, in the case of a cytogram with signs of inflammation with reactive or degenerative changes in the epithelium, based on one analysis, a diagnosis is not made, because the disorders can be complex. For example, if it is a herpes or papilloma virus, the nucleus of the epithelial cells may be increased in size. But such changes can also be detected with other problems. Therefore, when making a diagnosis, the gynecologist takes into account not only the results of the cytogram, but also the patient’s age, the phase of the menstrual cycle when the smear was taken, concomitant diseases, anamnesis, complaints, other symptoms and the results of a visual gynecological examination on the chair. Therefore, treatment is prescribed in accordance with the diagnosis made on the basis of all the above factors.
How long should I wait for an answer?
In emergency situations (for example, during surgery), the cytology result is provided to the surgeon within a few minutes before the operation is completed. Waiting for a response during a routine screening examination at a antenatal clinic takes up to 2 weeks, since in this case the time to prepare the result depends on the workload of the institution and does not require urgency.
In private clinics, an answer can be given within 1-3 days, but it should be remembered that the most accurate result of a cytological study can be obtained by following all stages of sample preparation, which takes about 7 days outside the cito (“urgent”) mode.
Decoding the results
Cytological analysis in gynecology ends with the issuance of results in the form of a cytogram.
The cytogram contains information about one of the 5 stages of disease development according to the Bethesda system from 2014:
- No deviations. Negative test result.
- Minor changes in cell morphology; There are no atypical cells. As a rule, this stage indicates the presence of inflammation, the detection of which will require additional examination measures.
- Some cells contain nuclear deformations, which indicates their tendency to be atypical. The stage is characteristic of cervical dysplasia and erosion and requires histological examination to exclude precancerous conditions.
- The presence of cells with malignant deformations: enlarged nucleus; altered cytoplasm; the structure of chromosomes is changed. This stage indicates a precancerous level of dysplasia.
- The presence of cells with malignant changes in large numbers.
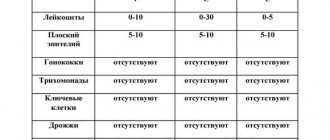
In addition to epithelial cells, the cytogram describes other components of the smear:
- the degree of microbiological cleanliness of the vagina (the norm is grades 1 and 2; grades 3 and 4 indicate infectious inflammation);
- the number of leukocytes (white blood cells that appear in a smear during various types of inflammation; normally - up to 10 pieces in a smear from the surface of the cervix, up to 30 - from the urethra);
- presence of mucus (norm – moderate amount);
- the presence of bacteria and fungi (microorganisms must be absent);
- content of flat epithelial cells (no more than 10 pieces).
Disorders detected using a cytogram
Cytology analysis in gynecology is an informative method that allows you to diagnose many disorders at the initial stage. In addition to different degrees of progression of malignant processes, a cytogram helps to detect a wide range of other pathologies.
Infectious diseases:
- bacterial (chlamydia - most often passes without symptoms; gonorrhea; trichomoniasis - accompanied by greenish discharge, itching and discomfort);
- viral (human papillomavirus infection and genital herpes); may be accompanied by the appearance of condylomas (warts) on the genitals; other studies will be required to establish the degree of oncological danger of the identified form of the virus;
- fungal (usually from the genus Candida); yeast overgrowth is usually accompanied by inflammation, itching, burning, and specific whitish discharge.
Benign formations and dysplasia (cell deformations) are dangerous due to the possibility of degeneration into cancer:
- polyps - cell proliferation;
- leukoplakia (hyperkeratosis) – deformation of the epithelium (mucous lining) of the cervix;
- erythroplakia - atrophy of the cells of the upper layer, can be observed with low estrogen;
- dysplasia - changes in the structure of cervical epithelial cells (refers to precancerous conditions).
Inflammations of a non-infectious nature (for example, caused by decompensated diabetes mellitus).
Hormonal status and its deviations:
- high estrogen levels are an oncological risk factor for diseases of the genital organs and mammary glands;
- reduced amounts of estrogen are a possible cause of infertility and instability of the menstrual cycle;
- increased levels of androgens - male sex hormones;
- deviations in prolactin levels;
- discrepancy between hormonal activity and cycle phase.
Additional examinations that may be prescribed if 2-5 stages are detected in the cytogram:
- Ultrasound;
- MRI;
- CT;
- radiography;
- histology;
- bacteriological analysis and bacterial culture;
- endoscopy of the uterus (hysteroscopy);
- extended colposcopy;
- PCR (to determine the type and form of the virus);
- ELISA (enzyme immunoassay of blood);
- blood test for tumor markers and TORCH infections;
- blood test for hormones.
Table 1:
| Phenomena | Signs | Duration | Frequency of occurrence |
| Norm |
| 1-2 days after the procedure | Often |
| Dangerous |
| More than 3 days | Rarely |
Table 2:
| Causes | Possible consequences | Actions |
| Pass on their own |
|
|
| Seeking urgent medical attention |
What changes are possible?
Benign changes may include:
- Detection of trichomonas, candida fungi, coccal infections, anomalies caused by infection with the herpes virus.
- Cellular atypia provoked by inflammatory reactions: metaplasia, parakeratosis, keratosis.
- Atrophic changes in epithelial cells in combination with inflammation: hyperkeratosis, colpitis, metaplasia.
Dysplastic changes and atypia suggest the following conditions:
- Atypia of unknown origin (ASC-US).
- High risk of presence of cancer cells in the material (HSIL).
- Precancerous atypia: varying degrees of dysplasia.
If cancer cells are detected, it is necessary to prescribe additional examination methods and a subsequent course of therapeutic correction (conservative or surgical treatment) with constant cytological monitoring.
Mixed flora: a variant of the norm or a violation?
Where can I get a smear for cytology?
Cytology analysis in gynecology is one of the mass types of examination of the female population in Russia.
According to the compulsory health insurance program, a smear for cytology is taken at the antenatal clinic at the place of residence.
Almost all private clinics in Russia offer similar services. Large institutions have their own laboratory facilities for testing samples, while smaller ones send samples to intermediary centers.
Can atypical endometrial hyperplasia develop into cancer?
A feature of atypical endometrial hyperplasia from oncology (early stage) is the lack of penetration of the growth through the edges of the plate separating the surface and stroma. Mutating cells multiply in the area of the upper layer of the endometrium. They do not penetrate to blood nodes or lymph nodes.
Atypical hyperplasia in gynecology is considered as the beginning of a malignant process (it is called endometrial precancer). There is a risk of developing into cancer in the absence of adequate therapy.
Normal and dangerous complications after cytological examination
To prevent complications after collecting material for cytoanalysis, you should follow several simple rules:
- for 1-2 days, limit yourself to a shower when taking water procedures;
- Abstain from sexual activity, douching, using a tampon and other intravaginal products for at least 1 week.
Features of cytological examination in pregnant women
During a normal pregnancy, a cytological smear is taken 3 times - at registration, at the 30th and 36th week. The main goal of the study is in this case to detect infections dangerous to the fetus, as well as to identify atypical cells, which, subject to predisposition, first appear during pregnancy.
Contraindications to manipulation are increased uterine tone and the threat of miscarriage.
The life of a modern active woman includes many factors that can negatively affect her health, therefore, for timely diagnosis of possible pathologies, it is extremely necessary to be regularly examined by specialists. Cytology analysis in gynecology is one of the most accessible, simple and effective methods for early detection of disorders.
Author of the article: lyubov_a
Article design: Oleg Lozinsky
Scheme of oncocytology
The method of taking a smear is painless. The procedure is performed by a doctor during an examination of the patient by a gynecologist in a gynecological chair. Initially, specialized magnifying mirrors are inserted into the vagina, then a piece of epithelium is removed from the membranes of the uterine cervix using a small spatula or using a special cytobrush. A cell sample is then taken from the cervical canal using a small cotton swab. The shelf life of the biological tissue is 14 days.
The collected material is applied to a special glass for further microscopic manipulations (Pap test) or placed in a special liquid for liquid-based cytology. The analysis has no painful symptoms and is absolutely painless. During the study, the tissues of internal organs are not injured. The initial examination may be accompanied by slight discomfort.
Oncocytology shows small discharge with blood clots. Bleeding goes away within two days and does not require treatment. When a woman passes childbearing age, diseases of the genital organs do not disappear. Seeing a doctor and undergoing diagnostics at this age reveals advanced and irreversible pathological processes. It is difficult to cure cancerous tumors in the later stages of development.
Pregnancy is a serious stressor on the female body. Increased hormonal levels and stress activate the progression of many oncological and non-oncological diseases. When registering a pregnant woman, the doctor must take a smear for oncocytology. If the pregnancy is stable, tests are performed again in the second and third trimesters. It is recommended to undergo examination during pregnancy planning. This will allow you to accurately prevent disturbances in fetal development.
In developing inflammatory processes, a smear is not taken after oncocytology to avoid obtaining distorted information. In such situations, the doctor takes a smear and scraping to check the development of viral infections and pathological diseases transmitted through sexual contact. The patient then undergoes a course of therapy. After recovery, oncocytology tests are repeated.