Why does antibody level change?
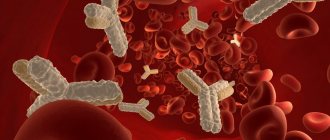
Thanks to the immunogram, it is possible to present a complete clinical picture of the state of the antibodies.
Just by the presence of certain cells of the immune system, it is possible to determine the disease even without identifying the pathogen. The reasons why a child has an increased level of a special protein produced by the immune system are different. Immunoglobulin M is elevated if:
- Bacterial, viral, fungal, parasitic infection has occurred.
- There are serious liver pathologies.
- There are dysfunctions in the hematopoietic system.
- There is purulent inflammation of the respiratory organs and gastrointestinal tract.
- Diseases of the ligamentous apparatus develop.
Immunoglobulin G is increased when:
- Serious systemic hereditary diseases.
- Complete immunodeficiency syndrome - AIDS.
- Recurrent and chronic infections.
- Helminthic infestations.
- In the recovery stage after primary infection.
- Transference of secondary infection and in some other cases.
Immunoglobulin G is also reduced in case of immunodeficiencies of various types, with a missing number of cytokines in cells, a malfunction in the functioning of isotope switching, a decrease in the activity of one’s own killer cells, and for a number of other reasons.
Elevated immunoglobulin E in childhood can be:
- For rhinitis, dermatitis, asthma, allergic origin.
- For allergic reactions to food and drug antigens.
- For pathological disorders of the immune system.
- When infected with parasites and in some other cases.
Low immunoglobulin E usually occurs as a result of acquired or congenital immunodeficiency. Disorder of hematopoietic processes can also reduce this indicator. The presence of non-benign neoplasms in the body affects the decrease in ige. In such pathologies, all measures should be aimed at increasing the level of class E antibodies.
If immunoglobulin E is elevated, only a qualified doctor can give competent recommendations on what to do in such a situation. The first thing you need to do is to definitely show the child to an allergist and immunologist. As a rule, you will need to do skin prick tests for allergens.
Normal immunoglobulin values in children
A slight increase in immunoglobulin E can be observed in spring and summer, which is due to flowering plants. And the lowest rate occurs in winter. The level of immunoglobulin E in children increases systematically and reaches its maximum value by adolescence. Then there is a gradual decrease, and the smallest indicator is observed in older people. An interesting fact is that a certain concentration of antibodies is already detected in the blood of the embryo by approximately the 12th week of formation.
Immunoglobulin E in children must be maintained at normal levels. Many people are susceptible to allergic diseases at a young age due to insufficiently strong immunity. Immunoglobulin E normally in children should not exceed 70 kE/l. Normal immunoglobulin E in a child contributes to the full course of many life support processes.
Table with indicators of what the norm of special cells of class E should be in children:
Side effects
Most patients do not have negative reactions to the administration of the stimulant. In rare cases, an allergy, a reaction to immunoglobulin in a child in the form of hypersensitivity and anaphylactic shock may develop. Therefore, after using the medication, children should remain under the supervision of medical personnel for at least half an hour.
Redness and slight swelling may occur at the site of intramuscular injection. These signs do not cause serious discomfort and go away on their own and do not require additional therapy.
After drips, children experienced the following manifestations:
- headache;
- chills;
- dyspeptic disorders;
- backache;
- muscle stiffness;
- deterioration of kidney function.
Cases of overdose with a drug to enhance immunity have not been described. When using an excessive amount of immunoglobulin, an increase in adverse reactions is expected. Treatment in this case is symptomatic.
Standards for immunoglobulin A content
Due to the fact that our immune system is imperfect from birth, for some time infants’ own IgA is not produced by the body, but is supplied with mother’s milk (this is one of the reasons why breastfeeding is so important in the early stages). The normal level of immunoglobulin A in children under one year of age is 0.83 g/l
The standards are further distributed as follows:
| Age | Norm |
| 1-4 years | 0.2-1.0 g/l; |
| 4-7 years | 0.27-1.95 g/l; |
| 7-10 years | 0.34-3.05 g/l; |
| 10-12 years | 0.53-2.04 g/l; |
| 12-14 years old | 0.58-3.58 g/l; |
| 14-16 years old | 0.47-2.49 g/l; |
| 16-20 years old | 0.61-3.48 g/l; |
| 20 years and older | 0.7-4.0 g/l. |
As can be seen from the standards, an adult has not only the highest upper limit of the permissible norm, but also the greatest variability of indicators. They can be associated both with the individual characteristics of the body and with the action of any irritants and vary slightly even within one day.
Immunoglobulin lgE increased causes
In most cases, an excess of total immunoglobulin E in the blood serum indicates the development of allergic diseases. The doctor takes venous blood and compares the results with the table value.
It is important not only to clarify the level of allergy indicator, but also to find out the clinical picture of the disease and study negative symptoms in detail. Increased levels develop not only against the background of hypersensitivity of the body after contact with an allergen, but also with other types of diseases
A high level of lgE indicates the development of the following diseases of an allergic nature:
- hay fever;
- bronchopulmonary aspergillosis of allergic origin;
- atopic dermatitis;
- hives;
- atopic bronchial asthma;
- allergic rhinitis;
- negative reaction to certain foods;
- drug allergies;
- angioedema;
- allergic conjunctivitis;
- Lyell's syndrome;
- contact dermatitis;
- allergic gastroenteropathy.
Increased levels in the absence of signs of allergy are one of the signs of the development of the following diseases:
- thymic aplasia;
- helminthic infestations;
- myeloma;
- hyper-lgE syndrome.
On a note! Based on the results of research, doctors have found that with food allergies, the body’s sensitivity to microparticles of pollen from certain plants, the level of immunoglobulin E increases more actively than with a pronounced reaction to mold spores and house dust. With a negative response to one type of allergen, the indicators often remain within the reference values or are slightly increased.
Immunoglobulin E is normal in children
In this article we will talk about immunoglobulin E (IgE), its general characteristics in children, consider the possible causes of increased immunoglobulin E in children, talk about what immunoglobulin E shows if it is elevated in a child and what treatment is required in this case.
Immunoglobulin E in children and adults is found on the surface of certain types of leukocytes (basophils) and mast cells. Its main purpose is to participate in the work of antiparasitic immunity (and therefore in the development of allergic reactions).
Normally, its content in the blood is minimal. In the blood serum, the immunoglobulin E level ranges from 30 to 240 mcg/l. But immunoglobulin e levels fluctuate throughout the year: the highest level is observed in May, and the lowest is usually in December. It's not difficult to explain. In spring, particularly in May, most plants actively bloom, saturating the air with pollen (which, as is known, is a fairly aggressive allergen).
It should be taken into account that each age has its own norms for the production of immunoglobulin E. As the child grows older, the production of immunoglobulin in the body increases, this is normal. An increase or decrease in the level of IgE in the blood, sharply exceeding the age norm, may indicate the development of certain diseases.
High immunoglobulin E in a child
If a child has high immunoglobulin E, this may indicate:
- hay fever;
- hives;
- infection with parasites (toxoplasmosis, worms, schistosomes, trichinosis, echinococcus, amoebic invasion);
- atopic dermatitis;
- allergic rhinitis;
- food intolerance;
- atopic bronchial asthma;
- drug allergies;
- hyper-IgE syndrome;
- thymic aplasia;
- myeloma;
- allergic diseases of other types.
Low immunoglobulin E in a child
- hereditary hypogammaglobulinemia;
- some types of tumors;
- Louis-Bar syndrome (ataxia-telangiectasia).
To determine the level of immunoglobulin, special laboratory tests of blood (blood serum) are used.
To ensure reliable results, it is important to properly prepare for blood sampling for analysis. So, in the morning before the test you can’t eat, blood is donated on an empty stomach
The day before (or better a few days), exclude fatty, spicy, intestinal-irritating dishes from the menu.
Since an increase in the level of immunoglobulin E is associated with the influence of allergens, in order to reduce it, it is necessary to find out which substance the reaction is manifested to and, if possible, limit the contact of the allergen and the child (patient) as much as possible. It would not be superfluous to preventively limit the level of household physical and chemical allergens (animal hair, pollen, household chemicals, etc.), adjusting the diet towards hypoallergenicity.
Some experts note a normalization of the level of immunoglobulin E when consuming dietary supplements containing spirulina. Despite a lot of positive
A good result comes from following a healthy lifestyle, a nutritious diet, playing sports (and an active lifestyle in general), walking in the fresh air, etc. But still, the main way to reduce immunoglobulin E is to avoid contact with the allergen.
- Privacy Policy
- Terms of use
- Copyright holders
- Adenoma
- Uncategorized
- Gynecology
- Thrush
- About blood
- Psoriasis
- Cellulite
- Ovaries
Preparation for analysis and collection of material
The level of immunoglobulin A (IgA) is determined in venous blood serum. The procedure for collecting biomaterial is carried out in the morning, on an empty stomach. It is allowed to donate blood during the day, 3-4 hours after eating. The day before the analysis, you must refrain from drinking alcoholic beverages and increased physical and psycho-emotional stress. During the last 3 hours you should stop smoking. The results of the test may be affected by taking certain medications, such as oral contraceptives, so a week before donating blood, you should discuss with your doctor the need to temporarily discontinue medications. Most often, blood is taken from the ulnar vein using a puncture method. Stored and transported in a test tube without an anticoagulant or with a coagulation activator.
Immunoglobulin A (IgA) in the blood is examined using the immunochemiluminescent or immunoturbidimetric method. Most laboratories use the second method. Specific antibodies are introduced into a test tube with blood serum, immunoglobulin A forms complexes with them, as a result of which the turbidity of the solution increases. Then, using a photometer, the scattering of light is determined, and the concentration of the glycoprotein under study is calculated. The entire study takes about 2 hours, the results are prepared the next day after blood donation.
Immunoglobulin value
Immunoglobulin (Ig) is a special protein compound responsible for the production of antibodies.
The protective mechanism consists of the following functions:
- antigen recognition;
- formation of an immune response;
- developing immunity to re-infection;
- rejection of foreign tissue.
The following groups of immunoglobulins are distinguished: lgA, lgE, lgD, lgG, lgM.
Immunoglobulin A is responsible for protecting the mucous membrane of the respiratory and genitourinary systems. Large amounts of IgA are found in saliva, colostrum, tears and secretions of the genitourinary organs.
An increase in immunoglobulin A is observed in cancer, autoimmune pathologies, and diseases of the digestive tract. A decrease in IgA in a child may be due to impaired renal function or anemia.
The main task of Ig E is to form an adequate response to the allergen. Its production begins already during intrauterine development of the fetus. An increased level of IgE is characteristic of hay fever, urticaria, and helminthiasis. A decrease in this indicator may indicate a possible oncological tumor.
Ig G. The main task is to develop an immune response to bacterial and viral diseases. IgG testing is of particular importance in case of frequent recurrent diseases of the child. An increased value is typical for chronic infections, viral liver damage (hepatitis), and autoimmune diseases. A decrease in Ig G is observed in cases of poisoning, muscular dystrophy, and damage to the lymphatic system.
Immunoglobulin M, together with IgG, is responsible for the development of the immune response during bacterial infection. But unlike IgG, immunoglobulin M forms the primary response to infection. An increase in IgM concentration is observed during the initial latent stage of development of a bacterial infection, fungal infection, or a disease of viral etiology. Low levels of immunoglobulin are observed during the postoperative recovery period.
The functions of IgD are not yet fully understood. Its concentration in the blood is less than 1% of the total amount of immunoglobulins and has no clinical significance.
Uncertainty of results
To obtain reliable results, you must adhere to the basic rules for all tests. The blood test is highly accurate, but errors are possible. The results of the study can be distorted by alcohol abuse and taking medications (immunosuppressants, estrogens, gold preparations), severe kidney disease, burns, removal of the spleen, and exposure to ionizing radiation. Immunoglobulin A may be lowered if a person has been vaccinated in the last 6 months or has taken immunoglobulins.
Immunoglobulins A, M,
G , E
(Immunoglobulin A, M, G, E)
What is this :
What's the point:
Depending on the time, place and type of pathogen, IGs are divided into classes:
Immunoglobulin A (IgA)
– are found in two forms: serum (in the blood, 10-15% of the total number of IGs) and secretory (in the bronchial and intestinal mucosa, sweat, tear fluid, saliva, colostrum). Secretory IgA is a component (along with its other elements, such as phagocytes, lymphocytes, cytokines and the complement system).
IgA is the border troops of our body, they give the first battle to all enemies who violate the borders of our homeland-body. At least 50% of immune resources are barrier immunity. “Don’t be afraid of heat or cold, harden yourself like steel!” – this is about training “border troops” for this type of immunity. IgA also protects our mucous membranes from the action of proteases (enzymes that break down protein bonds are found in the gastrointestinal tract and are also secreted by microbes).
IgA makes up 10-15% of the total number of Ig in the blood.
Norm: 0.7 – 4
g/l (there may be different reference values in laboratories).
Promotion
:
- oncology (carcinoma - a tumor of epithelial cells, myeloma - a tumor of plasma cells, chronic lymphocytosis - a tumor of B-lymphocytes);
- autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis, glomerulonephritis);
- chronic infections;
- cirrhosis of the liver.
Decline
:
- selective immunodeficiency IgA (1:400 in the population);
- celiac disease;
- absence of spleen;
- AIDS;
- congenital telangiectasia (persistent dilatation of skin vessels).
Immunoglobulins M (Ig M)
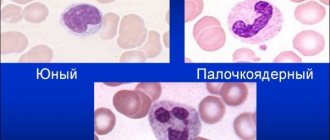
- are formed when B lymphocytes first encounter an enemy antigen and say in surprise: what the hell is this?! That is, this is the primary response to the antigen (apparently, swearing, that’s why they call them M). IgM consists of five monomers (and not one or two, unlike other IGs), one of them is in the shape of the letter Y, so it lifts the antigen “onto the pitchforks”, forming a complex with it. IgM rises in the first weeks of infection and is then replaced by IgG, which provides long-term protection. Thus, IgM is the main indicator of recent (new) infection.
IgM constitutes 5-10% of the total number of Ig in the blood.
Norm: 0.5-2.5
g/l (there may be different reference values in laboratories)
Promotion
:
- liver diseases;
- chronic infections (especially fungal);
- chronic and acute lymphocytic leukemia.
Decline
:
- neonatal period (up to about 6 months);
- amyloidosis;
- multiple myeloma (non-IgM);
- treatment with cytostatics.
Immunoglobulin G (IgG)
–
provide long-term protection against re-infection. If IgM, during a primary infection, labels all antigens hastily and inaccurately (and this is costly), then IgG, with the help of memory T-lymphocytes, is trained to label a specific pathogen (rubella, chickenpox, measles, etc.) leisurely and accurately. Their production is more elaborate and takes longer, so they appear several weeks later than IgM. IgG constantly circulates in the blood and with repeated infection, their number increases. Due to its small size, IgG is the only one of all IGs that passes the placenta and provides immunity to the fetus and newborn for up to 6 months.
They are an indicator of a previous (familiar) infection.
IgG constitutes 70-80% of the total number of IGs in the blood.
Norm: 7-16 g/l (there may be different reference values in laboratories).
Promotion
:
- recovery from primary infection;
- chronic infections;
- liver diseases;
- autoimmune diseases;
- chronic lymphocytosis;
- sarcoidosis (granuloma nodules, most often in the lungs and liver).
Decline
:
- common variable immunodeficiency;
- protein deficiency syndromes;
- splenectomy;
- pregnancy.
Immunoglobulins E (Ig E)
—
they have two main functions:
Normal: up to 100 IU/ml (there may be different reference values in laboratories).
Increase
:
Decrease:
- secondary or primary immunodeficiencies;
- ataxia-telangiectasia.
There are also Immunoglobulins
D ( IgD ),
the role of which has not yet been well studied; their participation in autoimmune reactions is assumed. IgDs make up 1% of the total number of IgDs in the blood.
What to do about it and what to pay attention to:
– the main task of a doctor is to answer the question: doctor, I often get colds, is my immunity weakened?!
The most common immunodeficiencies associated with impaired IH function:
- selective immunoglobulin A deficiency;
- common variable immunodeficiency;
- transient hypogammaglobulinemia in children and other, more rare, immunodeficiency conditions.
– determination of the level of IG – one of the analyzes of the immune system along with such studies as:
- and their phagocytic activity;
- complement system;
- level of T-lymphocytes and their subpopulations.
A note from life: you never develop immunity to rudeness. Be polite, don't strain yourself!
Viktor Yamshchikov, minimalist doctor
Serum immunoglobulin A is one of the subtypes of globulins in the blood. These are secretory antibodies that are mainly responsible for the humoral protection of the mucous membranes and skin. Immunoglobulin a increases sharply when viruses, microbes and infections appear in the body in the oral cavity, gastrointestinal tract, and respiratory tract. Group A antibodies bind all invading microbes and foreign substances, thereby preventing their further reproduction and spread to internal organs.
Answering the question of what immunoglobulin A is, we can give a specific explanation. This is one of the main factors in the body's primary immune response. However, these protective elements do not have immunological memory, which means that upon re-infection, new antibodies will be produced. That is why, when the doctor receives the results of a blood, saliva or urine test, where it is recorded that immunoglobulin A is elevated, the specialist has every reason to suspect that the patient is developing an acute inflammatory process in the body.
Let's talk in more detail about type A immunoglobulins, what should be the concentration of substances in a healthy person, and what can deviations in the level indicate?
The important role of immunoglobulin in the body
Immunoglobulin is found in human blood in very small quantities, and its half-life is 2-3 days in blood serum and 9-14 days in the skin.
When allergens enter the body, immunoglobulin Ig E interacts with them, and as a result of this interaction, complexes of specific antigens begin to form in the cells. As a result, calcium ions enter the affected cell, and biochemical processes are activated in it. This process is also accompanied by the release of biologically active substances, histamine and other toxic substances into the intercellular space, which leads to the appearance of a focus of inflammation.
Inflammation can manifest itself in the form of rhinitis, asthma, bronchitis, and skin rash. Collectively, foci of inflammation can cause a reaction in the form of anaphylactic shock.
Contraindications
Despite the fact that the drug is used to enhance immunity and provides benefits to the body, it has its contraindications. It is not recommended to drip, administer the solution intravenously or intramuscularly under the following conditions:
- increased sensitivity of the child to the active component;
- immunoglobulin A deficiency caused by the presence of antibodies in the body;
- exacerbation of chronic allergic reactions;
- renal failure;
- diabetes;
- the likelihood of developing anaphylactic shock due to blood products.
Before using the medication, it is important to take into account not only contraindications for use, but also the patient’s conditions in which the solution should be administered with extreme caution: recurrent migraines, heart failure. If therapy is necessary for a nursing woman, the baby should be temporarily weaned to prevent the medicine from entering his body without indications for this. For diseases caused by immunopathological processes, the solution is used only under the supervision of a physician.
Blood test for immunoglobulin
A blood test for immunoglobulin allows you to assess the condition and severity of an allergic disease, and, therefore, prescribe the correct treatment. Three days before taking blood for this study, it is necessary, if possible, to avoid unnecessary physical and emotional stress, and an hour before that, not to smoke.
A test for total immunoglobulin is prescribed for the following indications:
- helminthiases;
- hay fever;
- bronchial asthma;
- atopic dermatitis;
- eczema;
- drug and food allergies;
- children to assess the possible risk of developing atopic diseases in the presence of a hereditary predisposition.
In the case of an increased concentration of immunoglobulin in the blood, an additional examination may be prescribed to find out which disease caused such a reaction (if the disease is not yet known).
An increased level of immunoglobulin indicates hypersensitivity and predisposition to various types of allergic reactions. The concentration of this component also directly depends on how long the disease lasts, as well as on the number of previous contacts with allergens.
It has been noted that most often an increased concentration of immunoglobulin is observed in children who have allergies to food and pollen allergens. In children with allergies to dust and mold, this concentration is lower. Also, as statistics show, 75% of children whose parents have any allergic diseases have an exceeded normal level of immunoglobulin in the blood.
Indeed, we live in the age of allergies, everyone, young and old, suffers from it. Various unfavorable factors in the environment, as well as genetic predisposition - all this negatively affects our health and the health of our children. Therefore, if you have any allergic disease, an analysis of the concentration of immunoglobulin in the blood is mandatory. It has a high diagnostic value and can tell a lot about how strong the human body is and is able to fight various diseases. And early diagnosis of any ailment makes it possible to overcome it faster and better.
https://youtube.com/watch?v=yAeJCfOD2Rc
What other factors may distort the result?
In addition to the above, there are some other factors that can affect the result. They should be taken into account by the attending physician, who will evaluate the test result. These factors include primarily pregnancy, which usually results in low levels of immunoglobulin
. In addition, extensive burns, renal failure, drugs that lower immunity, and various types of radiation can reduce the concentration of IgA.
Factors that increase immunoglobulin A levels include certain medications (mainly antipsychotics, anticonvulsants, antidepressants and oral contraceptives), vaccinations given less than 6 months ago, and excessive physical, mental and emotional stress immediately before donating blood.
In some cases, immunoglobulin A deficiency is associated with a specific feature of the patient’s body - it produces antibodies to its own IgA protein. Such patients are at high risk of developing autoimmune diseases and infections. In addition, there is a risk of developing an anaphylactic reaction during blood transfusion or organ transplantation.
Immunoglobulin levels in children
The norms for the quantitative value of Ig levels in children, depending on age, are presented in the table.
Child's age | IgA | IgE | IgG | Ig M |
| Up to a year | less than 0.8 kU/l | 2 – 10 kU/l | 2.3-14.1 kU/l | 1.45 kel |
| 1 year – 5 years | 1 – 1.5 kU/l | 10-40 kE/l | 4.5-9.1 kU/l | 0.19 – 1.5 kU/l |
| 5 – 10 years | 0.2 – 3.75 kU/l | 40 – 60 kU/l | 5.7 – 14.7 kU/l | 0.3 – 2.1 kU/l |
| 10 – 15 years | 0.5 – 3.78 kU/l | 60 kE/l | 7.6-15.5 kU/l | 0.4 – 2.4 kU/l |
| Over 15 years old | 4.0 kU/l | up to 100 kE/l | 8 – 16 kU/l | 0.5 – 3 kU/l |
Situations often arise when the research results obtained are inaccurate.
In order to avoid this, you need to know the rules for preparing for testing:
- Blood donation is carried out in the morning, on an empty stomach. Dinner the night before should not be later than 6 pm.
- Before the examination, it is recommended to follow a strict diet. Fried and fatty foods, carbonated drinks, and seasonings are excluded from the diet.
- It is known that the normal level of immunoglobulin is distorted during severe physical fatigue and nervous stress. For this reason, it is not recommended to donate blood after sports training or exams.
- Distortion of test results is possible due to a temporary decrease in immunity after an acute respiratory infection or viral infection. There should be at least 15 days between complete recovery and immunogram control.
A definitive diagnosis is never made based on the results of an immunoglobulin test. If a suspicious conclusion from a clinical study is received, an additional examination is prescribed. First of all, this is a test for helminths, which can give an overestimated value of Ig E and M. When checking general and biochemical blood tests, the presence of infection in the body (leukocytosis in the CBC) and the functioning of internal organs (liver, kidneys) are revealed.
If a detailed examination did not reveal diseases characterized by changes in Ig levels, then attention should be paid to increasing the child’s immunity. This requires a healthy lifestyle with prolonged exposure to fresh air, taking multivitamins and immunostimulating medications.
The diet should include a large amount of vegetables and fruits, spirulina. It is recommended to exclude products that are considered classic allergens (honey, citrus fruits, egg yolk). Distortion of IgE in many cases is caused by hidden food allergies.
A month after the start of such treatment, the immunogram is re-checked. If the indicators do not change, then a more detailed diagnosis of the whole organism is carried out, including magnetic resonance imaging and computed tomography.
Monitoring the level of immunoglobulins often helps to make an accurate diagnosis in situations where standard research methods do not bring the desired result.
Regular checks of this analysis should be carried out at least once a year. In this case, the chance of detecting the disease at the initial stage of its development increases. And this significantly increases the child’s chances of a full recovery.
Directions for use and dosage
The instructions for use included with the drug allow immunoglobulin to be administered to children by injection in three different ways. The method of use is selected in accordance with the indications, general condition of the body, concomitant diseases, the baby’s age and medical history.
Unlike adults, children are more sensitive to various types of medical procedures. Therefore, when a stimulant is administered, children often experience an increase in body temperature. Depending on the characteristics of the child, the thermometer readings can vary from 37 to 39 degrees or more. Therefore, all injections should be done exclusively in a medical facility so that, if necessary, the little patient can receive timely, qualified assistance.
Before using the medication, it is necessary to keep the solution in the ampoule at room temperature. If it contains cloudiness and foreign impurities, then such an injection cannot be used. When giving an injection, it is important to follow the rules of asepsis.
Intramuscularly
Intramuscular administration of the drug to children is carried out in the upper thigh or buttock. Infusions with this solution are prohibited. The liquid is drawn from the ampoule with a sterile disposable syringe, the needle lumen of which is wide. This is necessary in order to avoid the formation of foam in the medicine. The dosage, administration regimen and frequency of use are determined individually for the child:
- hepatitis A - for preschool children 0.75 ml, at 10 years old 1.5 ml, for children over 3 ml (the second administration is carried out no earlier than 60 days after the previous one);
- measles – from 1.5 to 3 ml (depending on the time that has passed since contact with the infection);
- whooping cough - 3 ml twice with a break a day (no more than 3 days should pass from the moment of contact);
- meningococcal infection - 1.5 ml for infants, 3 ml for kindergarten children (no later than 7 days after contact);
- influenza – once for children under 2 years old 1.5 ml, for children of kindergarten age 3 ml, for schoolchildren up to 6 ml (in case of severe cases, the procedure can be repeated after 1 or 2 days);
- polio – from 3 to 6 ml for children who do not have artificial immunity or are not fully vaccinated;
- with reduced resistance, in order to increase immunity, the dose is calculated by weight 0.15 ml per kilogram, up to 4 injections with a break of 48-72 hours.
If blood levels indicate a decrease in immunoglobulins, the child is administered the drug in a volume equal to his body weight (1 ml per kilogram). Repeated use of the medication is permissible no earlier than after 30 days.
Intravenous injection
Before intravenous infusion, the medication is diluted with 0.9% saline or 5% glucose is used as an alternative. The proportion of the medicinal substance in relation to the diluent is selected 1:4.
The dose for children is calculated according to body weight. For every kilogram there should be 3-4 ml of stimulant. It is important that the total volume of the injection does not exceed 25 ml. The intravenous injection is administered slowly while monitoring the child's condition. Often, young children do not allow an injection into a vein. In this case, you should choose another option for using the drug - a dropper.
Infusion via IV
A dropper for children, unlike intravenous administration of immunoglobulin to adults, is also preferably pre-diluted in a solvent. To do this, use sodium chloride or glucose in a ratio of 1:4. This type of medication is administered at a rate of no more than 10 drops per minute. When using an undiluted immunomodulator, the administration rate is up to 40 drops per minute. The dosage of the drug for intravenous use depends on the type of pathological process:
- congenital or secondary immunodeficiency, AIDS – up to 8 ml per 1 kg of weight (once every month);
- after bone marrow transplantation – 10 ml per kilogram (for a week, daily);
- Kawasaki syndrome – 40 ml per kilogram of weight (one time or up to 5 injections per course);
- idiopathic thrombocytopenic purpura – 20 ml per kilogram (one-time use, but the injection can be repeated if prescribed by a doctor);
- sepsis or severe infections – 10 ml per kilogram (for 4 days);
- premature newborns - 10 ml per kilogram with a break of 2 weeks;
- inflammatory demyelinating neuropathy – 8 ml per kilogram (5 days, repeat no earlier than after 4 weeks).