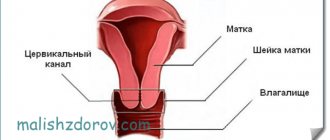
The cervix is one of the most important areas in the female reproductive organs. It refers to the uterus, that is, the internal genital organs, but at the same time serves as a boundary separating the internal and external genital organs.
Its distal section communicates with the vaginal cavity, and its proximal section with the uterus. Performs many functions, the main one of which is protective or barrier, as it prevents the penetration of pathogenic pathogens into the uterus and, accordingly, the abdominal cavity.
Purpose of the procedure
A cervical biopsy is performed in the following cases:
| Name | Description |
| Erosion | The pathology is characterized by a bleeding ulcer that forms on a thinned area of the mucous membrane. Erosion is not life-threatening for a woman, but may be a sign of a malignant process or viral infection. |
| New growth or compaction | The purpose of diagnosis is to confirm or refute the presence of malignant processes. |
| Human papillomavirus (HPV) | Pathogens can remain in a woman’s body for a long time without visible signs. They are activated under the influence of certain provoking factors, against the background of which immunity decreases. A biopsy will help determine the disease and select treatment. |
The study of affected tissues also helps to determine the cause of changes in cellular structures, exophytic condylomas, and malignant processes.
Indications for cervical biopsy
The indication for a cervical biopsy procedure is the detection in the patient of:
- changes of unspecified etiology (pathological changes in the cervical mucosa identified during colposcopy);
- dysplasia (precancerous pathology, in which atypical cells with a tendency to malignancy are found in the normal epithelium);
- ectopia (cervical erosion, endocervicosis) - pathological damage to the mucous membranes of the cervix with the appearance of bleeding erosions with a heterogeneous surface (biopsy of the cervix for erosion is the most reliable sensitive diagnostic method);
- leukoplakia (pathological thickening, proliferation and keratinization of the squamous epithelial layer);
- polyps (local benign neoplasms that rarely have the potential for malignant degeneration);
- genital warts (genital warts) – cone-shaped growths on the mucous membrane that are viral in nature and transmitted through sexual contact;
- iodine-negative areas (identification of areas of the mucous membrane that are not stained with iodine solutions may indicate the presence of atrophic changes in the mucous membranes, dysplasia, leukoplakia, etc.);
- acetowhite epithelium (areas of the mucous membrane that have turned white after treatment with solutions of acetic acids) - the presence of such epithelium may indicate the development of leukoplakia, the presence of human papillomavirus infections (HPV), etc.;
- atypical vascular growths, abnormally tortuous capillaries, etc.;
- gross damage to epithelial tissues.
Also, a histological biopsy of the cervix is indicated if koilocytes (appear during HPV infection), atypical cells in the squamous epithelium (ASC-US, ASC-H), atypical cells in the cylindrical (AGC) and squamous epithelium (HSIL) are detected in the Pap smear. as well as precancerous changes in the mucosa.
If indicated, immunohistochemical screening for cervical cancer using tumor markers may be required. This study is carried out for the purpose of early diagnosis of cervical dysplasia, which has a high risk of malignancy.
Immunohistochemical screenings are indicated when identifying:
- cervical intraepithelial neoplasia grade 2-3;
- HPV (human papillomavirus) with high degrees of oncogenic risks;
- Any neoplastic processes in the mucous membranes of the cervix (the study is carried out to clarify the diagnosis, make a prognosis, assess the sensitivity of the tumor to chemotherapy, hormones, radiation therapy, etc.).
You may also need a procedure called cervical conization (a surgical diagnostic and therapeutic method in which the outer part of the cervix containing atypical epithelium is removed, while the removed part of the cervix has a conical shape, which determines the name of the procedure)
Conization surgery of the cervix is indicated if the patient has:
- ectropion (eversion of the cervix);
- the presence of atypical cells in the Pap smear;
- erosive lesions of the cervix;
- cervical dysplasia of the 2nd and 3rd degree;
- cervical intraepithelial neoplasia;
- neoplasia and erosions affecting both the vagina and cervix;
- cystic neoplasms in the cervix;
- postpartum cervical deformities;
- precancerous conditions in the cervical mucosa;
- suspicion of cervical cancer.
In what cases is a biopsy performed?
The histological diagnostic method is reliably accurate in detecting malignant neoplasms at any stage of development. For research, a specialist takes cells or tissue from an organ.
There are certain indications for a biopsy:
- pathological changes in the mucous membrane of the cervix;
- suspicious lesions of mucous membrane tissue;
- gynecological diseases (endometriosis, leukoplakia);
- formation of polyps;
- precancerous conditions (the surface of the cervix is uneven, covered with tubercles).
Red spots on the surface of the mucosa are also an indication for diagnostic measures. The same applies to dysplasia, when the structure of the cellular structure is disrupted. The pathological condition is considered precancerous.
A biopsy also helps determine the sensitivity of the tumor to the drugs prescribed for therapy. Risks are assessed and repeated recurrences of tumors are identified.
Examination before biopsy
- General blood test (primarily interested in the presence of inflammation and the number of clotting elements - platelets)
- Hemostasiogram (blood clotting test)
- Vaginal smear for flora + gonococci, trichomonas
- Cytological smear (Pap test)
- Colposcopy (examination of the cervix under a microscope)
- Blood test for STIs (chlamydia, mycoplasma) using PCR method
- Blood test for HIV and hepatitis B and C using ELISA
- RMP (microprecipitation reaction to syphilis)
Types and methods of biopsy
The method of collecting the test material is chosen by the gynecologist, taking into account the condition of the woman, her body and the preliminary diagnosis.
| Name | Description |
| Sighting (colcoscopy) | The sample material is collected using a special needle. The woman is given local anesthesia. First, the doctor examines the surface of the cervix and determines the sampling area. Lubricates the tissue with a special solution and excises a piece. |
| Laser biopsy | A laser knife is used to collect the material to be examined. The patient is given anesthesia. The procedure is less traumatic, but after it the woman experiences red or pink bleeding for 2-3 days. |
| Radio wave biopsy | The risk of complications is minimal. The discharge is weak or completely absent. It is most often prescribed to girls who plan to have children in the future, since radio wave biopsy does not leave scars. |
| Wedge biopsy | During the procedure, the specialist takes the material in the form of a wedge. A scalpel or laser beam is used. The biopsy is performed under general anesthesia. Cervical biopsy. How they do it |
| Loop | During the procedure, the surgeon uses a special loop instrument. A small electric current is passed through it. This histology method is also called electrosurgical biopsy. Scars remain at the site of the tissue taken, which prevents conception. Therefore, loop biopsy is contraindicated for young girls. |
| Circular biopsy | The procedure is painful and therefore requires general anesthesia. Material for research is taken with a radio wave knife or scalpel. |
| Endocervical curettage | During medical procedures, a special curette is used. With its help, mucous secretions are scraped or scraped out from the endocervix. |
| Conchotomnaya | Traumatic method of collecting material. During the procedure, a special device is used - Conchotoma. The instrument looks like forceps, which the doctor uses to grab the uterine tissue and pluck it out. The procedure is performed under local anesthesia in a specialized laboratory. After collecting the material, minor bleeding is acceptable. |
Any method is as informative as possible and is chosen by a gynecologist.
What is a cervical biopsy?
A cervical biopsy is a gynecological examination that allows you to clarify the diagnosis if cervical dysplasia or cancer is suspected.
Why is a cervical biopsy performed?
This analysis is necessary if suspicious changes were detected in the cervix. A biopsy helps the doctor understand whether the cells in the cervix are benign (normal) or malignant (cancerous). Depending on the results of the biopsy, the gynecologist will formulate further treatment tactics.
Who needs a cervical biopsy?
Your gynecologist may recommend a biopsy if any unwanted changes in the cervix are suspected. The most common indications for cervical biopsy are:
- poor smear cytology results
- the presence of suspicious changes in the cervix during colposcopy (acetowhite epithelium, iodine-negative areas, atypical vessels, the presence of rough mosaics and punctuation, etc.)
- cervical erosion
- leukoplakia (hyperkeratosis)
- cervical polyps
- condylomas
On what day of the cycle can a cervical biopsy be done?
The most favorable days of the menstrual cycle for performing a cervical biopsy are days 7-13 (the first day of the cycle is considered the first day of menstruation). It is better to do a biopsy immediately after the end of your period, so that the wound on the cervix has time to heal by the beginning of the next menstruation.
How to prepare for a cervical biopsy?
To reduce the risk of biopsy complications, use the following recommendations from gynecologists:
- avoid sex 2 days before cervical biopsy
- do not use tampons or douche 2 days before the biopsy
- do not insert any medications into the vagina (only medications recommended by your gynecologist are allowed)
The evening before visiting the gynecologist, take a shower, following the rules of intimate hygiene. If the biopsy will be done under general anesthesia, try not to eat anything for at least 8 hours before the procedure.
What tests should be done before a cervical biopsy?
A cervical biopsy is an invasive procedure that carries the risk of infectious complications. In order to prevent undesirable consequences of a biopsy, a thorough examination is prescribed before this procedure.
As a rule, the gynecologist recommends taking the following tests before the biopsy:
- complete blood count and coagulogram (test for blood clotting)
- smear for flora (including gonorrhea and trichomoniasis)
- smear for cytology
- colposcopy
- tests for hidden infections (chlamydia, mycoplasmosis, ureaplasmosis)
- tests for HIV infection, viral hepatitis, syphilis
Contraindications to cervical biopsy
If during the examination you are found to have inflammatory diseases of the vagina or cervix, the biopsy will have to be postponed until the inflammation goes away.
Your gynecologist may order additional tests to determine the cause of the inflammation, or may prescribe treatment right away if the cause of the inflammation is clear.
A cervical biopsy should not be done during menstruation.
If you suspect you are pregnant, be sure to tell your doctor.
Is it possible to have a cervical biopsy during pregnancy?
In some cases, a cervical biopsy may be required during pregnancy. If your gynecologist notices suspicious changes in the cervix and concludes that waiting until after birth may be dangerous, a biopsy may be done during pregnancy.
A cervical biopsy in the early stages of pregnancy (up to 12 weeks) may slightly increase the risk of miscarriage, and in late pregnancy it can provoke premature birth, so gynecologists recommend performing a biopsy in the second trimester of pregnancy, when the risk of complications is lowest.
If the gynecologist considers that the detected changes in the cervix do not require immediate diagnosis, then the cervical biopsy can be postponed and done 6 weeks after birth.
What types of cervical biopsy are there?
There are several different methods for performing a cervical biopsy, so be sure to ask your gynecologist which method is right for you.
The choice of biopsy method depends on the preliminary diagnosis and several other factors known to your gynecologist. Some types of biopsy are not only a diagnostic method, but also a method of treating cervical pathologies.
Colposcopic (targeted, puncture) biopsy of the cervix
This is the most common method of cervical biopsy, which is considered the “gold standard” in the diagnosis of cervical dysplasia and cancer.
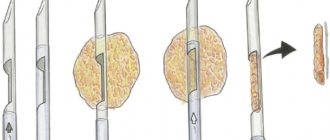
A targeted biopsy of the cervix is carried out during colposcopy, and those areas of the cervix that seem suspicious to the doctor are taken for analysis. To collect the material, a special needle is used, which takes a “column” of cervical tissue containing all the cell layers necessary for the study.
A needle biopsy does not require hospitalization and can be performed in a gynecologist's office. This type of biopsy does not require general anesthesia and is usually performed without any pain relief. During the biopsy, you may experience discomfort, pressure, or tingling that lasts no more than 5-10 seconds.
After a colposcopic biopsy, bleeding from the vagina may appear, which lasts no more than 2-3 days.
Conchotomic cervical biopsy
Conchotomic biopsy is not much different from the targeted biopsy described above. The only difference is that for a conchotome biopsy, not a needle is used, but a special conchotome instrument, which looks like scissors with pointed ends.
Conchotomic biopsy does not require hospitalization. In order to reduce pain, you will be given local anesthesia shortly before the material is collected.
Spotting may occur for several days after the conchotomy biopsy.
Radio wave biopsy of the cervix (biopsy with the Surgitron apparatus)
Radio wave biopsy does not cause significant damage to cervical tissue and is associated with a low risk of complications.
This method of biopsy of the cervix is performed with a special instrument sometimes called a radioknife. In Russia and the CIS countries, the Surgitron device is used to perform radio wave biopsy.
Biopsy with Surgitron does not require general anesthesia and can be performed in a gynecologist's office. After a radio wave biopsy, there is virtually no bleeding, or it is not profuse and lasts no more than 2-3 days.
The risk of scarring on the cervix after a radio wave biopsy is extremely small, and therefore this type of biopsy is recommended for girls and women who are planning a pregnancy in the future.
Laser biopsy of the cervix
In a laser biopsy, areas of cervical tissue are removed using a laser knife (laser).
Laser biopsy is performed in a hospital setting because the procedure requires a short general anesthesia.
This biopsy method is considered low-traumatic and rarely causes any complications. For several days after the biopsy, you may experience some spotting (red, brown, pink) discharge.
Loop biopsy of the cervix
Loop biopsy is also called electrosurgical biopsy or electroexcision. Some countries use English abbreviations for this type of biopsy: LEEP or LETZ.
The essence of a loop biopsy is that suspicious areas of the cervix are peeled off with an instrument similar to a loop through which an electric current is passed.
Electroexcitation can be performed in a gynecologist's office. This procedure does not require general anesthesia, but local anesthesia is required.
For several weeks after electroexcision, bleeding of varying degrees of abundance may be observed.
It is believed that electrosurgical loop biopsy of the cervix may cause scar formation on the cervix. Such scars in the future may become an obstacle to conceiving a child or to carrying a pregnancy to term. In this regard, electroexcision is not recommended for young girls and women who are planning a pregnancy in the future.
Wedge biopsy of the cervix (cervical conization, knife biopsy, cold knife biopsy)
During a wedge biopsy, the gynecologist removes a triangular piece of the cervix in such a way as to obtain the most informative areas of the cervix for further examination. This type of biopsy is sometimes called an extended biopsy because, unlike a targeted biopsy, not only suspicious areas of tissue are removed for examination, but also nearby tissue that appears healthy. Conization of the cervix can be used not only as a diagnostic method, but also as a method of treatment for certain pathologies of the cervix.
To perform a wedge biopsy, a regular surgical scalpel (knife) is used, which is not heated by either current or radio waves, so this method is sometimes called a knife or cold-knife biopsy.
A wedge biopsy requires anesthesia (general anesthesia, spinal or epidural) and the procedure is performed in a hospital. After cervical conization, you may be discharged the same day or the next day.
For several weeks after the biopsy, you may experience pain in the cervical area, as well as spotting of varying degrees.
Circular biopsy of the cervix
Circular biopsy is one of the types of conization of the cervix, which can be performed using a scalpel or using a radio wave knife. During a circular biopsy, a large area of the cervix is removed, including part of the cervical canal. This biopsy method is used both as a diagnosis and as a treatment for certain pathological conditions of the cervix. A circular biopsy also refers to an extended biopsy, since not only suspicious areas of tissue are taken for examination, but also neighboring tissues that may appear healthy.
A circular biopsy is performed under general anesthesia, spinal or epidural anesthesia in a hospital setting (in a hospital). You may have pain and bloody vaginal discharge for several weeks after the biopsy.
Endocervical curettage
Endocervical curettage differs significantly from the cervical biopsy methods listed above, but just like a biopsy, this analysis helps to identify malignant processes in the cervix.
Endocervical curettage is curettage of the cervical canal (not to be confused with uterine curettage), thanks to which it is possible to obtain cells from the cervical canal for research.
Local anesthesia is used to perform endocervical curettage.
How is a cervical biopsy done?
There are several different methods for performing a cervical biopsy, and depending on the method chosen, the doctor's actions may vary.
Ask your gynecologist how this procedure will work in your case.
If the biopsy is performed by a gynecologist in his office, this means that you will not be given general anesthesia, that is, you will remain conscious. To perform the biopsy, you will need to sit in the gynecologist's chair, as you would during a regular examination. In order to see the cervix, the doctor will insert a speculum into the vagina. A bright light will then be shined on your cervix to help you see it better. If necessary, the doctor will inject an anesthetic in the cervical area - this will help reduce pain during the biopsy. Suspicious areas of the cervix will then be removed and sent for histological examination under a microscope. The whole procedure will take no more than 25-30 minutes. You will be able to go home immediately after the biopsy.
If the biopsy is done in a hospital, you will most likely need to be hospitalized for 1-2 days. In this case, you need to ask what type of anesthesia you will receive: general anesthesia, spinal or epidural anesthesia. If you have general anesthesia, you will be asleep during the procedure; If you have a spinal or epidural anesthesia, you will remain conscious but will not feel the lower half of your body. The entire procedure, including anesthesia, can take from 40 minutes to 1.5 hours. After the biopsy, you will need to stay in the hospital for a few more hours, or until the next morning.
Cervical biopsy: does it hurt?
A cervical biopsy may seem painful, so in most cases, before taking material for examination, the gynecologist injects a painkiller into the cervix.
Some biopsy techniques can be so painful that they require general anesthesia, spinal or epidural anesthesia.
In any case, your doctor will do everything to make the procedure painless and comfortable for you.
What happens after a cervical biopsy?
Almost all women experience bleeding from the vagina after a biopsy. Depending on which biopsy method was used, the discharge may be more or less abundant and prolonged:
- after targeted, conchotomous, radio wave or laser biopsy: light discharge, lasting 2-3 days;
- after loop biopsy (electroexcision), conization of the cervix: discharge may be quite heavy (like bleeding during menstruation) for the first 5-7 days, and then spotting for several weeks.
If you experience spotting, use a pad. You should not use tampons, douche, or have sex until the discharge stops completely.
You may also experience pain in the lower abdomen or deep inside the vagina after the biopsy. This is normal and the pain will go away soon.
Some women may have a fever after a cervical biopsy. An increase in temperature may be associated with stress, but may also indicate infectious complications. Contact your gynecologist if your body temperature is above 37.5C.
Is it possible to have sex after a cervical biopsy?
After a cervical biopsy, it is recommended to abstain from sex for at least 7 days.
In some cases, your gynecologist may recommend sexual rest for 2-3 weeks after the biopsy.
Complications of cervical biopsy
In rare cases, complications such as bleeding and infection may occur after a biopsy. See your doctor as soon as possible if:
- you have heavy bleeding that is bright red or dark in color with blood clots
- “period” after biopsy lasts more than 7 days in a row
- bleeding is not profuse, but lasts more than 2-3 weeks
- your body temperature has risen (37.5C or higher)
- you have vaginal discharge with an unpleasant odor
Consequences of cervical biopsy
Puncture, conchotomic, laser and radio wave biopsies, as a rule, do not leave any consequences.
After electroexcision (loop biopsy), as well as after conical biopsy (wedge-shaped and circular), scars (scars) may remain on the cervix. Some women with cervical scars may have difficulty conceiving or maintaining a pregnancy.
If you have had a cervical biopsy and are planning a pregnancy in the future, be sure to tell your gynecologist.
How to interpret the results of a cervical biopsy?
Only a specialist can adequately decipher the results of a cervical biopsy: a gynecologist or oncologist. Do not rush to interpret the results yourself, as some terms may unduly frighten you.
In this article, we'll look at the meaning of key terms you may see in your cervical biopsy results.
What are koilocytes?
Koilocytes are modified cervical cells that appear if a woman is infected with the human papillomavirus (HPV). Normally, there should be no koilocytes, and their presence indicates an increased risk of developing dysplasia and cervical cancer. It is important to understand that the presence of koilocytes is not precancer or cancer. However, you need to pay special attention to your health and listen to your doctor's recommendations.
What is acanthosis, parakeratosis, hyperkeratosis, leukoplakia?
Acanthosis, parakeratosis, hyperkeatosis, leukoplakia - all these processes in the cervix represent the replacement of normal cervical epithelium with keratinizing epithelium (like keratinizing epithelium of the skin).
These conditions are not yet precancer or cervical cancer, and yet, your gynecologist will advise removing these altered areas of the cervix.
What is cervical dysplasia?
Cervical dysplasia is a precancerous condition that, without treatment, can develop into cervical cancer. Cervical dysplasia can be successfully treated. On our website there is a separate article dedicated to Cervical Dysplasia.
What to do if the results of a cervical biopsy are bad?
First of all, don't worry. In most cases, unwanted changes in the cervix can be successfully treated. Even cervical cancer can be cured if detected early.
Contact your gynecologist and, if necessary, consult an oncologist. Listen to the recommendations of your treating doctors and do not self-medicate.
Classification of types of biopsies according to sampling method
A gynecologist will not only select the most informative and safe biopsy method, but will also tell you when it is best to collect the material. To obtain accurate results, you must prepare properly and remember the specialist’s recommendations.
Based on the sampling method, the following types of biopsy are distinguished:
- wedge-shaped;
- circular;
- sighting;
- laser;
- loop;
- radio wave.
A biopsy of the cervix is done to determine erosion, changes in the tissues of the female organ, the formation of polyps, and hyperkeratosis. Additional diagnostics are carried out if the cytology smear shows poor results. The analysis also allows us to identify malignant processes and various diseases that provoked them.
Contraindications for biopsy
In order to exclude the development of possible complications after the procedure, it is necessary to exclude possible conditions that could aggravate the process.
Among them are:
- The presence of inflammatory processes on the cervix or vagina, carriage of specific sexually transmitted infections.
- Discharges that are pathological in nature.
- Pathology of the hemostatic system. This may be a blood clotting disorder, the presence of thrombophilia or changes in hemostasis.
- Lack of technical equipment , insufficient qualifications of a specialist, as well as insufficient compliance with the rules of asepsis and antiseptics.
- State of pregnancy. This is especially true in the first and last trimesters of pregnancy. In the second trimester of pregnancy, the contraindication is relative; a biopsy is allowed if the possible benefit of obtaining the result outweighs the risk. This is important if a malignant process with rapid progression of pathology is suspected.
Preparation for the procedure
A cervical biopsy is performed using an invasive method. There is a high probability of not only complications, but also infection.
Before the analysis, in order to minimize negative consequences, the gynecologist prescribes a multi-stage diagnosis to the woman:
| Name | Description |
| Coagulogram | Blood clotting is determined. |
| Flora analysis | The results will confirm or refute the development of pathological processes, infectious agents and help assess the state of the microflora. |
| General blood and urine analysis | The results will show the development of the inflammatory process. |
| PAP test | Cytological studies to determine the precancerous or cancerous condition of the cervix. |
For certain indications, a woman is also prescribed an additional biochemical blood test. Tests are carried out for HIV infection, syphilis and hepatitis. Taking into account the results of the examination, the gynecologist allows or prohibits diagnostics.
To obtain accurate information and prevent serious complications, it is also necessary to properly prepare for the procedure:
- refuse sexual intercourse several days before diagnosis;
- before collecting material, do not use tampons or douche for 2 days;
- Do not use vaginal suppositories;
- Immediately before going to a specialist, it is recommended to take a warm shower, observing all the rules of intimate hygiene.
If general anesthesia is planned for the procedure, the woman should not eat for 8-10 hours before the biopsy.
Methods and techniques for tissue collection
Depending on the technique for obtaining tissue for histological examination, there are:
- Radio wave biopsy;
- Conchotomous;
- Targeting (puncture);
- Loop;
- Laser;
- Wedge resection.
Radio wave biopsy
The trend in surgery in recent years is the search for the least traumatic and minimally invasive methods of diagnosis and treatment, which are not accompanied by complications, but are highly informative. One of them is the radio wave method. It has a number of advantages and is preferable for women of all ages with any pathology of the uterine cervix.
radio wave biopsy using the Surgitron device
Radio wave biopsy is based on the action of high temperature on cells, the liquid part of which evaporates . The main instrument in this case is a loop through which high-frequency radio waves pass. The loop does not touch the excised tissue, that is, the method is non-contact. Evaporation of tissue is accompanied by the formation of steam, which coagulates blood vessels, preventing bleeding.
Radio wave biopsy is practically painless, allows you to preserve the integrity of both the removed tissue fragment and the surrounding tissues, therefore it is highly informative and low-traumatic. The risk of burns, scarring and infectious-inflammatory complications is extremely low, as is infection due to the disinfecting effect of radio waves. Healing proceeds much faster than after conventional surgical procedures.
The radio wave technique is preferable for nulliparous women who are subsequently planning a pregnancy, since it does not leave scar deformation, and, therefore, there is no risk of miscarriage or miscarriage.
Radio wave biopsy can be performed on an outpatient basis and without anesthesia, without specific preparation, it is simple to perform and accessible to a wide range of patients. To carry it out, the Surgitron device is used, which is available in many antenatal clinics and gynecological hospitals.
Thanks to the listed advantages of the method, radio wave biopsy is practically free of contraindications. It cannot be performed on patients with a pacemaker, and this is perhaps the only reason to abandon this diagnostic method in favor of standard surgery.
Puncture (targeted) biopsy
Targeted biopsy remains one of the most common methods of obtaining cervical tissue for morphological analysis. It is carried out under the control of colposcopy, and the doctor excises those fragments of tissue that seem most suspicious upon examination. The material in the form of a column is taken using a puncture needle.
A puncture biopsy is performed in antenatal clinics and does not require special preparation or anesthesia. Subjective unpleasant sensations are short-lived and limited to those seconds when the needle enters the thickness of the organ.
Conchotomic technique
A conchotome biopsy is performed with a special instrument (conchotome) resembling scissors. It also does not require hospitalization, but can be painful and is most often accompanied by local anesthesia.
Loop and laser biopsy
loop biopsy
Loop biopsy involves excision of tissue using an electric current passing through a special loop. Electrical excision is painful and therefore requires local anesthesia, but there is no need for hospitalization.
Excision of tissue with electric current is quite traumatic; the defect is scarred and epithelialized over several weeks, and the woman may complain of bloody discharge from the genital tract.
After the action of the electric loop, there is a risk of the formation of dense scars that deform the cervix, which will interfere with pregnancy in the future, therefore this biopsy method is extremely undesirable for nulliparous patients planning to have children.
Laser biopsy is based on the use of a laser beam as a cutting tool. This manipulation is accompanied by pain, so it is done under general anesthesia. Advantages: rapid healing and low likelihood of scar deformities.
Wedge biopsy (conization)
wedge biopsy
During wedge resection, the doctor takes material in the shape of a cone, which includes both the surface epithelium and the underlying layer. This type of biopsy is considered extended, since both pathologically changed and surrounding tissues are taken into the removed organ fragment, which makes it possible to examine the transition area and use this type of biopsy as a therapeutic measure.
Conization of the cervix is traumatic, because it is carried out with an ordinary scalpel without the use of electric current or radio waves. This procedure is painful and requires anesthesia ranging from local anesthesia to general or spinal anesthesia.
Circular biopsy
One of the options for surgical excision of a fragment of the cervix for histological analysis is a circular biopsy, in which a large section of the cervix is removed with a scalpel or radio knife along with the initial part of the cervical canal.
A circular biopsy is traumatic and is performed in an operating room, always with pain relief. If during this operation the entire pathologically changed area of tissue is removed, then the manipulation is diagnostic and therapeutic in nature.
Endocervical curettage
endocervical curettage
Endocervical curettage is considered a radically different method of cervical biopsy. Its goal is to diagnose the pathology of the cervical canal by scraping its mucosa, carried out under local anesthesia. The resulting tissue is placed in formaldehyde and sent to the laboratory.
The technique of taking a biopsy is not difficult for an experienced specialist. If an outpatient procedure is planned, the woman should come to the clinic at the appointed time with the results of the examinations. The patient is in a gynecological chair; a special mirror is placed in the vagina to improve visibility; colposcopic control is possible.
If the examination may cause pain, then the cervix is pricked with a local anesthetic, and then the affected area is excised using a scalpel, radio knife, conchotome, or electric loop, which is immediately placed in a container with formaldehyde and sent to the pathohistology laboratory.
During a biopsy under general anesthesia, an anesthesiologist talks with the woman before the procedure, and during tissue sampling the patient sleeps and does not feel pain. During spinal anesthesia, the subject does not sleep, but does not feel discomfort from manipulations on the cervix.
Taking material for examination lasts on average about half an hour; in the case of general anesthesia, the operation lasts up to one and a half hours. After an outpatient biopsy, the patient can go home immediately, and during the study under anesthesia, she remains in the clinic for up to 10 days, depending on the condition.
Most women undergoing a cervical biopsy worry about the possible pain of the examination. The sensations will depend on the type of manipulation: during puncture and radio wave biopsy, the woman will not feel pain, in some cases there is no need even for local anesthesia. Biopsy with a scalpel, loop, and laser techniques are quite painful, but painkillers and anesthesia help to survive the pain.
How the research is carried out
A cervical biopsy, taking into account the chosen diagnostic method, is performed in a hospital setting or directly in the gynecologist’s office. The woman is given general anesthesia or local anesthesia.
| Name | Description |
| Outpatient collection of material | The cervical area is irrigated with lidocaine or given an injection. A vaginal dilator is inserted. Tissues are grasped with forceps. The area is treated with a special iodine solution. The doctor plucks off at least 5 mm of the affected tissue. |
| Inpatient diagnostics | In the hospital, a specialist uses general anesthesia to obtain the test material. |
Upon completion of the diagnosis, it is necessary to adhere to certain rules in order to prevent complications and recover in a short time.
Feel
When answering the question whether a biopsy of the cervix is painful or not, you need to take into account that the body’s sensitivity to intervention is different for everyone.
In most cases, the procedure is almost painless. This is due to the fact that there are almost completely no pain receptors in the cervix, and the doctor’s actions themselves will not take more than two minutes. For this reason, women are not usually given anesthesia before undergoing a biopsy.
As for minor discomfort, it will probably be present. This is very similar to pain in the lower abdomen before menstruation. To reduce the severity of discomfort to a minimum, the patient needs to relax, because tense muscles react to the biopsy process with a spasm.
Decoding the results
Considering the method of sampling, the biopsy takes from 30 minutes to 1 hour. The results of the study will be known to the doctor in 10-14 days.
The received data is decrypted into 4 types:
| Name | Description |
| Negative biopsy result | There are no signs of malignant processes. Minor cell changes indicate infection or inflammation. |
| Benign changes |
The woman’s health is not in danger, but it is recommended that she undergo specially selected treatment by a gynecologist. |
| Precancerous condition |
Treatment is necessary to prevent tissue degeneration. |
| Malignant tumors | Cervical cancer |
Oncology is not a death sentence for a woman, especially if the disease is detected at an early stage of development. It is important to go to the hospital in a timely manner and undergo a full medical examination and treatment. Properly selected therapy will allow a woman to maintain reproductive functions.
From anatomy
It would seem that the very phrase “cervix” suggests that the cervix is part of something. Historically, this is the case, there is the body of the uterus and the cervix. But after many years of observations, treatment of a variety of pathologies, and monitoring of pregnant women, the opinion began to emerge that the cervix is still a very special organ with its own structural structure and specific diseases.
The normal length of the cervix is about 3-4 cm, width is about 2.5-3 cm. Its shape is cylindrical, the external pharynx opens into the vagina, and the internal pharynx opens into the uterine cavity.
We pay attention to this aspect, because cervical diseases are now not at all uncommon, even among young and nulliparous women.
And this is all the more alarming because the cervix is a visually accessible organ. And by all standards, the patient should visit the gynecologist once a year. And during this visit she must undergo a smear for flora (to determine whether there is inflammation, vaginal dysbiosis, and so on) and a cytological examination of the cervix (scraping for cancer cells from the cervix), and the doctor also examines the cervix in the speculum.
What diseases can be detected
A cervical biopsy is done if other diagnostic methods have shown the development of pathological processes.
The procedure allows you to identify the following diseases:
| Name | Description |
| Leukoplakia | The disease is characterized by an increased level of horn cells and dyskeratosis. The tissues in the area of the cervical pharynx thicken and grow. |
| Inflammatory process | The content of the cellular composition changes. Inflammation of varying degrees can not only negatively affect the composition of tissues, but also provoke malignant processes. |
| Dysplasia | A pathological precancerous condition that occurs as a result of advanced erosion. Research will help determine the degree of development of pathological processes. |
| Ectopic cervix | The disease is characterized by damage to the mucous membrane and the formation of ulcers. The erosion has a non-uniform surface, crumbles on contact and bleeds. |
| Parakeratosis | Pathology often occurs against the background of leukoplakia. Accompanied by the formation of nuclei in the cells of the cervical mucosa. The cause of the disease is frequent sexually transmitted infections and injuries. |
When polyps appear, histological studies are also required. The disease is characterized by benign growths on the surface of the mucous membrane.
What could be the consequences?
If a woman does not comply with the basic rules aimed at complying with measures to prevent various consequences, measures are taken to protect against undesirable consequences. They can also arise due to errors made during the procedure.
Among them are:
- Inaccurate receipt of material. In this case, it is possible not only not to obtain an appropriate histological response, but also to miss severe pathology.
- One of the most common consequences is prolonged and possibly incomplete tissue epithelization. This can occur due to non-compliance with hygiene measures, the presence of an inflammatory process, heavy physical activity, which can contribute to the divergence of the seams, etc.
- The appearance of bleeding due to disturbances in the hemostasis system.
- The development of severe cicatricial changes that lead to deformation of the organ.
What not to do after the procedure
A biopsy of the cervix is done using traumatic methods. After the procedure, the likelihood of certain complications increases.
A woman is advised to adhere to the following recommendations to avoid negative consequences:
- The gynecologist advises taking a warm shower instead of a hot bath.
- After the procedure, you cannot use tampons for a month. They can be replaced with gaskets.
- Swimming pools, saunas or steam baths are prohibited.
- Physical activity is prohibited.
- During recovery, sexual intercourse should be avoided.
- Treatment of any disorders, changes, or secretions is carried out with tablets or capsules.
By following simple rules, you can quickly return to a healthy, previous life and fully recover.
Types of biopsy
The best outcome of the procedure is the complete removal of suspicious tissue of the cervix (if the lesion occupies a small area of the organ). In other cases, it is necessary to take punctures from different parts of the organ, which means cutting out 2-3 samples during one procedure. Depending on the individual characteristics of the patient’s body, the doctor uses one of the existing types of biopsy:
- Sighting (colposcopic). Using a special colposcope instrument, which is a pair of tweezers, a small piece of tissue is taken. The wound heals completely within 4-5 days after the procedure.
- Loopback (radio wave). A painless method of taking an analysis, which is carried out using a special apparatus. The patient does not require further rehabilitation.
- Knife (cononization). The tissue is taken through a hardware wedge-shaped excision of a tissue fragment. The method is used not only for diagnosis, but also for the treatment of pathological areas (their removal).
- Prevention of osteochondrosis - office exercises for the back, video
- Tattoo care
- Competitions for a fun company
How to speed up cervical healing
After the procedure, the gynecologist prescribes special medications to the woman to speed up tissue regeneration. It is important to use them strictly or read the instructions carefully.
| Name | Indications | Application |
| "Terzhinan" | Treatment and prevention of vaginitis | Vaginal tablets are used before bedtime for 6 days for preventive purposes. |
| "Metronidazole" | Treatment and prevention of infectious lesions | The adult dosage is 1.5 g 3 times. per day for 7 days. |
| "Depanthenol" |
| A woman is prescribed 1 suppository, 2 rubles. per day for 7-10 days. |
Additionally, along with traditional medications, it is important to follow medical recommendations so that damaged tissues heal faster and the woman can return to a full life.
Well-being
The gynecologist will try to carry out the examination as comfortably as possible, so you should expect quite tolerable pain or discomfort. As mentioned above, after a biopsy, bleeding of varying degrees of abundance will appear, depending on the chosen research method. During this period, you can only use pads, not tampons. If you develop a fever, you must contact the doctor who performed the procedure.
Typically, sexual rest is prescribed for 7 days. In rare cases - for two weeks. It is best to wait until the cervix is completely healed and the bleeding and pain have subsided.
Biopsy and pregnancy
During the period of bearing a baby, a woman’s body goes through numerous changes. Hormonal changes provoke the development of many diseases or exacerbation of chronic pathologies. A biopsy helps determine the source of the problem and select the most effective treatment. However, given the period of pregnancy, the procedure is not always permitted.
| Name | Description |
| I trimester | In the early stages of pregnancy, a cervical biopsy is completely contraindicated, since there is a high risk of miscarriage or infection of the fetus. |
| II trimester | During this period, it is not recommended to carry out the procedure, because it can provoke early labor. In the future, when a child is born, the uterine tissue may also be injured. There is an increased risk of severe bleeding or inadequate tissue repair. |
In the second trimester, a biopsy is sometimes performed, but if there are no contraindications. Doctors take this risk if there is a suspicion that a woman is developing cervical cancer.
Contraindications
If the gynecologist discovers any inflammatory processes in the vagina, the biopsy is postponed until they are eliminated. If the cause of the disease is clear, the gynecologist will immediately suggest a treatment regimen. Otherwise, additional tests will be needed to understand what is causing the inflammation. The procedure is not carried out during menstruation.
Sometimes during pregnancy, the doctor may suggest this test, taking into account the risks and benefits. It is most dangerous to perform a biopsy before 12 weeks, as it can lead to miscarriage. If the procedure is performed in the last weeks of pregnancy, there is a risk of premature birth. The most optimal period is the second trimester of pregnancy.
Possible complications
To speed up the process of tissue regeneration and prevent possible consequences, women are advised to follow simple rules for a month.
Surgery using various methods increases the risk of the following complications:
- body temperature rises;
- there is pain in the lower abdomen;
- troubled by bloody discharge with blood clots or yellow discharge with an unpleasant odor;
- general condition worsens;
- worries about dizziness and poor health;
- Purulent discharge appeared some time after the condition stabilized.
If any complications occur, it is important to promptly consult a gynecologist. The specialist will select a safe and effective treatment. The likelihood of complications increases if a woman smokes, has poor kidney function, or has lung disease.
Procedure for performing the manipulation
How is a cervical biopsy performed?
Depending on the volume of tissue to be removed, it can be performed in a antenatal clinic using local anesthesia or in a hospital under general anesthesia.
The procedure begins as a routine examination by a gynecologist. For pain relief, irrigating the cervix with lidocaine spray or injecting this drug directly into the organ tissue is used. If a circular biopsy of the cervix is performed, spinal, epidural or intravenous anesthesia is required, which is used only in a hospital setting.
A dilator is inserted into the vagina, the cervix is grabbed with forceps and lowered closer to the entrance to the vagina and treated with acetic acid or iodine to detect suspicious areas. If the manipulation is carried out without anesthesia, at this time the patient may feel a slight burning sensation. The doctor removes the abnormal tissue using biopsy forceps, a scalpel, or other instrument.
Is it painful to have a cervical biopsy?
Under conditions of appropriate anesthesia, the woman does not feel any discomfort. There are few pain receptors in the cervix, so manipulations on it may cause discomfort, but do not cause pain. If intravenous, spinal or epidural anesthesia is used, the examination is completely painless.
How is a biopsy performed depending on the method of intervention?
A piece of tissue is taken from the pathological area discovered during colposcopy. If there are several such lesions and they appear heterogeneous, several samples are taken. The doctor uses a scalpel to cut out a wedge-shaped area at the border between the healthy and the changed part of the cervix. It should be large enough, 5mm wide and up to 5mm deep, to encompass the underlying tissue. This is necessary to assess the degree of penetration of altered cells under the epithelium.
Surgitron device for radio wave biopsy, so-called. "radio knife"
When using a special conchotome instrument that resembles forceps, the structure of the tissue may be damaged, which will complicate diagnosis. Diathermic or loop biopsy of the cervix may be accompanied by charring of the edges of the sample, which also reduces quality. Therefore, it is better to use a scalpel. But the best option for the procedure is using radio waves, that is, biopsy of the cervix with Surgitron. This is a surgical device “radio knife”, with the help of which biopsy material is quickly, bloodlessly and accurately taken.
After the procedure, separate catgut sutures are placed on the wound in the cervical area, which will subsequently dissolve. If a knife biopsy was performed, a hemostatic sponge or tampon soaked in fibrin or aminocaproic acid is inserted into the vagina. This is necessary to stop bleeding. With diathermocoagulation or radio wave biopsy, these manipulations are not necessary, since the heat “seals” the damaged vessels and the blood immediately stops.
Taking a biopsy of the cervix should always be accompanied by an examination of the cervical canal to exclude precancerous changes.
The resulting tissue sample is fixed in a formaldehyde solution and sent to the laboratory for examination under a microscope.
Conization, or circular biopsy, is accompanied by the removal of more tissue. A circular excision of the cervix is performed in the form of a cone, with the base directed towards the vagina, and the apex into the cervical canal. It is necessary to capture at least a third of the channel. For this, a special scalpel, Rogovenko tip, radio knife is used, or an ultrasound biopsy of the cervix is performed.
Circular biopsy of the cervix
A circular biopsy is not only a diagnostic, but also a therapeutic procedure. Tissue removal must be carried out so that the biopsy sample includes all the changed cells and part of the healthy neck.
This study is carried out in the following cases:
- damage to the cervical canal, which spreads from the cervix;
- precancer of the canal according to diagnostic curettage;
- suspicion of tumor growth into the underlying tissue during colposcopy, which was not confirmed by conventional biopsy.
Indications for performing the procedure in a hospital:
- conization;
- laser biopsy;
- the need for intravenous anesthesia.
Cost of the procedure
The price of a biopsy depends on numerous factors (method of conduct, use of anesthesia), you can find out from your gynecologist. In most cases, the amount ranges from 1000 to 5000 rubles. In government institutions, the procedure is provided free of charge. The same applies to the oncology clinic.
A cervical biopsy is a traumatic procedure, but the doctor receives the most informative results that help him establish an accurate diagnosis. The procedure is often done under anesthesia to relieve the woman of pain. Recovery is quick if you follow the useful recommendations of your gynecologist.
Article design: Vladimir the Great
How is the procedure performed?
Progress of the procedure:
- The procedure is carried out under strict aseptic conditions while observing safety rules and asepsis with antiseptics.
- The woman is placed on a gynecological chair in a standard gynecological position.
- The external genitalia must be treated with antiseptic agents, as well as the vaginal cavity.
- The gynecologist surgeon performing the procedure must completely clean the hands. The procedure is carried out with strict adherence to the sequence of actions.
- If necessary, pain relief is provided.
- After completion, the cervix is processed and the woman in most cases can go home.
- The resulting biopsy material is placed in a sterile container and signed, after which it is transported to the laboratory.
Recovery period
An excisional biopsy of the cervix is performed on an outpatient basis, after which the patient can go home. The next day she can go to work, or she is given a sick leave for 1-2 days.
After conization, the woman remains under medical supervision for 1-2 days. She is issued sick leave for up to 10 days.
In the first days, you may experience mild pain in the lower abdomen and minor bleeding. Sometimes they have a greenish tint due to the treatment of the cervix with iodine solution. These signs last no more than a week. If pain after a biopsy causes discomfort, you can use regular painkillers. You can put a warm compress on your lower back or wrap yourself in a woolen scarf.
To prevent infectious complications, the doctor may prescribe certain medications, for example, Terzhinan vaginal tablets. They need to be administered at night for 6 days.
Other medications that your doctor may prescribe in the first days after the biopsy:
- antimicrobial drugs Metronidazole or Ornidazole in tablet form;
- rectal suppositories Genferon to stimulate local immunity;
- Betadine vaginal suppositories.
Suppositories may be prescribed to speed up healing and prevent scar formation, for example, Depantol.
Women are advised to wear cotton underwear and use absorbent pads. You need to wash yourself daily with fragrance-free soap and dry the perineal area well. You can drive a car only after 24 hours.
What not to do after a biopsy: lift objects heavier than 3 kg, use vaginal tampons or douches for a week during an excisional biopsy or a month after conization. Sexual intercourse is not allowed for 4 weeks after the usual procedure and 6-8 weeks after conization. According to foreign recommendations, restriction of sexual activity after a puncture biopsy lasts only for a week. For 2-4 weeks you do not need to take a bath, visit the sauna or pool.
Healing of the wound occurs after 4-6 weeks, depending on the amount of tissue removed. After this period, the woman visits a gynecologist who examines the cervix using mirrors.
Menstruation after a biopsy occurs at normal times, since the procedure does not affect the hormonal status and condition of the endometrium. There may be a slight shift in the cycle associated with the patient’s emotional reaction or with the characteristics of the recovery period.