Most diseases are quite difficult to determine based solely on patient complaints. Sometimes even an initial examination cannot help the doctor make an accurate diagnosis. And especially when it comes to chest diseases. This is why there is a need to conduct additional research. The most informative and inexpensive research method is ultrasound diagnostics.
There are many different organs in the chest
What is ultrasound
Ultrasound examination is carried out using a special device. It consists of a main monitor, on which information is displayed, and a sensor. This sensor works using the principle of ultrasonic waves. Penetrating deep through the tissue, the waves reach the organ under study and are reflected from it. This reflection ends up on the main monitor.
To get a better look at the organ, the specialist who is responsible for the diagnosis turns the sensor. In some cases, the specialist may also ask the patient to change position to view the organ from a different angle. It is noteworthy that in most cases, ultrasound is performed in the supine position. However, some types of research are not possible in this situation. And so the doctor may ask the patient to sit on the couch or stand up straight.
When performing an ultrasound, the doctor must examine the organ from different points
It is worth noting the fact that this research method has not always been so popular. Because it was less informative. However, as soon as technology stepped forward, this made it possible to significantly improve the method. Thanks to this, its information content has also increased.
This method is considered one of the most informative and is used to diagnose various diseases.
Purpose of the study
The main symptom of heart disease will be pain. There are many reasons for its occurrence; examination of the heart vessels allows us to determine the etiology of the disease and the prevalence of the pathology.
- Coronarogenic processes are characterized by damage to the vessels responsible for feeding the heart muscle; when sclerotic plaques, stenosis or other pathology of the circulatory system are detected, a diagnosis of IHD (coronary artery disease) is made. The most informative in determining the degree of disruption of the blood supply to an organ will be intravascular ultrasound, used only in case of preparation for surgery.
- In a situation where the patency of the vessels is not impaired, the cause of the disease will be non-coronary mechanisms: myocarditis, cardiomyopathy, impaired conduction of the His bundle, arrhythmias, which is determined by examining the coronary vessels of the heart.
Addressing the cause of the disease rather than the symptom significantly increases the effectiveness of the treatment provided.
When is an ultrasound performed?
Before considering the indications for this diagnostic method, it is worth mentioning that there are two types of chest ultrasound. The first method involves examining exclusively the pleural cavity. It allows you to most accurately determine the volume of the pleural cavity, as well as its contents. The second method allows you to assess the condition of the lungs. Moreover, the specialist also examines the serosa of the lungs.
It is worth noting that it is the second method that experts use most often. It is considered to be combined. And therefore, its use allows you to more accurately assess a larger range of factors.
The indication for ultrasound is a severe cough with sputum.
Let's look at exactly what symptoms might lead a doctor to believe that a patient needs an ultrasound examination of his organs:
- Severe pain and phlegm.
- Difficulty breathing and a heart attack.
- Thrombosis and suspicion of the presence of neoplasms.
- Suspicion of the presence of fluid in the pericardium, as well as the presence of various foreign bodies in the lungs.
Another indication for ultrasound diagnostics is chest trauma. It is a mistake to assume that in this case the doctor will necessarily require an x-ray. After all, most often in case of injuries, an ultrasound examination is prescribed.
What does the decoding of the results show?
During an ultrasound scan, a two- or three-dimensional image of organs is displayed on the monitor screen, the doctor deciphers the ultrasound data, makes the necessary measurements and a written conclusion, which the patient submits to his attending physician. Only a specialist who relies on medical history, laboratory tests and other examinations can correctly interpret ultrasound results and make a diagnosis. It is possible that after an ultrasound examination, other diagnostic methods will be needed to clarify the diagnosis (for example, CT or MRI).
Neoplasms
When examining the lungs, a decrease or increase in the echogenicity of the lung tissue may indicate pathologies such as:
- primary cancer tumors, metastases (foci with smooth edges and vessels inside the formation), damage to the thoracic lymph nodes;
- tumor infiltrates;
- effusion of fluid into the pleura (even slight);
- excess lymph fluid in the lungs.
Suspicion of thoracic neoplasms will need to be confirmed or refuted by using other diagnostic methods - radiography, CT, MRI.
Ultrasound of the mammary glands in women under 40 years of age makes it possible to diagnose mastopathy or malignant neoplasms in the initial stage, when it is possible to completely cure a formidable and common disease - breast cancer. It is advisable for women to undergo this examination 1-2 times a year, as well as an ultrasound of the pelvic organs.
Pneumonia
The inflammatory process in the lungs looks like the presence of hypoechoic areas (foci) in which there is no air or infected fluid is present. There may be several or one such infiltrates; in severe pneumonia, lung abscesses (cavities filled with pus) and pleural effusion can form.
Assessment of the pleural wall parenchyma
Assessment of the condition of the pleura includes checking for the presence of such pathologies:
- the presence of transudate in the pleural cavity - fluid formed due to impaired blood flow or lymph flow (it is not of inflammatory origin and looks like an anechoic (airless) formation);
- during the inflammatory process, ultrasound records exudate in the pleural cavity, interspersed with fibrin threads - signs of inflammation;
- pleural tumors are hypoechoic inclusions of various sizes and types.
Ultrasound assessment of the chest wall reveals:
- hematomas arising from injuries (smooth edges, without vessels, varying echogenicity);
- lipomas are benign tumors (smooth edges, few vessels);
- abscesses - foci of inflammation with clear edges without internal vessels;
- metastases - malignant neoplasms of varying degrees of echogenicity;
- tumor infiltrates - accumulations of malignant cells mixed with lymph or blood, having a hypoechoic structure, uneven boundaries, penetration into other internal organs, their vessels.
Assessment of the parenchyma (the main organ-forming tissue) allows the sonologist to make diagnoses such as lung abscess, pneumonia or infarction - a condition of necrosis of part of the lung that occurs when blood circulation in the respiratory organs is impaired.
What organs are located in the chest
To understand what is included in an ultrasound of the chest organs, you must first consider its structure. The cavity contains several organs. The most “famous” is the lungs. It is worth noting that this organ occupies approximately 4/6 of the total volume of the chest. It is the lungs that perform an important function. After all, thanks to them, a person can breathe. The arteries and veins that are located in the lungs form the pulmonary circulation. It is called the pulmonary circulation.
The chest also contains the heart.
In addition to the lungs, other organs are also located here. These organs include: heart, bronchi, lymph nodes, thyroid gland. Each of these organs is limited to the lungs. The pleura acts as a kind of limiter in this case. That is why sometimes there is a need for a separate study of this limiter.
Ultrasound protocol for respiratory failure
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A | A | A |
| Lateral | A | A | A | A | A | A |
| Rear | A | A | A | A | A | A |
| Conclusion: Echo picture of a normal lung (USDG of non-crystal veins is shown). | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A | A | A |
| Lateral | A | A | A | A | A | A |
| Rear | A | WITH | WITH | A | A | A |
| Conclusion: Echo picture of alveolar consolidation (pneumonia) in c/3 and n/3 of the posterior zone of the right lung (segments 6 and 10 of the lower lobe). | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A | A' | A |
| Lateral | A | A | A | A | A | A |
| Rear | A | A | A | A | A | A |
| Conclusion: Echo picture of partial pneumothorax of the left lung, the point of the lung at the level of the anterior axillary line. | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | A | A | A | A' | ||
| Lateral | A | A | A | |||
| Rear | A | A | A | |||
| Conclusion: Echo picture of complete pneumothorax of the left lung, the point of the lung is not determined. | ||||||
| Profile | On right | Left | ||||
| Zones | at 3 | s/3 | n/3 | at 3 | s/3 | n/3 |
| Front | IN | IN | ||||
| Lateral | ||||||
| Rear | ||||||
| Conclusion: Echo picture of bilateral interstitial pulmonary edema (ECHO-CG shown). | ||||||
Echo pattern of alveolar consolidation
With pneumonia, there is local swelling of the lung, as well as pleural effusion of varying significance.
Due to inflammation and edema, the lung parenchyma becomes echo-dense like the liver - “hepatization”.
Against the background of pneumonia, the sliding of the pleura is usually weak due to a small excursion of the lung and adhesions.
With pleuropneumonia, sliding (-), acoustic enhancement in the form of a bright vertical C-line.
The border between the consolidation and the air tissue is often ragged and echogenic, with an energetic B(+) line behind it.
Within the foci of alveolar consolidation, hyperechoic contours of the bronchi can be observed.
Dynamic bronchogram - movement during inhalation and exhalation - air in the bronchioles during pneumonia.
Static bronchogram - immobility during inhalation and exhalation - atelectasis with bronchial obstruction.
Liquid bronchogram - anechoic tubular structures - fluid inside and along the bronchioles.
Echo pattern of pleural effusion
Usually the effusion is found above the diaphragm, but it can be confined anywhere in the chest cavity.
Pleural effusion is hypo- or anechoic; may include suspension, threads, clots and partitions.
Hemothorax and empyema are isoechoic in the liver and spleen, homogeneous or heterogeneous.
Calculation of pleural fluid volume: V (ml) = maximum separation (mm) of pleural sheets * 20.
B-mode - the hypo- or anechoic area between the sheets of pleura disrupts the shape of inhalation and exhalation.
The echo-dense lung responds to the pressure of the pleural fluid like a sail under a gentle wind.
M-mode - a sinusoid in solidarity with breathing, the sheets of the pleura come closer and diverge during inhalation and exhalation.
Echo picture of pulmonary edema
Pulmonary edema can be focal or diffuse; On ultrasound, many B-lines move along with breathing.
With pulmonary edema in the intercostal space there are more than 3 B-lines; the short pitch between them is less than 3 mm.
To distinguish between cardiogenic and noncardiogenic causes of edema, evaluate left heart function.
Cardiogenic causes of pulmonary edema: impaired LV contraction, abnormal MtCl and AoCl.
The B profile occurs with excessive infusion therapy due to volume overload.
Other causes of pulmonary edema: ARDS, aspiration, pneumonia, allergies, toxins, kidney disease...
Echo pattern of pneumothorax
When the pleural sheets are separated by a layer of air even 1 mm thick, there will be echo signs of pneumothorax.
A'-profile - A-lines, sliding (-); in M-mode, when sliding (-), a “bar code” will be set.
In the presence of sliding of the pleural layers in the M-mode, the “sea shore” picture is determined.
Weakly moving lines of the chest wall (“waves”) lie above a fine-grained layer (“beach”).
The deep granular layer appears from satisfactory respiratory movements of the lung.
In the intercostal space, the sensor is moved back from the sternum to the border of the pneumothorax - the “lung point”.
At the border of pneumothorax, the sheets of pleura stick together during inhalation and are separated by air during exhalation.
Here, at the “lung point,” sliding/non-sliding and “seashore”/“barcode” are interspersed.
“Lung point” occurs with partial pneumothorax; it is absent with complete collapse of the lung.
With a small anterior pneumothorax, the “lung point” is anterior to the anterior axillary line.
With average anterolateral pneumothorax, the “lung point” is above the mid-axillary line.
With massive pneumothorax, the “lung point” is determined posterior to the mid-axillary line.
Echo picture of pulmonary embolism
In a patient with sudden shortness of breath and a normal echo picture of the lungs, it is necessary to exclude PE.
A targeted ultrasound of the deep veins of the non-cancerous veins is indicated: only the femoral and popliteal veins are examined.
The sensor is determined longitudinally immediately under the c/3 inguinal ligament, then to the center of the popliteal fossa.
The vein stuck together due to the pressure of the sensor - there is no thrombus; the vein does not compress completely - there is a thrombus in the lumen.
The thrombus can be “blind” isoechoic; pay attention to the defective color flow signal and spectrum.
Massive pulmonary embolism causes acute cor pulmonale—a “loose” right heart.
A patient with pulmonary embolism sometimes has triangular-shaped foci on the subpleural base.
Rarely does the lesion have a round and polygonal shape; Small pleural effusion often collects.
Echo picture during exacerbation of COPD or asthma
Echo picture of a normal lung, venous thrombosis n/c (-), effusion (-), exacerbation of COPD is likely here.
With anterior emphysematous bullae and at the peak of an asthma attack, the pleural slip is tiny.
The echo pattern is similar to pneumothorax, but the absence of a “lung point” indicates COPD or Asthma.
Echo pattern during intubation
Endotracheal intubation - sliding (+) on 2 sides;
Esophageal intubation - sliding (-) on 2 sides;
Endobronchial intubation - sliding (-) on the 1st side.
Is preparation necessary?
Many studies that are carried out within the walls of a medical institution require special training. However, such a statement cannot be applied to ultrasound examination.
Experts say that if you sign up for a chest ultrasound, the patient does not need to prepare for this procedure in any way.
The only thing that is necessary is to come to the diagnostic room on time, taking with you a small piece of fabric that can be laid on the couch.
There is no need to specially prepare for an ultrasound
Ultrasound of the lungs and pleura
Ultrasound of the lungs and pleura is performed using abdominal scanning settings in the main B-mode.
Sector and microconvex sensors are convenient, but you can work with convex and linear sensors.
For superficial structures - 7-10 MHz, and for general inspection and distant foci - 2.5-5 MHz.
Acoustic shadows behind the ribs, sternum, and spine will significantly interfere with imaging.
Ultrasound is possible through the intercostal spaces, the upper and lower apertures of the chest.
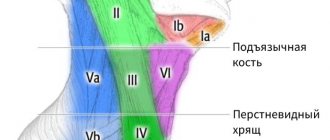
Mark the anterior, lateral, and posterior areas; zones are additionally divided into v/3, s/3, n/3:
- anterior zone - from the sternum to the anterior axillary line;
- lateral zone - from the anterior to posterior axillary line;
- posterior zone - from the posterior axillary to the paravertebral line.
The posterior zone in v/3 corresponds to the upper lobe; c/3 and n/3 correspond to the 6th and 10th segments of the lower lobe of the lung.
The anterior zones are studied with the patient in the supine position, the posterior zones - on the side, stomach, sitting.
When the patient lies on his back, air accumulates in front, and fluid flows back.
Pneumothorax and pulmonary edema are visible from the front, pneumonia and pleurisy are seen from the back and sides.
Every disease with acute respiratory failure has its own special echo picture.
Echo image of a normal lung
A standard cross section shows the shadows of 2 adjacent ribs and the intercostal space.
Below the ribs there is a hyperechoic line of the pleura, and the visceral sheet slides synchronously with breathing.
In the chest cavity there is an obstacle that is insurmountable for the ultrasound beam - the airy lung tissue itself.
Ultrasound does not show normal lung tissue, only an echogenic pleural line with artifacts.
A-lines - horizontal lines occur exactly at a distance equal from the skin to the pleura.
In a normal lung, A-lines are slightly noticeable and bright, single and multiple.
B-lines are vertical lines of the “comet tail” type that run synchronously with the visceral pleura.
B-lines are burned from the echogenic line of the pleura to the end of the depth, crossing across the A-line.
Z-lines are short vertical lines of the “comet tail” type that do not reach the first A-line.
When touching the sheets of pleura, sliding of the visceral pleura, B- and Z-lines becomes visible.
In healthy lungs, in one intercostal space there are several short Z-lines, up to 3 long B-lines.
How is ultrasound performed?
The specialist will tell the patient what position to take and after that the examination will begin. Using the sensor, the specialist will try to examine the area being examined as closely as possible. Typically, the area to be examined is pre-coated with a special ultrasound gel. It increases the throughput of the device.
Next, the doctor will periodically ask the patient to hold his breath. Don't worry if you can't hold your breath for long. Because you will need to hold your breath for just a few seconds. This will allow you to better view the peripheral areas of the lungs.
In some cases, the doctor may ask you to raise your hands for the same purpose.
How indicators should be normal
If no abnormalities are observed, then the doctor can easily evaluate all structures. In other words, subject to the presence of any pathological process, the specialist will not be able to clearly see the following structures on the monitor:
- hypoechoic layer;
- muscles;
- strip of external fascia;
The doctor must check the structure and density of the lung tissue
- layer of loose fiber;
- lung tissue.
Difficulties in examining the above structures may indicate that there are certain pathologies.