Most diseases are quite difficult to determine based solely on patient complaints. Sometimes even an initial examination cannot help the doctor make an accurate diagnosis. And especially when it comes to chest diseases. This is why there is a need to conduct additional research. The most informative and inexpensive research method is ultrasound diagnostics.
There are many different organs in the chest
Ultrasound of the chest - what kind of procedure is it?
Lung ultrasound is not prescribed to all patients; many have not even heard of this type of examination. However, the technique exists and is used for the early detection of various diseases of the lungs, bronchi, pleura, lymph nodes and surrounding tissues. Ultrasound of both lungs is often combined with ultrasound of the pleural cavity. This is due to the need to examine the chest organs in more detail to identify a number of combined pathologies.
The advantages of ultrasound are:
- There is no pain or discomfort.
- There is no need for preparation, refusal to drink or eat.
- There is no effect on medication use.
- In children, the procedure can be performed even in their sleep.
- The duration of the examination is minimal, the price is affordable.
- There are no strict contraindications.
Features of ultrasound in pulmonology
An ultrasound of the bronchi/lungs can be done transthoracically: through the skin and intercostal tissues. Examine the respiratory organs of newborns or infants in the prone position on their stomach and back. Sonography is done for adults or children over one year old while they are sitting or standing.
Ultrasound examination algorithm:
- The subject undresses to the waist.
- The diagnostician lubricates the chest area with water-soluble gel and places the sensor perpendicular to the skin between the ribs or under the collarbones.
- The doctor scans the lung area from all sides of the body, the patient periodically inhales deeply and raises his arms.
- During the procedure, the doctor uses a monitor to assess the condition of the bronchi, lung, and pleura, and takes pictures in places of changes.
After scanning, wipe off the gel from the skin and get dressed. The diagnostician prepares a protocol and hands the document to the patient. When examining a baby, an ultrasound of the lungs, bronchi and pleura takes 5–7 minutes. Sonography for adults takes less than half an hour.
Watch the video of what pneumonia looks like on an ultrasound:
Which is better - X-ray or ultrasound of the chest?
To differentiate oncological pathologies from benign tumors or to clarify a questionable diagnosis, information from ultrasound will not be enough. Ultrasound diagnostics is based on obtaining data from the contact of a sound wave with dense organ tissue. The lungs are filled with air, so their visualization will not be highly accurate. In this regard, such examination is rarely performed in adults, only if there are direct contraindications to radiography.
But in childhood, during pregnancy, ultrasound of the pleural cavity and lungs will be a safe alternative to the use of x-rays.
Despite the fact that with an ultrasound examination of the lungs the information will not be as accurate as with radiography, the technique still has an advantage. Thus, ultrasound has the ability to search for pleural effusion (fluid accumulation) even with its minimum volume (from 5 ml), as well as to identify the type of exudate.
Ultrasound is indispensable if it is necessary to perform a pleural puncture - it is under ultrasound control that this invasive manipulation is performed.
What are they watching?
In order to timely identify diseases of the lungs, pleura and pleural cavity, a type of examination such as ultrasound is prescribed.
Reference! Diseases of the respiratory system are very common, there are many of them - from pneumonia to malignant neoplasms.
The examination is absolutely comfortable and painless; the harm of ultrasound has not been scientifically proven, so there are no restrictions on the number of procedures. Ultrasound of the lungs of the pleura is performed for both preventive and therapeutic purposes.
Fluid in the lungs
The undoubted advantage of this medical technique is the high image resolution. It is this that makes it possible to discern even a small accumulation of fluid in the lungs; this fluid is divided into two types:
- Transudate is a non-viscous, clear liquid. The cause of its occurrence is not inflammatory processes, but impaired blood circulation.
- Exudate is a liquid of inflammatory nature, it is secreted by tissues and cavities of the human body.
Types of exudate
It is customary to divide exudate into several types:
- fibrinous – abundant in fibrinogen;
- serous – clean and transparent, dissolving without a trace;
- putrefactive – dirty green in color with a pungent mothball odor;
- purulent - has a characteristic dull green color. Mating;
- mucous – looks similar to serous, differs in a significant amount of mucin;
- hemorrhagic - the color of which is pink or red; Chylous - due to the significant proportion of fat in the composition, it is externally similar to milk.
Important! In addition to detecting fluid, ultrasound makes it possible to find out about the presence of tumors and determine their nature.
Both when a tumor is detected and when fluid is detected, the next diagnostic step should be a biopsy or puncture under ultrasound guidance.
Ultrasound of the lung, pleura - what it shows
The diagnostic procedure will help in identifying various diseases of the respiratory system and other chest organs. The equipment allows us to discern pathologies of varying severity and stages of development. If the examination reveals lung cancer or other tumor diseases, a CT scan or puncture biopsy is prescribed.
What does ultrasound show in the pleural cavity? This method reflects all additional formations and the amount of effusion in the pleural cavity. The specialist will see what type of liquid fills this zone:
- Transudate. Clean liquid, transparent, thin, there are no signs of inflammation or malignant process. It happens when there is a disruption in the circulatory system.
- Exudate. Inflammatory fluid accompanies various pathological processes. With bacterial phenomena it can be purulent, with viral ones - serous, with tuberculosis - fibrinous. Exudate occurs with blood in cancer or metastases in the lungs, and in a number of infections.
Pathologies
Ultrasound examination helps to diagnose in time:
- unilateral or bilateral pneumonia;
- presence of metastases;
- bronchopneumonia;
- pulmonary infarction;
- peripherally located tumors (more difficult to determine than others);
- the presence of intravascular fluid (occurs in patients with heart failure);
- damage to the lymph nodes by metastases (they are not visible on x-ray);
- primary lung cancer or intrathoracic recurrence;
What is better in terms of identifying certain pathologies - ultrasound or, for example, x-ray?
To identify tumors, X-ray examination is more often used, but to clarify the diagnosis, ultrasound is indispensable. Tumors of the bronchopulmonary system occupy a fairly large proportion among all identified pathologies of various etiologies.
For obvious reasons, ultrasound diagnostic specialists (and others) always pay special attention to neoplasms.
There are several types of neoplasms:
- lipomas (fat);
- fibromas (benign tumors of fibrous connective tissue);
- fibrolipomas (have a mixed composition);
- fibroids (rarely form in the lungs);
- other types of tumors.
Indications for performing ultrasound on the pleural cavity and lungs
Usually, the doctor recommends undergoing a procedure, which is much simpler and safer than an x-ray, for a number of symptoms:
- Wheezing in the lungs.
- Difficulty breathing.
- Low-grade fever with prolonged cough.
- Fever in combination with signs of pulmonary damage.
- Suspicion of peripheral venous thrombosis.
- Signs of accumulation of effusion in the pleura.
- Hemoptysis.
- Suspicion of cancer, tuberculosis.
- Chest pain.
- Prolonged sputum production.
Ultrasound of the pleural cavity is done if it is necessary to perform a diagnostic or therapeutic puncture. An ultrasound is also often performed if inflammation has spread from the bronchi to the lung tissue. In case of pneumonia, an ultrasound examination will show the location of the inflammation and its severity. Lung ultrasound is also used if a foreign body is suspected in the respiratory system, or if there is a chest injury with cough, pain, or wheezing. Ultrasound in the bronchi and lungs will become indispensable if frequent examinations are necessary, for example, to monitor the process and results of treatment.
Advantages and disadvantages
One of the advantages of ultrasound diagnostics is its safety compared to other popular examination methods (X-ray and tomography). The use of ultrasound does not involve exposure to harmful rays, so it can be used as much as needed.
When performing an ultrasound, children are also not subject to any special conditions.
But the procedure also has its disadvantages. Sometimes doctors do not have enough detail in the picture.
The fact is that ultrasound is capable of penetrating into tissues only 7 cm, which does not allow examining the lungs in full.
On the screen of the ultrasound machine you can only see the pleural cavity and the upper parts of the organs.
Due to the high frequency of ultrasonic vibrations, the density of internal organs can be assessed. However, the air in the lungs interferes with ultrafrequencies and impairs visibility. In addition, bone structures, that is, ribs, interfere with the examination of the lungs.
How is the procedure performed?
No preparation is required for this type of examination. You should not refuse to eat food, take medications, or drink water.
The only exception is examination of the respiratory tract under anesthesia (for example, when performing a puncture): such a complex diagnosis will require tests and refusal of food and water for 8 hours.
The procedure for conducting an ultrasound examination is as follows: the patient undresses to the waist and sits on the couch. A special gel is applied to the lung area, eliminating the negative influence of air on the passage of ultrasonic waves. Next, the specialist installs the sensor in the intercostal space, holding it at an angle of 90 degrees. Sometimes 2 different types of probes are used for ultrasound if necessary. In order for the procedure to show reliable results, it is performed in the transverse, oblique, and longitudinal planes.
Ultrasound of a given anatomical zone of the body takes little time - from 10 to 20 minutes. In infants, the duration of the procedure usually does not exceed 5 minutes. An ultrasound to assess the development of fetal lungs in a pregnant woman (performed if a cesarean section is necessary early or if intrauterine fetal pneumonia is suspected) can take about 15 minutes.
The cost of ultrasound varies greatly depending on the type of clinic. A number of medical institutions offer the service at a price no higher than 550-700 rubles, others perform a similar study at a cost of 1500-2000 rubles.
How is ultrasound performed?
The specialist will tell the patient what position to take and after that the examination will begin. Using the sensor, the specialist will try to examine the area being examined as closely as possible. Typically, the area to be examined is pre-coated with a special ultrasound gel. It increases the throughput of the device.
Next, the doctor will periodically ask the patient to hold his breath. Don't worry if you can't hold your breath for long. Because you will need to hold your breath for just a few seconds. This will allow you to better view the peripheral areas of the lungs.
In some cases, the doctor may ask you to raise your hands for the same purpose.
Research results
Normally, during the examination, areas of loose tissue, the border between the lung tissue and soft tissues, the external and internal fascia of the chest, lung tissue, muscles surrounding the chest organs, subcutaneous tissue, etc. should be clearly visualized. Based on changes in echogenicity, the doctor draws conclusions about the presence of a particular pathology. For example:
- Pneumonia - there are foci with air inclusions with unclear contours, sometimes with purulent formations.
- Tuberculosis – enlarged lymph nodes of a dense structure (with a large amount of fluid), oval in shape, located next to the aorta.
- Cancerous tumors are formations with increased blood flow, motionless during breathing. In advanced stages, the picture is complemented by the destruction of ribs and other structures.
- Lung abscess - in an area without air there is a fluid cavity with bubbles inside in the absence of blood flow.
How indicators should be normal
If no abnormalities are observed, then the doctor can easily evaluate all structures. In other words, subject to the presence of any pathological process, the specialist will not be able to clearly see the following structures on the monitor:
- hypoechoic layer;
- muscles;
- strip of external fascia;
The doctor must check the structure and density of the lung tissue
- layer of loose fiber;
- lung tissue.
Difficulties in examining the above structures may indicate that there are certain pathologies.
Diseases for which ultrasound is prescribed
- Hydrothorax
- Pleurisy
- Empyema
- Adhesions in the lungs
- Pneumonia
- Pleural tumors
- Lung cancer
- Metastases to the chest organs
- Lung abscess
- Pulmonary infarction
- Lymph node cancer
- Bronchitis
- Obstructive bronchitis
- Tuberculosis
The data obtained from ultrasound provide a preliminary picture of the disease, which in some pathologies is sufficient to make a diagnosis. In doubtful cases, the patient is referred to CT or radiography. In pediatric practice, ultrasound examination is usually sufficient to determine the cause of the pathology and prescribe treatment.
Lung ultrasound is a diagnostic method that can detect almost all pathological lesions of this organ
Rules for preparing for ultrasound in pulmonology
There are no mandatory preparation requirements for sonography, regardless of whether ultrasound of the pleura, lungs, mediastinum or bronchi is performed. Before the procedure, you can eat, drink non-alcoholic drinks, and take medications.
Respiratory sonography has two limitations. An ultrasound examination is performed on an empty stomach if general anesthesia is used or performed with an endoscopic scanner. For burns, injuries or diseases with deep damage to the epidermis, the procedure is carried out after granulation (healing) of the wounds.
Carrying out
Carrying out an ultrasound of the lungs and bronchi does not require any special preparation. If it is necessary to perform diagnostics in children, it is important to maintain the usual daily routine, coming to the procedure after breakfast or lunch - this will help ensure the child’s calm behavior. To obtain complete and high-quality information, ultrasound of the mediastinal organs is performed using various sensors (convex, vector or linear) with a frequency of 3–7 MHz.
Depending on the access used, sensors with a variable frequency of 2.5–5 MHz or 5.0–10.0 MHz can be used. The examination can be performed in an upright position (standing or sitting) or horizontally (lying on your back, stomach or side). As a rule, during the procedure the doctor asks the patient to accept all of the above provisions.
Scanning of the thoracic area is performed from the following approaches:
What does a lung x-ray show?
- parasternal or intercostal. Scanning is carried out between the third, fourth or fifth intercostal space;
- subcostal. The ultrasound sensor is placed directly under the xiphoid process along the sagittal axis of the body;
- suprasternal. The sensor is installed above the sternum.
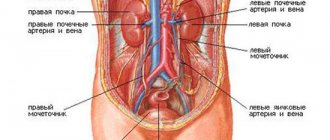
For better visualization of the peripheral parts of the chest, the patient should take a deep breath and hold his breath for a short time. Inspection of the scapular area is carried out after the patient raises his arms up. During the examination, the structure, size, echogenicity and localization of organs are assessed. If there is a diagnosed lung tumor, the list of structures examined includes probable areas of spread of metastases (pleural cavity, lymph nodes, liver, kidneys).
Ultrasound for mediastinal tumors begins with peripheral organs located in the abdominal cavity, supraclavicular region and regional lymph nodes. The research technique for a thoracic tumor is to determine the nature of its relationship with the chest wall by assessing mobility during inhalation and exhalation or when changing body position.
Important! Signs of metastasis of a neoplasm are the immobility of structures adjacent to the tumor, unevenness or blurring of the contour between the tumor and the lung, the presence of arteries, veins or bronchial tubes in the structure of the tumor.
Standard approaches for chest ultrasound
Normal echographic picture
What does an ultrasound of the lungs and mediastinal organs show? Echography allows you to assess the condition of the chest wall, mantle (peripheral) parts of the lungs, dome of the diaphragm, sheets of the pleura, hollow vessels and veins (aorta, branches of the aorta and pulmonary artery), lymph nodes, costophrenic sinuses. With an intercostal scan of the chest wall, all the soft tissues covering the chest (skin, fat, muscles), the ribs and the lung itself are sequentially imaged.
All bone structures, in particular the ribs, are identified on ultrasound as hyperechoic lines, arcuate in shape, with acoustic shadows diverging in the form of a cone. When using high-resolution scanners, the structure of the visceral pleura and the lung can be easily distinguished. The parietal pleura is defined as a hyperechoic line located on the inner side of the chest muscles.
The surface of the lung is located as a wide, well-defined hyperechoic line, located somewhat deeper than the parietal pleura. During scanning, the visible contour of the air lung moves in accordance with the patient's breathing movements. The pleural sinus (the gap between the sheets of pleura) with a small amount of fluid, on the echogram looks like a thin anechoic gap in which the mobile part of the lung is determined.
Scanning from a subcostal approach allows you to see the liver, diaphragm and spleen. When you inhale, the line of the diaphragm, which is about 0.5 cm thick, moves downward, and when you exhale it returns to its previous position. Suprasternal access allows you to assess the condition of the mediastinal organs. In this case, large vessels and lymph nodes are defined as echo-negative structures, clearly protruding against the background of echo-positive fatty tissue.
Normally, lymph nodes should have an oval shape, clear contours and a length on the longest side equal to 1.0 cm. The effectiveness of lung echography depends not so much on the quality of the equipment used, but on the qualifications of the specialist conducting the examination, since significant physiological differences in patients require doctor experience and deep knowledge of anatomy.
Ultrasound image of the pleural cavity from the subcostal approach