Why does a doctor often ask patients to take thyroid hormone tests rather than do an ultrasound? Which hormones should be tested first, and which tests are a waste of money? Dr. Anton Rodionov, in the book “Deciphering tests: how to make a diagnosis on your own,” talks in detail about what each thyroid hormone shows, about the norms of TSH, T3 and T4, and about the treatment of hypothyroidism and thyrotoxicosis.
The thyroid gland is a regulator of metabolic processes that controls many body functions. What the pulse will be, frequent or rare, what the pressure will be, high or low, what the temperature will be - all these questions are answered to some extent by the thyroid gland. Even the degree of intelligence is determined by how the thyroid gland worked in childhood, this is a scientific fact!
Therefore, solving complex diagnostic problems and answering difficult questions from patients: “Why is my skin dry?”, “Why is my heart beating?”, “Why am I constipated?”, “Why don’t boys like me?” ? etc., we invariably ask ourselves a counter question: is there a dysfunction of the thyroid gland?
And in this case, it is not an ultrasound of the thyroid gland that will help us, but a blood test.
| Indicators | Normal (check the results with the normal values of the laboratory that performed the tests, taking into account the units of measurement) |
| Thyroid-stimulating hormone (TSH) | 0.4 - 4.0 mIU/l |
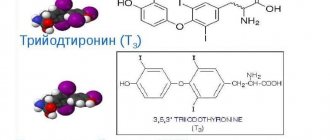
| Triiodothyronine (T3) free | 2.6 - 5.7 pmol/l |
| Thyroxine (T4) free | 9 – 22 pmol/l |
| Antibodies to thyroid peroxidase (Ab to TPO) | <5.6 U/ml |
| Antibodies to thyroglobulin (AT to TG) | 0 - 18 U/ml |
| Antibodies to the TSH receptor | <1.0 U/l |
Treatment of hypothyroidism and thyrotoxicosis
Overt hypothyroidism should always be treated. You will be prescribed thyroid hormone replacement therapy, levothyroxine, which you will need to take for life.
Subclinical hypothyroidism in most cases does not require treatment; tests must be repeated after 3–6 months. The exception is pregnancy, as well as a pronounced increase in cholesterol (> 7 mmol/l). In these cases, even with subclinical hypothyroidism, thyroxine replacement therapy is prescribed.
Manifest (overt) thyrotoxicosis almost always requires treatment. At first I wrote “always,” then, to be fair, I decided to add that there are rare forms that go away on their own. However, thyrotoxicosis always requires consultation with a doctor and observation.
Subclinical thyrotoxicosis does not require treatment, but tests must be repeated after 6 months, there is a possibility of transition to an expanded form.
Thyroid-stimulating hormone
Most endocrinologists rely specifically on the level of thyroid-stimulating hormone in the patient's blood, or TSH. This hormone is produced by the pituitary gland and is designed to stimulate the thyroid gland.
If the level of this hormone in the blood is high, we can conclude that the pituitary gland is working to activate the gland, and accordingly, the body does not have enough thyroid hormones.
Levels of thyroid-stimulating hormone vary from country to country. The range looks like this:
- For Russia, the normal level of TSH in a patient’s blood varies in the range of 0.4-4.0 mIU/l.
- American endocrinologists adopted a new range, according to the results of their research, which corresponds to a more realistic picture - 0.3-3.0 mIU/l.
Previously, the normal TSH range was 0.5-5.0 mIU/L - this was changed to the first 15 years ago, which led to an increase in the diagnosis of thyroid abnormalities.
In our region, it is worth focusing on the first indicator. A TSH above four mIU/L indicates hypothyroidism, and below - hyperthyroidism.
On the other hand, TSH concentration depends on many other factors. For example, low concentrations of thyroid-stimulating hormone are observed in cancer of the pituitary gland, since it is not able to produce hormones. A similar picture is observed after a stroke or injury affecting the hypothalamus.
The time of blood sampling has a great influence on the result of the study. Early in the morning, the level of TSH in the blood is average, by lunchtime it decreases, and by the evening it rises again above the average range.
Antibody tests: is it necessary?
Many saw some other mysterious antibodies in their analysis, for example, antibodies to thyroid peroxidase (AT to TPO) or antibodies to thyroglobulin (AT to TG). An increase in these antibodies indicates that some autoimmune processes may be occurring in the thyroid gland.
I’ll say right away that if this was an analysis “just in case,” then this is money thrown away (your own or the insurance companies’). There is no need to do these tests just in case. They are used not for primary diagnosis, but to clarify the diagnosis in cases where the disease has already been found.
However, the trouble is that often these are also “discarded nerves.” The fact is that antibodies themselves do not require treatment; their isolated increase is not equivalent to the diagnosis of “chronic thyroiditis”. So if a random test reveals an increase in antibodies with normal thyroid function (with normal TSH), then don’t worry. Just get tested for TSH once a year.
Advertising
Who is at risk
Diseases of the thyroid gland, the consequence of which is a decrease in the level of produced hormones or the inability to sufficiently absorb these elements by the tissues of the body, affect primarily the well-being of the patient, without causing him any specific painful sensations. This condition may be genetically determined, or may occur as a reaction to taking certain medications or prolonged exposure to chemicals. Hypothyroidism also often develops with a lack of iodine in food. Lack of absorption or production of thyroid hormones can be caused by other diseases that need to be diagnosed. There is a serious question - what tests should pregnant women with hypothyroidism take, because the intrauterine development of the fetus directly depends on the health of the mother. If a woman is diagnosed with hypothyroidism, hormone tests during pregnancy are standard procedure.
Thyroid diseases: 5 tips
Since we're talking about the thyroid gland, I'll take this opportunity to give a few more important recommendations.
Ultrasound does not provide insight into how the thyroid gland works
- Most regions of Russia are in the zone of iodine deficiency. Buy only iodized salt and use it instead of regular salt.
- Sea kale does not contain as much iodine as is commonly believed. You can use seaweed to make salads if you like, but this does not mean at all that you can abandon traditional methods of iodine prophylaxis (iodized salt or pharmacological doses of iodine for pregnant women).
- You cannot use an alcohol solution of iodine for “prevention and treatment of the thyroid gland,” as is sometimes recommended in TV shows and pseudoscientific books about health. “Iodine nets,” a solution of iodine in sugar or milk, can quickly lead to the accumulation of toxic doses of iodine in the thyroid gland and the development of thyrotoxicosis.
- There is no need to do an ultrasound of the thyroid gland just in case. If the function of the thyroid gland is not impaired, and the gland itself is not enlarged and no formations are palpable in it, then an ultrasound “just in case” will do more harm than good. Detection of small nodular formations, fear of detecting cancer, unjustified repeated punctures, repeated ultrasounds - this is what awaits a person who has set foot on this slippery path of multiple unnecessary examinations.
- A healthy adult needs to have their TSH level determined once every 5 years. If you have previously been diagnosed with subclinical hypothyroidism, subclinical thyrotoxicosis, or if you are taking the antiarrhythmic drug amiodarone, then take a TSH blood test once every 6 months.
What can hypothyroidism be like?
Medicine divides hypothyroidism into two types:
- primary - as a manifestation of disorders in the thyroid gland itself;
- secondary - develops due to malfunctions of the hypozypha.
In order to identify an existing problem in the endocrine system, you need to know what tests are taken for hypothyroidism. They should help identify a decrease in the level of thyroid hormones in the blood so that the patient can undergo further examinations to determine the cause of hypothyroidism.
Classification of autoimmune disease
Autoimmune thyroiditis has several forms, here are the main ones:
- Chronic AIT. Appears due to increased growth of T-lymphocytes. Against the background of this autoimmune pathology, hypothyroidism develops. The most common form of the disease.
- Postpartum thyroiditis. It also occurs very often and appears due to changes in the structure of a woman’s body during pregnancy and hormonal surges. It is enough to simply recover, the function of the gland will stabilize.
- Painless form. The most unpredictable type, it is difficult to understand the course of the disease, it is difficult to notice hormonal disorders at the first stage. To identify it, it is recommended to undergo a periodic comprehensive examination.
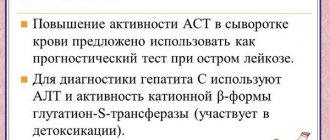
- Cytokine-induced thyroiditis. Occurs due to taking pharmacological drugs for liver damage and blood disorders. The treatment process is long and complex.
Modern diagnostic methods make it possible to accurately determine the form of the disease, hormone levels and the condition of the thyroid gland. After this, the doctor prescribes treatment depending on the form. In most cases, AIT can be treated quite successfully. It is impossible to get rid of it completely, but it is easy to prevent further development. The main thing is to contact specialists for help in a timely manner.
Preparing for the examination
Before taking tests if you suspect autoimmune thyroiditis, you need to protect yourself from possible mistakes:
- a month before diagnosis, multivitamins and hormonal medications are excluded; the period can be reduced by the doctor to 15 days;
- if you are constantly taking certain medications, this is indicated when taking tests;
- in 2-3 days, eliminate alcohol, intense physical activity and nervous stress;
- in the evening before the diagnosis, remove fatty foods from the diet; it is better to limit yourself to a light dinner 10-12 hours before the test;
- under normal daily routine, blood is donated from 8 to 10 am;
- You cannot have breakfast, drink tea and coffee, you can drink a glass of still water;
- Smoking is prohibited 30 minutes before the diagnosis;
- 15-20 minutes before blood sampling, you need to relax in the fresh air, or relax in the hospital premises, adjust your heart pulse and try not to be nervous.
The result will be ready within 1-3 days, depending on the workload of the laboratory to which the patient applied.
Decoding the results
Based on the test results, you can determine what hormones look like normally, and what they look like with autoimmune thyroiditis:
- T4 ( FT4) . Normally, it does not exceed 22.3 pmol/l, while the figure is not lower than 9.56 pmol/l. With AIT, the indicators decrease.
- T3 ( FT3). Normally it is in the range of 2.62-5.77 pmol/l, with AIT the figure decreases.
- TSH . It is measured in mU/l, ranges from 0.47-4.15, and increases with AIT.
- Anti-TPO. Measured in units/ml, the indicator ranges from 0 to 5.57. When sick, it increases sharply.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Weight gain (weight gain, weight gain) | 90% |
| Dryness of the entire skin (dry skin) | 90% |
| Fatigue during physical activity (fatigue, loss of strength) | 75% |
| Daytime sleepiness | 75% |
| Deepening of the voice | 60% |
| Facial swelling | 60% |
| Hair loss on the head | 50% |
| Constipation | 50% |
| Decreased blood pressure (low blood pressure, hypotension) | 50% |
Common T4 and free T4
Total T4 is a measure of all T4 hormones in the blood, including T4 that is bound to protein and is not available for use by body cells. In fact, most of the T4 released by your thyroid gland is bound to proteins.
Important A good endocrinologist will rely on more than just a TSH test as a way to diagnose hypo- or hyperthyroidism. TSH testing, after all, shows only part of the picture; that is, how much the pituitary gland pushes the thyroid gland to produce more hormones. More comprehensive testing will include free T3 and free T4—the actual amount of thyroid hormone available.
Although total T4 testing has been used in the past to diagnose hypothyroidism, it is considered a less useful tool today. This is because the amount of total T4 may depend on the amount of binding proteins in the blood. The amount of protein depends on medical conditions, such as certain types of liver and kidney diseases, and pregnancy. However, low total T4 levels often indicate hypothyroidism.
A more useful diagnostic tool is the free T4 test. This test measures unbound T4 in the blood, called free thyroxine. If it is too little, it is a sign of hypothyroidism. Free T4 enters the body's cells, where it can be converted into T3, the active form of thyroid hormone. In patients who have hypothyroidism, free T4 levels are rarely lower than normal. Patients with hypothyroidism, especially mild hypothyroidism, typically have elevated TSH with low-normal free T4 because TSH rises before free T4. Your doctor should look at the relationship between T4 and TSH to see if there is a discrepancy that could be a clue to a problem.