Blood hemolysis is the destruction of the red blood cell membrane, which leads to the release of hemoglobin. It occurs normally at the end of the cell life cycle, during diseases and poisoning, transfusion of incompatible blood, and also outside the body during testing. Acute hemolysis occurs with the development of shock and renal failure.
Damaged red blood cells make the sample unsuitable for testing. Read more about the clinical and laboratory signs of hemolysis, as well as ways to prevent it, in this article.
Types of red blood cell hemolysis
Destruction of the erythrocyte cell membrane occurs inside and outside the body during laboratory diagnostics. Blood hemolysis always occurs normally and serves to remove non-viable cells, but it can increase with adverse external influences or diseases.
Physiological and pathological
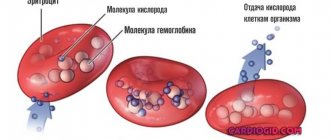
Red blood cells live for about 4 months and are then destroyed by cells in the liver, bone marrow or spleen. As a result, hemoglobin is released, which turns into a pigment - bilirubin. Cell debris is disposed of by macrophages (cleaner cells).
In case of diseases or penetration of poisons with a hemolytic effect, the breakdown of red blood cells occurs faster, which is accompanied by a lack of oxygen delivery to tissues (anemia), an excess of toxic bilirubin (jaundice), the spleen may enlarge, and the functioning of the liver and kidneys is disrupted.
We recommend reading the article on blood rheology. From it you will learn about rheology disorders and measurement methods, hemodynamics, evaluation of indicators, drugs that improve blood rheology. And here is more about antiphospholipid syndrome.
Acute and chronic
Massive destruction of cells is caused by transfusion of incompatible blood according to group or Rh factor, antigenic composition, as well as poisoning. Acute conditions requiring emergency medical care include hemolytic disease of the newborn. It is associated with an immune conflict between the child’s red blood cells and antibodies from the mother’s blood.
These conditions are characterized by fever, chills, pain in the abdomen and lumbar region, vomiting, severe weakness and dizziness. Blood pressure decreases, and in the absence of intensive treatment, acute renal failure develops with a fatal outcome.
Chronic hemolysis occurs in congenital hemolytic anemia. It can be asymptomatic, but can appear after infectious diseases or taking medications that damage red blood cell membranes. Among acquired pathologies, the most common are autoimmune forms, in which the body produces antibodies against its own red blood cells. They occur in a permanent form or are accompanied by hemolytic crises.
Intravascular and intracellular
Normally, there can only be intracellular hemolysis in macrophages that destroy non-viable red blood cells. Congenital enhancement of this process occurs with genetic inferiority of red blood cells. It is characterized by yellowness of the skin, sclera, enlarged spleen, free bilirubin, and decreased haptoglobin (hemoglobin-binding protein).
With the development of hemolytic anemia, the membranes of red blood cells can disintegrate already inside the bloodstream. This leads to an abundant appearance of free hemoglobin. If the liver cannot cope with its processing into bilirubin, then it is excreted in the urine - hemoglobinuria occurs. The spleen in such cases is normal, the disease is accompanied by:
- pain in the kidneys, abdomen, heart due to vascular thrombosis;
- weak yellowness of the skin;
- signs of intoxication - nausea, fever, chills;
- a sharp increase in hemoglobin and low haptoglobin.
Watch the video about the types of blood hemolysis:
Causes
The reasons that trigger the process of destruction of hemolysis can be either external (damage to cells during a blood test or transportation of material) or internal (takes place inside the red blood cell itself).
Internal factors of cell damage include a number of diseases:
- Hemolytic type anemia.
- Hemoglobinuria.
- Aglutinin disease (cold disease).
- Penetration of poisons.
During internal injuries, red cells in the liver, spleen and bone marrow are destroyed. This happens due to the development of congenital microspherocytosis, anemia of the 1st degree and autoimmune nature, a blood disease - thalassemia.
Considering a number of factors that destroy the membranes of red blood cells, it becomes clear that hemolysis poses a danger to the entire body, as it often causes an enlargement of the spleen and liver, leading to the development of very serious diseases.
During pregnancy, the destruction of red blood cell walls is caused by the presence of iron deficiency anemia. In this case, hemolysis during pregnancy is not a severe pathology, but only a physiological process. To normalize a woman’s condition, it is necessary to compensate for the lack of iron in the body. To do this, it is enough to adhere to the basic principles of the diet and eat pomegranates regularly.
Reasons for the appearance of hemolysis in a biochemical blood test
When conducting laboratory diagnostics, the results of the study contain a conclusion that the analysis was not performed due to hemolysis of the blood sample. This situation may arise due to non-compliance with the rules for collecting and storing material. Possible causes of red blood cell destruction:
- traces of the previous portion remained, the dishes were poorly washed;
- the anticoagulant was insufficiently added or incorrectly selected, poorly mixed with the sample;
- during rapid blood sampling, damage to the cell membrane occurred;
- the patient did not adhere to recommendations for limiting fatty foods and alcohol before the analysis, and did not take a break after the last meal;
- the blood was poured into another tube;
- the sterility of consumables is compromised;
- During transport, the sample was subjected to vibration, shaking, heat or light, freezing and thawing.
Hemolysis of red blood cells in diseases
Pathological damage to cells develops in diseases, poisoning, and congenital abnormalities of blood composition. In some sensitive patients, cold and medications can destroy the membrane of red blood cells.
Manifestations of hemolysis are detected in the following conditions:
- transfusion of incompatible blood;
- autoimmune diseases;
- vaccination;
- streptococcal infections (scarlet fever, erysipelas, tonsillitis, endocarditis);
- malaria, toxoplasmosis, typhoid fever, mononucleosis, syphilis;
- systemic candidiasis;
- hepatitis and pneumonia of a viral nature;
- prolonged and uncontrolled use of antibiotics, cytostatics, antiparasitic agents, sulfonamides, painkillers;
- poisoning with lead salts, arsenic, acetic acid, gasoline, mushrooms, ether, chloroform, alcohol (especially surrogates);
- viper, tarantula or bee bite;
- damage to red blood cells when passing through a prosthetic valve or heart-lung machine;
- Rhesus conflict pregnancy;
- acute leukemia, lymphogranulomatosis.
Mechanical destruction of red blood cell membranes also occurs during heavy physical activity, hyperbaric oxygen therapy, severe arterial hypertension, and intravascular coagulation (DIC).
When is hemolysis a normal option?
Natural hemolysis of red blood cells occurs in the spleen
The process of hemolysis itself in the body occurs continuously throughout life, since the life cycle of red blood cells is only 4 months (120 days). Natural intracellular hemolysis, caused by the death of red blood cells, does not cause harm to the body. Instead of destroyed red blood cells, new, more stable and younger ones appear.
Hemolysis is pathological if red blood cells die without living a full life cycle. This can happen under the physical or chemical influence of destructive factors that damage the membrane of red blood cells as their size increases. The cell membrane does not have a stretchy structure, therefore, when the cell enlarges, it ruptures, releasing its component out. When red pigment from red blood cells enters the blood plasma, it takes on an unnatural bright red color.
Signs of hemolysis in the blood
There are clinical and laboratory symptoms of red blood cell destruction . Some forms of diseases can occur hidden and are detected only by analysis. With hemolysis of red blood cells, the following manifestations occur:
- general weakness;
- nausea, vomiting;
- increased body temperature, chills;
- skin and mucous membranes yellowish-pale;
- pain in the lower back, right hypochondrium and epigastric (epigastric) region, headache and heart;
- dark coloration of urine with a red tint;
- disturbance of urination up to cessation in severe cases.
In a blood test, hemolysis is detected based on the following signs:
- decreased red blood cell count;
- increase in young precursor cells (reticulocytes), bilirubin, hemoglobin, lactate dehydrogenase activity;
- The blood plasma turns red and takes on a lacquered appearance.
Symptoms of hemolysis
Acute hemolysis is characterized by rapid onset
Biologically provoked hemolysis occurs unnoticed by the body, since it is a slow-moving natural process.
The chronic form of hemolysis, which usually accompanies the disease that provokes it, also does not have obvious symptoms.
At the stage of acute hemolysis, symptoms can appear sharply and immediately. If the patient is conscious, he may feel:
- feeling of sharp squeezing in the chest;
- unnatural heat throughout the body;
- sharp pain in the chest, abdominal cavity and lumbar region.
Other signs of acute hemolysis:
- decreased blood pressure;
- hyperemic state of blood vessels on the face, and soon subsequent pallor;
- anxiety;
- uncontrolled urination or defecation (indicates a very acute stage).
The state of acute hemolysis initially subsides within a few hours, symptoms subside, discomfort and pain disappear, blood pressure normalizes. Many people mistake this stage for a general improvement in their condition, but after a certain time all the symptoms return with renewed vigor, and with them:
- There is a sharp rise in body temperature;
- Jaundice appears;
- Acute headaches appear;
- Renal dysfunction develops. This requires careful monitoring to avoid the development of more serious pathologies.
Why is this indicator dangerous?
Hemolysis of red blood cells leads to a decrease in oxygen delivery to tissues, causing dizziness, weakness, and low exercise tolerance. But the main danger is associated with the accumulation of hemoglobin in the blood and its increased conversion into bilirubin.
Hyperbilirubinemia negatively affects brain function and increases the load on the liver and kidneys. In severe form, hemolytic crisis is accompanied by a state of shock, liver failure, and cessation of urine excretion.
The destruction of red blood cells outside the body makes laboratory blood tests difficult, requiring repeat tests.
How samples are taken
Blood is usually collected by pricking a finger with a scarifier if capillary blood is needed, or by puncture of the ulnar vein after applying a tourniquet. In order to prevent the occurrence of hemolysis, you should:
- observe all rules of sterility when drawing blood;
- carefully handle laboratory glassware;
- transport samples carefully.
When venous blood enters the syringe, the plunger should not be pulled sharply; it is better to wait for passive filling; it is not recommended to tighten the tourniquet too much.
Since compliance with these rules does not depend on the patient, it is important to choose a laboratory that values its reputation. You should take into account all the doctor’s recommendations regarding the exclusion of fats and alcohol from food, and discuss the possibility of using medications, including conventional painkillers, at least 3 days in advance.
Norm and deviations in analyzes
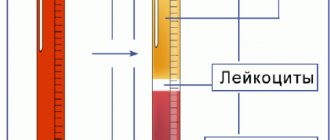
In order to study the stability of red blood cells, a test is used with the addition of sodium chloride solution and a gradual decrease in concentration. It is based on the fact that when they enter a low-salt environment, the membranes stretch due to the entry of water into the cells according to the laws of osmosis. The cells take on the shape of a ball (normally, red blood cells are disc-shaped), but the extensibility of the membrane has a limit. If the salt level is further reduced, hemolysis occurs.
Osmotic stability (resistance) of erythrocytes is most often determined when hemolytic anemia is suspected. Normally, blood hemolysis begins with 0.46 - 0.42% solution and reaches a maximum of 0.3%. For congenital abnormalities of cell structure, it is sufficient to reduce the concentration from 0.9% to 0.7%. Similar processes can also occur in acquired pathologies, most often of autoimmune origin.
Increased osmotic resistance (high resistance to hemolysis) occurs with iron deficiency anemia, thalassemia, and liver diseases. Some hemolytic anemias (secondary passage) occur with normal indicators.
What to do to avoid hemolysis
To prevent destruction of red blood cells in the body, you should:
- Avoid not only eating unfamiliar mushrooms, but even contacting them;
- take precautions when staying in habitats of poisonous insects and snakes;
- When working with toxic chemical compounds, use protective equipment;
- long-term drug therapy is carried out under the control of blood tests.
It is possible to prevent immunoconflict hemolytic diseases in newborns by examining women with negative Rh blood (analysis of amniotic fluid, chorionic villus biopsy). They need the introduction of anti-Rhesus immunoglobulin after an abortion or the birth of an Rh-positive fetus. Termination of a first-time pregnancy is strictly prohibited.
Harmful substances that cause hemolysis
Nature is not only a friend of man, but at the same time a source of danger if you do not know how to behave correctly. For example, hemolysis of red blood cells is sometimes provoked by the following factors:
- eating poisonous mushrooms;
- contact with plant poisons and toxins;
- animal and insect bites;
- penetration of malarial plasmodium into the blood.
The reasons listed above cause hemolysis not instantly, but as the provoking factor acts. In any of these cases, medical consultation and treatment aimed at preventing complications are required.