Every person during his long life is faced with various diseases, which are sometimes not so easy to overcome. If you feel any signs of illness or even serious pain, you should contact the appropriate doctor as quickly as possible, the choice should depend on what your problem is related to. Thus, you will be able to get the necessary diagnostics as quickly as possible, and this will allow you to correctly diagnose and prescribe medications. For a disease called osteomyelitis, x-rays are one of the most common diagnostic examinations. The fact is that it allows you to get fairly informative images with excellent accessibility, that is, this procedure is quite common, and the equipment allows it to be carried out in most medical clinics. Let's take a closer look at how specialists perform x-rays for osteomyelitis of the jaw; we will also not omit other parts of the body that may be affected by this disease.
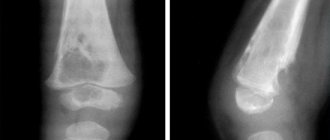
Acute hematogenous osteomyelitis is already visible on x-ray in the initial stages.
When is the examination scheduled?
First, you should consider the main signs that you are developing chronic osteomyelitis or acute osteomyelitis. Let us immediately mention that it can be divided into three categories:
- Infectious. This form is considered the most dangerous, because the disease fully develops in just two days. During this time, the signs of the disease gradually increase, but at first they are usually almost invisible, so in most situations they are simply ignored.
- Toxic. This form of the disease is characterized by the fact that patients’ blood pressure immediately begins to drop, sometimes they feel pain in the heart area and even lose consciousness. As you might guess, you shouldn’t help a person yourself; it’s important to get him to a doctor as quickly as possible.
- Traumatic. This type is always accompanied by severe symptoms, almost immediately the temperature rises and a severe headache begins. If you do not take a person to a doctor, blood poisoning will most likely occur.
Note! Doctors note that sometimes osteomyelitis in the initial stages occurs completely without symptoms, this is very dangerous, because in most such situations there is no treatment or diagnosis, so the disease sometimes immediately passes into a generalized form, and sometimes even into a chronic stage. Carefully monitor your health and the manifestations of your body!
Here are the main general symptoms that appear most often during the local course of the disease (the direction of the x-ray is not particularly important):
- excessive increase in body temperature in the absence of obvious reasons (up to 38.5 degrees);
- the appearance of certain swellings on the body that occur only in the area of the affected area;
- pain or even aches, which is always accompanied by bloating;
- an increase in skin temperature in the affected area, as well as significant redness;
- abscess formation;
- problems associated with certain movements, namely their limitation and the appearance of pain;
- constant discharge of pus occurring directly through the skin.
Sequestra are visible on an x-ray - foci in which necrosis of the bone or muscle structure is observed.
But here are the main signs found in the generalized form of osteomyelitis of the spine, femur, teeth or anything else:
- increase in body temperature to a dangerous state (up to 40 degrees);
- gradual increase in pain, which becomes constant;
- pallor of the skin, and in most situations this is observed throughout the entire skin;
- various neurological lesions, for example, delirium or convulsions, less often loss of consciousness occurs;
- intoxication of the body, expressed in terrible health;
- problems related to kidney function;
- shortness of breath, excessive sweating and chills.
New technologies for restorative treatment of patients with osteomyelitis of the calcaneus
1 Yurkevich V.V., Bashirov R.S., Podgornov V.V., Pekshev A.V., Kolesnikova I.V., Luzgin V.Yu.
The urgency of the problem is due to the increase in the frequency of foot injuries when using explosive ammunition in local wars, complicated by osteomyelitis of the calcaneus, and the unsatisfactory results of traditional surgical treatment in 68.3% of cases with subsequent disability in 72%.
The results of 56 autotransplantations of blood-supplied tissue complexes for chronic osteomyelitis of the calcaneus were analyzed. Good and excellent results were obtained in 53 patients (94.6%).
The proposed microsurgical technologies for the treatment of osteomyelitis of the calcaneus made it possible to move away from the practice of multi-stage traditional operations, reduce the time of hospital treatment and restore combat capability in 44.5% and 37% of the wounded and sick, respectively.
Chronic osteomyelitis of the calcaneus in relation to osteomyelitis of all locations of the skeletal bones is observed in up to 14.8% in peacetime, in wartime – 19.4%, and in relation to the bones of the foot it is 51% [1, 2, 3, 5].
The existing system of traditional treatment of chronic osteomyelitis of the calcaneus requires long-term multi-stage reconstructive plastic surgeries and in 68.3% of cases is accompanied by unsatisfactory results with relapse of the osteomyelitic process and high subsequent disability of people of working (combat-ready) age (up to 72%) [4, 7, 9 ].
The reasons for the failure of surgical treatment are the inadequate selection of material for eliminating the bone cavity and the traditional methods used to close defects in the integumentary tissue in the heel area [8,10].
Significant progress in reconstructive plastic microsurgery in the treatment of the consequences of wartime and peacetime injuries is a reliable, well-proven method of medical and social rehabilitation of patients with purulent pathology of the foot.
The purpose of the study was to develop technologies for the surgical treatment of patients with osteomyelitis of the calcaneus using blood-supplied autografts using microsurgical techniques to replace foot tissue defects and improve the functionality of the limb [6].
Material and research methods. During the period from 1995 to 2003, 56 patients with chronic osteomyelitis of the calcaneus combined with bone and integumentary tissue defects were operated on. The area of the latter in 38 (68%) patients was up to 50 cm2 and in 18 (32%) more than 50 cm2.
Surgical treatment of osteomyelitis of the calcaneus consisted of traditional sequesternecrectomy of the purulent focus and local myoplasty of the resulting bone cavities and soft tissue defects in combination with either transposition of foot flaps or transplantation of blood-supplied tissue complexes from distant areas of the human body.
Table 1. Types of flaps used in the treatment of osteomyelitis of the calcaneus
| Types of flaps | Abs. | % |
| A) medial plantar fasciocutaneous flap | 8 | 23,5 |
| B) medial plantar fasciocutaneous muscle flap | 5 | 14,7 |
| c) medial plantar fasciocutaneous flap in combination with the peroneus longus muscle | 2 | 5,9 |
| D) medial plantar musculocutaneous flap | 8 | 23,5 |
| D) dorsal foot flap | 5 | 14,7 |
| E) external calcaneal flap | 6 | 17,7 |
| Total: | 34 | 100 |
Table No. 1 shows that most often (67.6%) the medial plantar flap in one form or another was used as a plastic material.
This is due to the fact that the skin structure of the above-mentioned tissue complex corresponds to the texture of the skin of the supporting surface of the heel and calcaneal tubercle, and what is equally important is that it is sensitive and therefore resistant to significant mechanical load.
These factors were decisive when planning the closure of the defect in the integumentary tissue on the plantar surface of the foot in the heel area.
Arterialized foot flaps were used as a plastic material to eliminate bone and soft tissue defects in the heel area while the plantar arterial arch and main vascular bundles of the leg were preserved.
Indications for operations using foot flaps were:
- osteomyelitic ulcers and fistula tracts in the soft tissues of the heel region with a superficial focus of destruction of the heel bone (cortical osteomyelitis);
- parietal and central location of the purulent focus in the heel bone in combination with a defect in the integumentary tissues up to 50 cm in area;
- end-to-end (tunnel-shaped) location of the osteomyelitic lesion in the calcaneus with a defect in the integumentary tissue above it with an area of up to 50 cm;
34 patients were operated on using this surgical technology. The duration of the surgical intervention was on average 5 hours.
Transplants from remote areas of the human body as a plastic material are presented in Table No. 2. They were used to eliminate bone and soft tissue defects in the heel area when one of the main vascular bundles of the leg and (or) the plantar arterial arch was damaged.
Table 2. Types of blood-supplied grafts used in the treatment of calcaneal osteomyelitis
| Types of grafts | Abs. | % |
| A) radial fasciocutaneous graft | 3 | 13,6 |
| B) radial fasciocutaneous-muscular graft | 2 | 9,1 |
| c) radial fasciocutaneous aransilantate in combination with the gastrocnemius muscle | 13,6 | |
| d) radial fasciocutaneous graft in combination with the soleus muscle | 2 | 9,1 |
| D) ulnar fasciocutaneous graft | 5 | 22,8 |
| E) thoracodorsal graft | 4 | 18,2 |
| G) inguinal graft | 3 | 13,6 |
| Total: | 22 | 100 |
Table No. 2 shows that in the majority of patients, forearm tissue complexes were most often (68.2%) used as plastic material in one form or another.
This is due to the fact that the collection of the above-mentioned tissue complexes is less complicated and traumatic in relation to others; The diameter of the vessels of the vascular bundles of both the forearm grafts and the recipient zone of the leg, as a rule, correspond to each other, which greatly facilitates the performance of microvascular anastomoses.
In addition, there was no subsequent need to perform corrective operations, as is often the case when transplanting the latissimus dorsi muscle to the foot.
These factors were decisive in planning the closure of the integumentary tissue defect on the foot with free blood-supplied tissue complexes.
Indications for operations using blood-supplied tissue complexes from distant areas of the body were:
- central location of the purulent focus in the heel bone with subtotal or total damage in combination with a defect in the integumentary tissues above them with an area of more than 50 cm2;
- parietal location of the purulent focus in the heel bone and osteomyelitic ulcers and fistulous tracts in combination with a defect in the integumentary tissue above them with an area of more than 50 cm;
- end-to-end (tunnel-shaped) location of the osteomyelitic lesion in the calcaneus with subtotal damage with a defect in the integumentary tissue above it with an area of more than 50 cm2;
- extensive defects of integumentary tissues with damage to the anatomical structures of several zones of arterial blood supply (proximal, median and lateral plantar) of the foot with osteomyelitis of its bones, including the heel.
22 patients were operated on using this surgical technology. The duration of surgery ranged from 8 to 25 hours.
Treatment results. A positive result of surgical treatment was obtained in 53 patients (94.6%). The occurrence of acute circulatory disorders in transplanted tissue complexes was observed in three patients (5.4%) during transplantation from distant areas of the body.
The average treatment period for chronic osteomyelitis of the calcaneus in the hospital for this group of patients ranged from 24 to 30 days. During dynamic observation after discharge from the hospital for a period of 1 to 8 years, no exacerbation of the osteomyelitic process was noted.
44.5% of military personnel serving under contract continued to serve in the Russian Army without changing their fitness category, and 37.1% of civilians had their ability to work restored.
Conclusion.
The proposed microsurgical technologies for the treatment of chronic osteomyelitis of the calcaneus make it possible to reduce the number of mutilations and move away from the practice of traditional multi-stage reconstructive operations, give a good anatomical and functional result with a small number of complications, and also reduce the length of hospital treatment.
Literature
- Epstein G.Ya. Complications of gunshot injuries to the foot. Experience of Soviet military medicine in the Second World War 1941-1945. Moscow: Medgiz, 1950. – Volume 18. – P. 316-320.
- Nechaev E.A. Mine-explosive injury / E.A. Nechaev, A.I. Gritsanov, N.F. Fomin, IL. Minnullin. – St. Petersburg: JSC “Ald”, 1994. – 487 p.
- Gumanenko E.K. Combat surgical trauma: Textbook. – St. Petersburg, 1997. -72 p.
- Nikitin G.D. Surgical treatment of osteomyelitis / G. D. Nikitin, A. V. Rak, S. A. Linnik and co-authors - St. Petersburg: Russian Graphics, 2000. - 288 p.
- Shapovalov V.M., Ovdenko A.G. Gunshot osteomyelitis. – St. Petersburg: Morsar AV. -2000. -144 pp.
- Patent of the Russian Federation for the invention “Method of surgical treatment of osteomyelitis of the bones of the foot” No. 2161447 with priority from 06/02/1998, registered in the State Register of Inventions of the Russian Federation on January 10, 2001 // Official Bulletin of the Russian Agency for Patents and Trademarks. – No. 9. -2001. – P. 128. (Yurkevich V.V., Polyakov A.A., Podgornov V.V., Kolesnikova I.V.)
- Shevtsov V.I. Rehabilitation of victims with consequences of gunshot wounds of the foot / V.I. Shevtsov, G.R. Ismailov, D.V. Samusenko, A.I. Kuzovkov // Current problems of traumatology and orthopedics. Materials of the scientific conference. – Nizhny Novgorod, 2001. – Part 1. -P. 210-211.
- Efimenko N.A. Surgical treatment of diseases and injuries of the foot / N.A. Efimenko, A.A. Gritsyuk, SM. Rybakov, A.L. Ryabov // Military medical journal. – 2002. – Volume SSSХХШ. – No. 4. – P. 12 – 18.
- Nechaev E.A. Blast injuries: A guide for doctors and students / E.A. Nechaev, A.I. Gritsanov, I.P. Minnullin et al. – St. Petersburg: IKF “Foliant”, 2002. – 656 p.
- Nikitin G.D. Bone and musculoskeletal plastic surgery in the treatment of chronic osteomyelitis and purulent false joints / G.D. Nikitin, A.V. Rak, S.A. Linnik et al. – St. Petersburg: “LIG”, 2002. -192 p.
Bibliographic link
Yurkevich V.V., Bashirov R.S., Podgornov V.V., Pekshev A.V., Kolesnikova I.V., Luzgin V.Yu. New technologies for restorative treatment of patients with calcaneal osteomyelitis // Fundamental Research. – 2004. – No. 2. – P. 35-37; URL: https://fundamental-research.ru/ru/article/view?id=2918 (access date: 03/20/2020).
Source: https://fundamental-research.ru/ru/article/view?id=2918
Causes of osteomyelitis
It is also worth knowing the main reasons for its appearance, because it does not immediately begin to progress and affect even parts of the intervertebral region, if we are talking about this part of the body. If you know how the disease begins to develop, then the clinical picture will not take you by surprise, and diagnostic procedures will be carried out when they are needed. Experts note that the main causative agents of the acute form of this disease are bacteria such as staphylococci, but sometimes the problem lies in other bacteria. But because of one Staphylococcus aureus, the disease usually does not begin; the inflammatory process manifests itself in the presence of precipitating factors, as well as the main causes that directly cause osteomyelitis itself, here are the main ones:
- ARVI;
- injuries of various types;
- burns of varying severity;
- severe frostbite;
- disorders associated with the psycho-emotional state (this can include stressful situations, but most often this occurs due to prolonged nervous exhaustion);
- physical activity that is excessive for the body.
Here are the main predisposing factors:
- the presence of diseases such as tuberculosis and diabetes;
- severe physical exhaustion;
- receiving any injuries, especially if they occur constantly;
- damage associated with the consequences of thermal burns;
- allergic reactions and the diseases they cause;
- severe weakening of the immune system;
- infectious lesions;
- the presence of oncology, as well as the negative effect on the body of chemotherapy used in its treatment;
- fasting for a long time, as well as a lack of nutrients in a person for some other reason;
- surgical interventions and errors made in their process;
- disorders associated with the circulatory process;
- ulcers.
Important! Try to reduce your risk of developing this disease as much as possible. To do this, try to avoid any predisposing factors, and especially the mechanisms that trigger the disease itself!
Treatment methods
Treatment measures for all types of osteomyelitis are carried out according to the same principle. After a microbiological study testing the sensitivity of microorganisms, the doctor determines a treatment regimen (how to treat and which antibacterial drugs are suitable in a particular case). Over the course of a month, the therapeutic strategy is changed, trying new drugs and combinations. To prevent intoxication and improve the functioning of the circulatory system, the patient receives intravenous drips with plasma, hemodez, and a 10% albumin solution.
The acid-base state is restored using sodium bicarbonate. Immunomodulating drugs and vitamin complexes are used as maintenance therapy. For staphylococcal infections, the administration of staphylococcal vaccine and gamma globulin is practiced. Hyperbaric oxygenation is effective - treatment with oxygen in special pressure chambers. During the treatment period, complete immobilization of the limb is indicated.
In the presence of sepsis, extracorporeal hemocorrection is performed. The method allows you to improve the rheological properties of blood and selectively eliminate pathogenic factors. The essence of the procedure is the creation of a temporary blood circulation circuit to purify and modify blood components.
In acute osteomyelitis, drainage of the area of suppuration is mandatory. For this purpose, trepanation holes are made in the bone tissue, through which the pathological focus is washed with antibacterial solutions. Proteolytic enzymes are also used as bioantiseptics. If soft tissues are colonized by pyogenic microflora, the places where pus accumulates are opened and subjected to open lavage.
For complete sanitation of a purulent-necrotic focus, the following is carried out:
- sequestrectomy – excision of fistulous tracts and free sequestra;
- necrectomy – complete resection of necrotic tissue to healthy layers.
Full access to the sequestra located in the medullary canal is ensured by trephination of the long bone. In case of destruction of bone tissue, marginal, end, or segmental bone resection is indicated. The duration of the pathological process and the shortening of the limb are the basis for the use of compression-distraction osteosynthesis using the Ilizarov apparatus.
Physiotherapeutic procedures are introduced into the complex with medicinal and surgical assistance: laser therapy, UHF, ultraviolet irradiation, diadynamic currents.
The final stage of surgical interventions is carried out in the long-term period. Elimination of cavities that have formed - bone grafting - is performed after the infection has been completely eliminated.
X-ray in the initial stages
As mentioned earlier, it is better to do an X-ray examination after you notice that the clinical picture of the disease has begun to appear. At this stage, using X-rays, it is already possible to identify the disease, and its treatment will be quite simple. Most often, doctors use multi-projection x-rays. As for the later stages, only x-rays using hard radiation will help.
The choice of rigidity itself can only be made by a qualified specialist, and it can be influenced by factors such as the rate of development of the disease, features of the course and phase. It is worth mentioning that you can diagnose some forms by taking pictures even with minimal hardness, but others will be quite difficult to notice.
Features of the procedure
As was mentioned earlier in the process of describing the key actions for osteomyelitis, diagnostic procedures associated with x-rays are used most often, but this is not informative in all situations, because sometimes the disease extends to soft tissues (for example, fat, as well as muscles and on tendons). Of course, in some cases, even an x-ray will help to see the problem if its hardness is low, but in such cases it is better to use magnetic resonance imaging. Thus, the specialist will be able to create a complete clinical picture, which will allow the most competent approach to treatment. Without magnetic resonance imaging, diagnosis will not be successful in situations where the lesion is associated with the pelvis or spine.
Specialists always pay attention to what osteomyelitis looks like on an x-ray, because this allows you to learn a lot about it. Modern diagnostic methods make it possible not only to determine the presence of the disease, but also to provide some information about it. Unfortunately, x-rays are not the most informative examinations, and in their process attention is drawn to sequestration and osteonecrosis. Let us mention once again that such a diagnosis using X-rays will only be possible for an experienced specialist, and sometimes even he needs to study images from a repeat X-ray or MRI.
The bone is clearly thickened in places where the inflammatory process develops.
Diagnostic methods
Establishing the correct diagnosis can be difficult, especially with the septic and adynamic form of the disease. Patients are often treated for rheumatism, pneumonia, arthritis, and neurological disorders.
When examining a patient, the doctor palpates the affected limb and notes increased pain and muscle contractures when trying to make any movements. Radiography is important. At the initial stages of osteomyelitis (14–21 days), images record thickening and deformation of soft tissues; later, abscesses, intermuscular phlegmons, cavities in the bones surrounded by sclerotic structures, and narrowing of the medullary canal are revealed.
X-rays do not always provide a reliable clinical picture of the disease, so computed tomography is additionally performed. This diagnostic method helps to identify and assess the extent of inflammation, determine the presence and location of sequesters.
To identify the causative agent of the infectious process, bacteriological culture of purulent discharge is done. Based on the results of the analysis, the most effective antibiotics to which pathogens are sensitive are selected.
What can you see in the photographs?
Here are the main signs of osteomyelitis that can be seen when studying an x-ray (we are talking about the earliest stages, when the lesions are not yet so large):
- There are significant thickenings of the bones in those places where the inflammatory process occurs.
- On the x-ray you can see foci of necrosis called “sequestra”. It is worth understanding that they can be related to both bone and muscle structures, and their appearance will resemble dark circles located directly on a person’s bones (as you might guess, circles on muscle tissue will be light). It is also worth understanding that sequesters always have an irregular shape.
- The images of this disease never reveal the medullary canal.
Each specialist, over the many years of his work, finds his own method of studying images, which he follows in most situations.
Brody's abscess.
Classification
Clinical classification of osteomyelitis is carried out according to many criteria. The more precise the diagnosis, the clearer the treatment tactics become.
Types of disease depending on the pathogen:
- caused by nonspecific microflora (gram-positive or gram-negative): staphylococcus, pneumococcus, streptococcus, proteus, Escherichia coli and Pseudomonas aeruginosa, less commonly anaerobes:
- caused by one type of microbe (monoculture);
- associated with the association of 2 or 3 different types of microorganisms.
- specific for infectious pathology:
- syphilitic;
- leprous;
- tuberculosis;
- brucellosis;
- other.
- no pathogen was detected.
Bactericidal damage to bone layers.
There are clinical forms of the disease:
- hematogenous:
- after an infection of another organ;
- post-vaccination;
- other.
- post-traumatic:
- after fractures;
- after operation;
- when using spoke devices.
- firearms;
- radiation;
- atypical (primary chronic):
- Brody's abscess;
- Ollier and Garré osteomyelitis;
- tumor-like.
Flow options:
- generalized:
- septicotoxic;
- septicopyemic;
- isolated toxic.
- focal:
- fistulous;
- fistulaless.
Character of the current:
- acute (in particular, lightning);
- subacute;
- primary chronic;
- chronic.
The following stages of the osteomyelitic process are distinguished:
- acute;
- subacute;
- ongoing inflammation;
- remission;
- exacerbation;
- recovery;
- convalescence.
Phases of defeat:
- intramedullary (only the bone marrow is affected);
- extramedullary.
Based on localization, osteomyelitis of tubular and flat bones is distinguished. In long tubular bones, different parts can be affected: epiphysis, diaphysis, metaphysis. Among the flat bones affected are the skull, vertebrae, shoulder blades, sit bones and ribs.
Local complications of osteomyelitis:
- sequestration;
- fracture;
- bone, paraosseous or soft tissue phlegmon;
- pathological dislocation;
- formation of a false joint;
- ankylosis;
- joint contractures;
- violation of bone shape and development;
- bleeding;
- fistulas;
- vascular complications;
- neurological complications;
- muscle and skin disorders;
- gangrene;
- malignancy.
Variants of the disease with common complications:
- amyloid damage to the kidneys and heart;
- severe pneumonia with lung collapse;
- inflammation of the pericardium;
- sepsis;
- other.
The most common variants of the disease are acute hematogenous (in childhood) and chronic post-traumatic (in adult patients).
The disease most often affects certain bones of the human body.
Osteomyelitis of the thigh
Symptoms of femoral osteomyelitis.
It is observed in people of any age, most often of hematogenous origin, but often develops after surgery on the bones. Accompanied by swelling of the thigh, fever and impaired mobility of adjacent joints. A large fistula forms on the skin, through which pus is discharged.
Osteomyelitis of the leg bones
Signs of osteomyelitis of the lower leg bone.
It is observed more often in adolescents and adults, and often complicates the course of tibia fractures. Accompanied by redness and swelling of the lower leg, severe pain, and the formation of fistula tracts with purulent discharge. The tibia is affected first, but then the fibula always becomes inflamed. The patient cannot step on his foot.
Osteomyelitis of the calcaneus
Signs of osteomyelitis of the calcaneus.
Unlike the forms described above, it usually has a long course and often complicates infectious diseases of the foot, for example, diabetes. The main signs are pain and swelling in the heel, redness of the skin, and the formation of an ulcer with the release of purulent contents. The patient may have difficulty walking while resting on the front of the foot.
Osteomyelitis of the shoulder
It often occurs in childhood, has an acute course, accompanied by fever, swelling, and pain in the arm. As the disease progresses, pathological fractures are possible.
Metatarsal osteomyelitis
Signs of osteomyelitis of the metatarsal bone.
It develops when the surgical treatment of a wound resulting from a foot injury is insufficiently thorough. It can also complicate the course of diabetes. Accompanied by pain and swelling of the foot, difficulty walking.
Vertebral osteomyelitis
Develops mainly in adults against the background of immunodeficiency or septic condition. Accompanied by back pain, headache, palpitations, weakness, fever.
Examination for chronic osteomyelitis
It is important to briefly examine the research process observed in the chronic form of osteomyelitis. Here is its dependence on the type:
- Hematogenous chronic osteomyelitis. This type of disease is always accompanied by some symptoms manifested in the bone marrow, as well as the periosteum. In this case, on an x-ray you will notice focal clearing.
- Recurrent multifocal osteomyelitis in chronic form. This type is diagnosed localized only if the specialist has correctly chosen the projection of the image. A feature of the disease in this case will be the restructuring of the tubular bone into spongy bone. In this case, in the image you will notice a significant thinning of the periosteum, as well as replacement of the medullary canal with spongy substance. Some areas of enlightenment that were not there before will also appear.
The chronic form is accompanied by a host of other features, but usually patients should not know about this. Under no circumstances try to decipher images yourself in order to save money on visiting a specialist, because this is fraught with dire consequences!
Prevention
If a patient has risk factors for osteomyelitis, he should be aware of them. It is necessary to take all measures to prevent various infections, avoid cuts and scratches, and treat skin injuries in a timely manner. People with diabetes need to constantly monitor the condition of their feet to prevent skin ulcers from developing.
Dental caries, chronic tonsillitis, cholecystitis, and pyelonephritis should be treated in a timely manner. To increase the body’s nonspecific protection, it is necessary to monitor nutrition and physical activity, and lead a healthy lifestyle.
Osteomyelitis of the upper limb.
Osteomyelitis is an inflammatory process in the bone marrow that spreads to the surrounding bone substance. It can have an acute or chronic course and is manifested by bone pain, fever, intoxication, the formation of cavities and fistulas with purulent discharge. Treatment includes surgery and massive antibiotic therapy.
2
I likeClass LikeTweet