How are the research results interpreted?
Normal bones are quite dense and block X-rays well.
Because of this, in the picture they are painted bright white. X-ray semiotics of bone pathology manifests itself in the form of abnormal zones - clearing and darkening. Highlights are areas with a lower density than bones, which have gray-black shades in the image. They may correspond to fracture lines, areas of osteoporosis and inflammatory bone destruction, and malignant neoplasms.
https://www.youtube.com/watch?v=ytcreatorsru
Shades, on the contrary, are areas with an increased level of density. The white color they are painted in is much brighter than the shade of bone. Darkening indicates an impacted fracture of tubular bones and vertebrae, osteosclerosis.
White, clearly defined spots on a bone x-ray indicate the presence of a benign neoplasm such as osteoma. Unlike many other tumors, it consists of bone tissue and has a high density, which is why it appears as darkening rather than clearing.
If an x-ray is taken to monitor the healing of a fracture, it can show the bone calluses that form at the site of the injury and indicate its healing.
On X-ray, the developing callus appears as a slightly darkened cloud around the site where the fracture occurred. After calcification, it appears bright white in the image.
What do the finished photos say?
A healthy bone in a black and white photograph will be almost white without darkening or structural changes. The cartilaginous joints of the ankle joint should also be clearly visualized.
What will an x-ray show in cases of any pathology?
- Closed fractures appear as shadows on a white background.
- Various neoplasms are defined as dark spots with unclear edges.
- Osteomyelitis of the leg on an x-ray is manifested by thickening in areas of inflammation of hard tissues and lighter spots with jagged edges in the area of soft tissues. If the leg is healthy, then the bone marrow canal is clearly visible in the image; with osteomyelitis, it is not visualized.
For diagnostics and diagnosis, specialists also take into account the following normative indicators of healthy norms and deviations:
- The shape, size and arrangement of elements in relation to each other. If the shape changes after receiving a certain load, a diagnosis of hyperostosis or atrophy is made.
- Structure. Increased density indicates osteosclerosis. An overly thinned outer layer in addition to darkened areas on the white bone structures indicates advanced osteoporosis.
- Surface of the bone. Any changes in the outer layer of bones (destruction, ossification, detachment) may indicate the development of cancer.
- The gap between the joints. An unevenly narrowed gap is a sign of arthrosis.
- Foot angle. A sign of flat feet is considered to be a foot angle greater than 130 degrees.
Bandaged leg
Although the dose released during an X-ray image of a section of the tibia or fibula bone is minimal, X-rays should be avoided: for pregnant women; children at an early age (the doctor discusses this issue with the child’s parents); people in critical condition.
X-ray with contrast agent
There are no special contraindications. If a person is in extremely serious condition, then in some cases this procedure is canceled. It's all about the contrast agent, without which an x-ray of the shin bone is impossible. However, in most situations it is given to patients even though they may have an allergic reaction. Otherwise, it is difficult to draw any conclusions about the nature of the fracture and understand what actions should be taken.
X-rays can reveal foreign bodies and how much the bone is displaced. After this, treatment is prescribed. Subsequently, a repeat x-ray is performed. If a cast is applied to the lower leg, this does not mean that the process of bone fusion cannot be checked using the device.
During the procedure, the patient must take one of two positions: either lying on his back or on his side. In the second case, he should twist his healthy leg so that it does not interfere with the study. X-rays are available to anyone. You can go to a clinic, trauma center, etc. Moreover, everything is carried out absolutely free of charge or for a purely nominal fee.
If you fracture your tibia, you should immediately go to the nearest medical aid station, where they will take an x-ray and determine the extent of the fracture. You can also take an x-ray of the shin bone in our medical centers.
Such technologies are used infrequently, but sometimes they are extremely necessary. The procedure is performed using contrast agents. Human bones differ from other body tissues in their increased natural contrast. There are several radiopaque techniques for studying bone tissue:
- fistulography;
- pneumography;
- arthrography;
- angiography.
Thanks to the use of a contrast agent, clearer information is obtained, hence the quality of care. The downside to this type of bone diagnosis is that there are contraindications and some limitations; in addition, the radiologist must have extensive experience.
| Name of service | Price, rub.)* |
| Description of the presented radiographs | 850 |
| Intraoperative cholangiography | 18 700 |
| Intraoperative X-ray control | 7 100 |
| Irrigoscopy | 4 400 |
| Contrast study of the maxillary (maxillary) sinuses in 2 projections | 1 900 |
| Mammography of 2 mammary glands in 2 projections | 2 600 |
| Mammography of 1 breast in 2 projections | 1 350 |
| Adjusting the gastric band | 4 400 |
| X-ray of the 1st cervical vertebra with open mouth | 950 |
| X-ray of the thigh or lower leg, or shoulder, or forearm in 2 projections | 1 550 |
| X-ray of the abdominal cavity (survey) | 2 150 |
| X-ray of the temporal bones according to Schuller or Mayer on both sides (2 images) | 2 050 |
| X-ray of the eye sockets or cheekbones, nasal bones in 2 projections | 2 150 |
| X-ray of the thoracic and lumbar spine in lateral projection | 2 600 |
| X-ray of the thoracic spine (2 images) | 2 150 |
| X-ray of the floor of the mouth (according to Kovalenko) | 950 |
| X-ray of the clavicle, scapula, sternum | 1 550 |
| X-ray of the pelvic bones | 2 250 |
| X-ray of the urinary system (survey) | 1 550 |
| X-ray of the lower jaw in 2 projections | 2 050 |
| X-ray of the nasopharynx - lateral projection (1 image) | 1 800 |
| X-ray of the chest organs (survey) | 1 550 |
| X-ray of the chest organs in 2 projections | 2 250 |
| X-ray of the chest organs in lateral projection | 1 350 |
| X-ray of the lumbar spine in 2 projections | 2 150 |
| X-ray of the paranasal sinuses in the 1st projection (1 image) | 1 550 |
| X-ray of the paranasal sinuses in 2 projections (2 images) | 1 900 |
| X-ray of the ribs (2 images) | 1 800 |
| X-ray of the feet (for transverse flatfoot) with functional load (1 image) | 1 700 |
| X-ray of the feet (for longitudinal flat feet) with functional load (2 images) | 1 900 |
| X-ray of the foot or hand, heel, ankle joint in 2 projections | 2 250 |
| X-ray of the hip, knee, shoulder, elbow, wrist joints in 1 projection | 1 700 |
| X-ray of the hip, knee, shoulder, elbow, wrist joints in 2 projections | 2 250 |
| X-ray of the skull in 2 projections | 2 150 |
| X-ray of the cervical spine in 2 projections | 1 800 |
| X-ray of the stomach, duodenum | 3 200 |
| X-ray of the esophagus | 2 600 |
| Salpingography | 3 200 |
| Urography intravenous | 4 400 |
| Fistulography | from 3 500 |
| Functional images of the cervical spine (2 images) | 2 150 |
| Functional images of the lumbar spine (2 images) | 2 250 |
| Cone beam computed tomography of both jaws for SM-Clinic patients upon referral from the attending physician (without description by a radiologist) | 3 010 |
| Contrast radiography of the small intestine (barium passage) | 3 950 |
| Cystography | 2 800 |
| X-ray of the sacrum and coccyx in the 1st projection | 1 250 |
| X-ray of a finger or toe in the 1st projection (1 image) | 800 |
| Description of a three-dimensional X-ray examination (on a dental 3D computed tomograph “Galileos”), size 15x15 cm | 1 600 |
| Description of a three-dimensional X-ray examination (on a dental 3D computed tomograph “Galileos”) measuring 5x5cm, 8.5x5 cm (one jaw, ENT area) | 1 200 |
| Description of three-dimensional X-ray examination (using a dental 3D computed tomograph “Galileos”) of the TMJ (one joint) | 1 200 |
| Description of three-dimensional X-ray examination (using a dental 3D computed tomograph “Galileos”) of the TMJ (two joints) | 2 400 |
| Description of orthopantomogram (OPTG) | 800 |
| X-ray of the temporomandibular joints on both sides (4 images) | 4 050 |
| X-ray of the sacrum and coccyx in 2 projections | 1 700 |
| X-ray of a finger or toe in 2 projections (2 images) | 1 250 |
| X-ray of the nasolacrimal duct with contrast in 2 projections | 2 500 |
| Angiography of peripheral vessels | 20 500 |
| Coronary angiography | 23 500 |
The posted price is not an offer. Medical services are provided on the basis of a contract.
Dr Nona in Kazan -{amp}gt; , Treatment of osteoporosis during menopause - Traditional and alternative medicine , Osteoarthrosis of the knee joint: degrees of the disease, symptoms , Treatment of osteoporosis , Arthrosis of small joints: how to get rid of pain in the arms and feet ,
Types of X-ray examinations
Radiation diagnostics of bones occurs using various units and research methods. It all depends on some factors:
- patient's age;
- clinical situation;
- underlying pathology;
- associated factors.
This method is indispensable in recognizing the causes of pathology and plays an important role in making the correct diagnosis and treatment of the patient.
In medical practice, there are the following types of bone x-rays:
- Film radiography.
- Digital.
- CT scan.
- X-ray densitometry.
- X-ray of bones using contrast agents and other methods.
All these devices serve as an excellent aid to doctors in providing the necessary assistance for:
- bone fractures and dislocations;
- clarification or detection of the location of bone fragments during fractures;
- identifying foreign bodies in soft tissues or in the bones themselves;
- control of orthopedic surgical interventions (joint replacement, spinal stabilization, etc.);
- specification of certain diagnoses (arthritis, pathological proliferation of bone tissue, arthrosis and others);
- suspected bone cancer.
Having received the results of these studies, the specialist already has a more objective picture and draws appropriate conclusions.
X-ray of the lower leg bones at the Yauza Clinical Hospital
X-rays of the leg bones in our hospital are performed by experienced radiology specialists using the Digital diagnost digital radiographic system (Philips, the Netherlands), which provides:
- high-quality image at maximum research speed due to digital signal transmission;
- convenience of the procedure (flat panel detectors allow you to obtain images in the required projection without moving the patient);
- instant availability of the received images to the doctors treating the patient (all images are sent immediately via Wi-Fi to the hospital server).
The results of our radiation diagnostics comply with all strict international protocols and are accepted in any medical institution in the world.
You can see prices for services
The article was checked by radiologist M.A. Petrova. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
"Pros" and "cons" of X-ray examination
Radiography is the fastest and most inexpensive way to assess the condition of bone tissue. Equipment for it is available in almost every medical center. In this regard, this type of research is intensively used even for diagnosing emergency conditions. The radiation dose is small and does not cause any disturbances in the adult body. After the examination, there is no need for rehabilitation of the patient.
But sometimes, due to low resolution, x-rays of the humerus, foot, skull and other parts of the skeleton do not allow us to examine minor pathological changes in bone tissue. In addition, X-rays cannot assess the condition of blood vessels, nerves, and soft tissues around the bones. For this purpose, other types of diagnostics are prescribed - computed tomography (CT), magnetic resonance imaging (MRI).
Osteomyelitis on x-ray: signs on x-ray (image)
Radiography can reveal the presence of osteomyelitis of bone tissue in a patient.
Sometimes the disease is clearly visible (especially if it has spread widely), sometimes very poorly (in the initial stages). An x-ray is capable of identifying indirect signs of its presence (even if it cannot accurately confirm osteomyelitis in the early stages). That is, after such a procedure, more informative diagnostics (computer or magnetic resonance imaging) may be required.
Is osteomyelitis visible on x-ray, and how exactly?
X-rays in most cases show indirect and sometimes (if the process is widespread) direct signs of osteomyelitis. X-rays are often used to monitor the dynamics of the disease during its active (aggressive) treatment.
Modern digital X-ray machines are able to detect osteomyelitis in the early stages. This is possible due to the fact that the x-ray does not show intermuscular and fascial septa, which should normally be present.
X-rays can be used in the diagnosis of osteomyelitis for any part of the bone apparatus. X-rays will show the condition of the lower leg and jaw especially well due to their relatively large size, ease of diagnosis and the absence of tissues that distort the image (for example, ligaments).
Osteomyelitis on X-ray
Typically, a narrow-profile technique is used for diagnosis - multi-projection x-ray. However, classical radiography performed on a digital device will also show the disease (from the sixth day of its development).
The disease is visible on x-rays as pathological compactions, visualized by the loss of sharp boundaries in the deep layers of muscle tissue. Problems may arise with the diagnosis of infiltrates in tendons and muscles - radiography is not intended for examining such tissues.
It is possible to determine the disease in soft tissues by indirect signs. For example, by reducing the rigidity of rays passing through the muscle layers. But such a description of the image requires re-checking with more sensitive techniques (for example, using MRI).
Comparison with other diagnostic methods
X-ray is a good, but not the best, method for diagnosing osteomyelitis occurring in bone tissue. Problems arise with the diagnosis of complications of osteomyelitis in the form of purulent leaks into soft tissues or suppuration of wounds.
Therefore, a full diagnosis using radiography alone is not possible, even with the most modern devices. In this regard, other visualization methods can be used:
- Magnetic resonance imaging - allows you to visualize not only bone, but also soft tissue (cartilage, muscles, ligaments/tendons).
- Computed tomography visualizes bone tissue much better than x-rays.
- Fistulography is used to detect complications of osteomyelitis in the form of sequestration and fistulas.
Tomography is mandatory for the differential diagnosis of osteomyelitis with other inflammatory diseases (including malignant neoplasms). Only tomography can detect signs of early osteonecrosis and sequestration.
Detection of such early complications significantly improves the prognosis, since the sooner they are detected, the sooner their treatment will begin. Tomography can also detect layered periostitis in the early stages, which is evidence of a re-exacerbation of the disease.
Acute osteomyelitis on x-ray
It turns out that X-ray diagnostics is excellent for the primary diagnosis of osteomyelitis and for the management (monitoring) of patients. But for a full examination, tomography is required, often with the addition of fistulography.
Indications and contraindications for the procedure
X-ray diagnostics to detect osteomyelitis is carried out in cases where the patient has symptoms of the disease. The problem is that in the initial stages, osteomyelitis can manifest itself in different ways: from mild discomfort to urgent conditions that require an immediate response.
General list of symptoms and indications for x-ray:
- increase in body temperature up to 40 degrees;
- severe general condition of the patient due to intoxication;
- episodes of syncope (loss of consciousness), stupor, delirium;
- unmotivated hypercalcemia or hyperkalemia;
- the patient has metabolic acidosis, hyponatremia;
- diffuse purulent lesion (ulcers are localized in various areas of bone tissue, development of purulent destructive pneumonia or pericarditis);
- in the fulminant (adynamic) form of osteomyelitis, severe toxicosis, convulsions changing to adynamia, severe decrease in blood pressure, and cardiac dysfunction are observed;
- suspicion of the presence of serous or purulent exudate in the joint sac;
- hyperemia (redness, palpable sensation of heat) of the skin over the affected bone or joint tissue.
Contraindications (relative) to the procedure:
- The patient is in serious condition, cachexia, fever (more than 39 degrees).
- The presence of tattoos in the examined area made using metal-containing substances.
- Aggressiveness and increased nervous excitability of the patient, violence.
- Severe inflammatory processes in the area being examined (can distort the x-ray).
What needs to be examined and how much does it cost?
The area of bone or joint tissue in which the pathological processes are localized is subject to examination. When the disease is generalized (systematic), examines all or most of the areas in which symptoms are observed (for example, ulcers).
X-ray visualization of osteomyelitis
If individual bone elements (jaw, foot, leg) are affected, they should be fully diagnosed, without focusing only on the location of the pathological focus. That is, if the lower jaw is affected, then the healthy upper jaw is also examined - the pathological process may already have begun there (subclinically).
Diagnosis of suspected osteomyelitis is carried out in clinics and hospitals. The procedure is carried out free of charge (if the severity of symptoms is minimal, the examination is carried out on a first-come, first-served basis).
You can also undergo the procedure in private medical institutions, but not every private clinic has an X-ray machine. The cost of the procedure in private clinics is 300-700 rubles. The cost in public clinics or hospitals rarely exceeds 300 rubles.
Osteomyelitis: general information (video)
Source: https://osankino.ru/diagnostika/osteomielit-na-rentgene.html
Digital and film X-ray of bones
At the beginning of research in this area, a photosensitive screen or film was used as a receiving element. Today, X-ray film is the most popular detector of electromagnetic radiation.
But digital radiography showed the best results. Here the receiving element is sensors sensitive to X-ray radiation. This type has many advantages:
- high sensitivity of digital sensors allows you to reduce the radiation dose;
- increasing image resolution and increasing accuracy;
- no need to process photosensitive film;
- quick and easy image acquisition;
- ease of processing, transmission and storage of information.
The only drawback is that the equipment is expensive, so not all medical institutions have it.
The difference between spotty and diffuse
https://www.youtube.com/watch?v=ytcopyrightru
The main types of osteoporosis are spotty and uniform (diffuse). What they have in common is increased transparency of the bone pattern. In the spotted form, even lighter lesions appear on a light gray or normal background. They can be single or numerous, round, polygonal or oval. Their outline is not clear, and their size is 2-5 mm. The cortical zone does not change or acquires a loose (spongy) structure.
Diffuse osteoporosis has a uniformly transparent appearance without a spotty pattern. Bone substance consists of thin partitions (trabeculae) that do not block x-rays much. The bones are like glass with an accentuated shell (cortex).
These two types are often successive stages of osteoporosis - spotty early, and uniform later, but can also occur as independent variants of the disease.
X-ray and computed tomography (CT)
This method is even more accurate and informative. With its help, a three-dimensional image of any bone in the body or sections through any bone in different projections is obtained. A very accurate diagnostic method, but it carries with it a high radiation dose.
Advantages of CT over conventional bone x-ray:
- accuracy and high resolution;
- three-dimensional reconstruction of the body part being studied;
- the admissibility of obtaining any projection when conventional x-rays are performed in only two or three projections;
- the image is undistorted;
- in parallel, you can examine soft tissues and blood vessels;
- the research is carried out in real time.
CT scans are performed no more than once a year due to high radiation exposure. Complex pathologies are usually examined (intervertebral hernias, osteochondrosis, tumor diseases).
Thanks to this type of x-ray, a clear image of the internal structures of the body is obtained in various planes. Three-dimensional reconstruction of human tissues and organs is also performed. Radiation exposure during MRI examination is reduced to zero.
The operating principle of the device is based on giving the atoms that make up the body a magnetic impulse. After this, the energy released by the atoms when returning to their original state is read out.
This method cannot be used if there are pacemakers or implants in the body. Diagnostics are expensive and this is considered a disadvantage.
How is the procedure done?
X-ray of the ankle takes little time and does not require special preparation. The patient's body, with the exception of the area being studied, must be protected at the time of filming with a special apron that shields ionizing radiation.
An x-ray of the lower leg is taken in two projections: direct and lateral. If these projections are not enough to make a diagnosis, an x-ray is taken in oblique projections (at different angles), as well as an x-ray of the foot with a load
.
Osteoporosis of different localizations in the picture
When reading an x-ray of a bone, the radiologist pays attention to the size, shape, and position of the structures shown. Describes the offset.
In the second step, the structure of the external, internal contours of the cortical layer along the entire length is analyzed in order not to miss the “greenstick” fractures found in children. Pathological periostitis (inflammation of the periosteum) can occur with cancerous tumors. Based on the results of the x-ray, osteomyelitis is established - purulent melting of the bone.
If a photograph of the upper or lower extremity is taken on a child, an assessment of the state of the ossification nuclei is required.
These structures appear at a certain time. Caused by the transformation of cartilage tissue into bone. The absence of a focus of bone ossification at the required time indicates developmental delay and genetic diseases.
It is important to evaluate the timing of ossification and the symmetry of the appearance of ossifications on both sides.
1. Outlines of the epiphyses; 2. Condition of the endplate; 3. The size of the joint space; 4. Location, external contours of the articular ends of the bones.
The description of the bone image by the radiologist contains information about all the criteria described above - changes in contours, volume, size, surrounding soft tissues.
X-ray of the forearm bones is normal: Koval’s scheme
An X-ray of a fused bone may be no different from the norm or show excess callus or improper fusion of fragments.
Typically, three zones are chosen to diagnose bone changes - hand, hip, spine. If necessary, examination of periarticular bone formations is also carried out, for example, near the knee joint.
In patients with primary osteoporosis (menopausal, senile and juvenile), the limbs are the last to be affected. In some forms of secondary (against the background of other diseases) changes in the area of the radius are the first sign.
When bone tissue is destroyed, the photographs reveal:
- narrowing of the cortical layer;
- expansion of space for bone marrow;
- increasing the transparency of the spongy part;
- emphasized structure of the bone beams.
Several variants of lesions of the metacarpal bones have been identified, which can help in establishing the cause of the development of osteoporosis:
- trabecular and intracortical - disintegration of the cortical zone and spongy part with a decrease in density. Characterizes the menopausal process of bone loss;
- endosteal (from the bone marrow) – the cortical area is destroyed from the inside of the bone, which happens in the senile version of the disease;
- subperiosteal (under the periosteum) – loss of external density, accompanies hyperparathyroidism (increased function of the parathyroid glands).
Bone densitometry
This is a modern non-invasive method for determining bone density, performed to diagnose osteoporosis. With this pathology, the content of minerals in the bones is reduced, usually calcium, which causes bone tissue to become fragile. Osteoporosis is most dangerous for the femoral neck and spine.
There are several types of such research:
- Ultrasound densitometry is the safest non-radiation modern method for determining bone density.
- X-ray densitometry is a highly accurate method for determining the mineral mass of bone tissue.
- Photon absorptiometry—measures bone absorption of a radioisotope.
The method allows you to detect the slightest loss of density (from 3 to 5%). The higher the loss, the worse the bones' resistance to damage. The method is based on the degree of reflection of ultrasonic waves from the surface of the bones. Advantages of the method:
- the procedure does not last long;
- financially accessible;
- no pain;
- can be given repeatedly to pregnant women.
How harmful is a bone density x-ray? The absence of radiation exposure shows that this method is absolutely harmless.
This study in childhood
In a child, this type of study is often used to diagnose such a common disease as congenital hip dislocation. Joint damage is often unilateral. After examining the child by a doctor and if there is a suspicion that the child has a pathology of the hip joints, the doctor prescribes a diagnosis:
- If the child is under 4 months old. ─ ultrasound examination of the hip joints.
- If the child is older than 4 months. ─ X-ray examination may be used.
When interpreting a radiograph in a child, it is important to remember that at an early age the acetabulum and femoral heads consist of cartilaginous tissue and do not create contrasting shadows.
X-ray signs of hip instability include:
- Smoothness of the articular cavity.
- Late-appearing ossification nuclei in the femurs of a child.
In case of subluxation, along with the listed signs of instability, there is non-closure of the head of the child’s femur with the acetabulum.
For hip dislocation:
- Smoothness of the articular cavity.
- The femoral head is smaller than on the healthy side, flattened and located outside the socket.
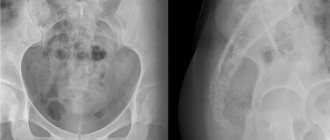
Congenital hip dislocation
Osteomyelitis of the tibia on x-ray
During the development of osteomyelitis, an X-ray examination is performed in order to establish a final diagnosis, as well as clarify the extent of the pathological process and monitor the dynamics of the disease.
In an image taken in the initial stages of the disease, it is impossible to localize intermuscular and fascial septa, which are normally visible in healthy people. During the pathological process, the line between the muscle structure and subcutaneous tissue disappears, and the saturation and volume of soft tissue structures also increases.
What does osteomyelitis look like on an x-ray?
Osteomyelitis is a purulent inflammation of bone structures. Confirmation of the diagnosis is carried out using x-ray diagnostics.
Subsequently, the technique is used to visualize the dynamics of the process, the effectiveness and efficiency of therapy.
Osteomyelitis is difficult to detect on X-ray in the initial stages; careful selection of the degree of radiation is necessary; in the later stages of the disease, tissue lysis and the appearance of an inflammatory infiltrate leaves no doubt about the correctness of the diagnosis.
X-ray technique
If osteomyelitis is suspected, it is necessary to select the optimal dose of X-ray radiation. The higher the hardness of the rays, the more contrast the image and the better the inflammatory areas are visible.
The chronic course of the pathology requires mandatory research. This is necessary to clarify the degree of damage and control the dynamics of the development of the process, since the study expands the field of view and helps the doctor fully imagine the volume of the lesion.
Source: https://geraklionmed.ru/osteomielit-bolshebertsovoy-kosti-na-rentgene/