The spinal column and adjacent soft tissues can be affected by tumor, infectious-inflammatory, post-traumatic, degenerative-dystrophic diseases, as shown by MRI of the thoracic spine after diagnosis. The procedure allows the doctor to see a layer-by-layer image of an organ or circulatory system (even individual parts of a vessel) in a three-dimensional image.
The thoracic spine is a rigid frame that includes the ribs, sternum and 12 vertebrae. Individual vertebrae are least susceptible to injury, since they practically do not touch. The most common pathologies of the thoracic region are disorders of blood flow and metabolism. Such conditions cannot be detected using CT or X-ray, which is why in some cases an MRI of the thoracic spine is necessary.
When is magnetic resonance imaging prescribed?
An MRI of the thoracic spine is required when a patient requires surgery. The study is carried out both before and after surgery, as well as as part of postoperative monitoring.
MRI is indicated when necessary:
- diagnose osteochondrosis, stenosis, encephalomyelitis and a number of other pathologies;
- identify foci of infections, tumor formations;
- assess the degree of damage to the area under study due to fractures, bruises, displacement;
- monitor the condition of bone and surrounding tissues at the final stages of recovery.
The doctor also prescribes an MRI scan when the patient complains of discomfort in the chest area or between the shoulder blades. This can be pain, sensations of squeezing, tingling, sometimes with “recoil” in the limb. Investigation is necessary to determine the source of these symptoms.
Sometimes a problem in the thoracic spine causes pain in the heart, stomach, pancreas, liver, and kidneys. With such symptoms, MRI becomes the stage of differential diagnosis.
Indications for the study
Magnetic resonance imaging can be performed both as a primary diagnosis and to confirm an earlier diagnosis. The main indications for the study are:
- injuries (especially if they are invisible on x-rays - soft tissue damage);
- congenital anomaly in development, impaired blood circulation;
- inflammatory process, infectious disease;
- back pain, poor posture and stoop;
- spinal canal deformity;
- stiffness of movements in the chest area;
- numbness or tingling in the limbs;
- changes in systemic diseases;
- osteochondrosis (diagnosed or requiring confirmation);
- control after surgery or therapy;
- preoperative preparation.
How to prepare for the examination
Typically, no preparation (or diet) is needed for an MRI of the thoracic spine. The procedure can even be performed on an outpatient basis. But you need to prepare for a magnetic resonance examination with contrast (the drug is prepared for intravenous administration for better visualization of the lesion in the intervertebral space) - the patient prepares not to eat for 5-7 hours before the magnetic scanning session. If contrast is planned, it is recommended to take a urine test in advance to rule out kidney disease.
Standard training rules include only a few points.
- On the eve of the procedure, visit a therapist to rule out contraindications.
- Warn the doctor about diseases and conditions that can interfere with the procedure - claustrophobia, epilepsy, and other neurological pathologies. You may have to take a sedative.
- Before entering the room with the tomograph, you need to remove all metal and electronic objects - belts, jewelry, braces, mobile devices, hearing aids, plastic cards, and so on.
What are the contraindications to the procedure?
Is it harmful to have an MRI if there are no contraindications? The answer is no. But for some people the procedure is still not allowed. Contraindications for MRI of the spine are:
- The presence of any metal objects implanted in the body (prosthetic heart valves, inner ear implants, nerve stimulators, pacemakers).
- Contraindications to MRI do not apply to orthopedic joint prostheses, but they may distort the results obtained.
- Pregnancy in the first trimester. The harm from MRI to the fetus has not been proven, but doctors recommend holding off.
- The patient has any mental illness.
Is MRI of the spine harmful for children? Sometimes it is quite problematic to perform an examination on children under 6 years of age: it is difficult for a child to lie still on a hard surface for as long as the MRI lasts, but the procedure is completely safe.
How to do an MRI of the spine
The entire MRI procedure of the thoracic spine takes approximately 20 minutes (when using a contrast agent - 40 minutes, it is administered before turning on the machine). Scanning proceeds as follows.
- Before the scan begins, the client may be asked to put on a disposable hospital gown. Of your clothing, you are allowed to leave only your underwear (if the bra clasps have metal objects, this part of the wardrobe is also removed).
- After changing clothes, the person lies face up on the machine table. The head and limbs are secured with straps, and comfortable cushions are placed under them. These precautions are necessary to ensure that the patient does not accidentally move and interfere with the accuracy of the result.
- An MRI is done in the same way as a CT scan. The table with the patient slowly moves into the closed scanner tunnel. If an open-type apparatus with a movable table is used, then the screen with emitters and detectors is located exactly above the person.
- The subject lies motionless while the scanner reads the information and transmits it to the computer. There may be a slight noise when the tomograph ring rotates. If it causes discomfort, you are allowed to use earplugs. Otherwise, there are no inconveniences during the scanning procedure.
While the patient is lying on the table, the doctor, located in the next room, watches him through the window and maintains communication via a special intercom. The microphone is built into the tomograph camera.
At the end of the examination, the patient waits for the results to be deciphered and can go home. No rehabilitation required.
Features of magnetic tomography
The device is an open, closed type, presented in the form of a ring passing through the center of a horizontally placed magnetic capsule. The patient, having changed into a disposable set of clothing, is placed on a movable table, which slowly moves inside the capsule.
During MRI diagnostics of the thoracic spine, you will have to lie on your back. The head, chest, and arms are secured with belts. The patient may be offered a pillow or blanket. The patient must not move or talk (except when it is necessary to contact a specialist through an equipped microphone).
MRI image of the thoracic spine
A patient preparing for an MRI scan of the spine should be prepared to hear a lot of noise from the equipment. If the patient is uncomfortable with the sound, he can ask for earplugs or headphones.
If the subject is nervous, he is offered sedatives. Discomfort or pain during the diagnostic process is not a typical occurrence. There may be a feeling of swelling and stiffness of the body. There will be a feeling of warmth in the area of examination (in the sternum), colic - this is normal and goes away very soon.
If a patient notices signs of nausea, vomiting, pain, dizziness, or difficulty breathing, it is necessary to immediately report this to a specialist.
The scanning time is 20-40 minutes. If a contrast agent is used, the session may last up to an hour.
Osteochondrosis
At the end of the study, the patient can get dressed and leave the office. There are no rest, restrictions on food and drink after MRI of the spine. The results are delivered to the patient after an hour. In severe cases, the conclusion is issued the next day.
What will an MRI of the thoracic spine show?
Traumatologists, neurologists, vertebrologists and other specialized specialists choose MRI of the thoracic spine because it shows in detail the structure of the vertebrae and surrounding tissues. It helps to identify and analyze:
- congenital anomalies of the spinal cord, vertebrae;
- degenerative changes in the anatomical structure and position of intervertebral discs - hernias, protrusions and other forms of osteochondrosis;
- violation of the structure and position of the vertebrae - spondylolisthesis and similar diseases;
- damage, deformation of the spinal column of a traumatic nature;
- stenosis and vascular pathologies of the spinal cerebral canal, including hemorrhages, stroke;
- Bekhterev's disease;
- neoplasms in the tissues of the studied area, including malignant ones;
- foci of inflammation and infections, including ostiomyelitis.
By analyzing what an MRI of the spine can show in general, a specialist can:
- to find out the nature of anomalies in the intercostal space and spine - congenital or acquired, for example, as a result of injury, chronic disease;
- determine the degree of degenerative changes in the intervertebral discs;
- control the development of ankylosing spondylitis, spondylolisthesis and other chronic pathologies;
- assess the risk of strokes, hemorrhages;
- understand whether the diameter of the spinal canal is normal, and so on.
MRI with contrast reveals the location of tumors and foci of infection. The coloring agent used is concentrated in such places.
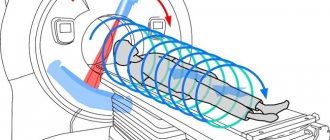
What is MRI?
MRI as a diagnostic method was discovered by scientists at Stanford and Harvard universities and is based on the ability of hydrogen atoms to absorb the energy of a magnetic field and release it in the form of a radio signal (the so-called NMR - nuclear magnetic resonance). During the examination, the tomograph receives a signal and creates images of certain tissues, which are displayed on a computer monitor in the form of 2D and 3D images. Now this research method is used all over the world, but, as a rule, the necessary equipment is available only in large medical institutions, as it is not cheap.
Magnetic resonance imaging
On a note! This method of examining the spinal column was first demonstrated in 1982 in Paris at an exhibition of radiologists.
A Brief History of MRI
MRI makes it possible to obtain the most accurate and reliable data on the condition of tissues and organs of the body, including all elements of the spine (intervertebral discs, spinal cord, blood vessels, etc.). It will allow us to identify a number of diseases at the earliest stages of development, including tumor, inflammatory, degenerative-dystrophic and other pathologies.
MRI allows you to obtain very accurate and reliable data
Indications for examination
MRI of the thoracic spine is indicated for:
- diagnosis of osteochondrosis;
- diagnosis of diseases of the central nervous system (CNS) with inherent demyelination;
- identification of intercostal neuralgia;
- detection of tumors and metastatic processes;
- localization of foci of inflammation, development of infection, abscess;
- detecting the location of narrowing of the spinal canal;
- diagnosis of vascular pathologies;
- assessing the severity of traumatic injuries;
- monitoring of chronic diseases, including congenital ones;
- monitoring the condition before and after surgery;
- complex diagnosis of systemic diseases.
Osteochondrosis is called a “chameleon disease”. Pinching of local nerves provokes pain in areas that are not usually associated with back problems. Often, clinical symptoms mislead specialists who suspect diseases of the internal organs - the heart, stomach or liver. MRI helps differentiate the diagnosis. It is indicated for patients who complain of:
- acute painful sensations in the heart area, back between the shoulder blades;
- girdle pain, feeling of stiffness, numbness in the chest;
- shooting pain between the ribs;
- abdominal pain (in the stomach or liver), worsening after physical activity;
- sexual dysfunction.
Indications
The thoracic spine is a complex system consisting of 12 vertebrae, ribs attached to them, joints, intervertebral discs, etc. This part of the spinal column is less mobile than others, and therefore less likely to suffer from various injuries. But, nevertheless, pain in this area is far from uncommon . It is usually caused by problems with metabolism, due to which the nutrition of the intervertebral discs deteriorates. Over time, this problem will lead to the development of osteochondrosis.
Inside each vertebra there is a small hole through which the spinal cord passes. And as a result of changes in the size of this channel, compression of the nerve endings can occur. Hence the pain syndrome that arises again.
Indications for MRI
On a note! Often problems with internal organs arise precisely because of disruption of the spine.
MRI is a painless, safe and non-traumatic research method. The doctor refers the patient to a tomography if the following indications exist:
- chest pain;
- migraines and dizziness;
- pain in the shoulder blades;
- numbness of the upper extremities;
- swelling of the neck and face;
- cough;
- upcoming surgery;
- weakness in the legs;
- suspicion of a disease of the nervous system;
- difficulty moving.
Osteochondrosis of the thoracic spine
MRI is also performed if the development or presence of a number of diseases is suspected - osteochondrosis, kyphosis, intervertebral hernias, tumors, tissue infection, etc. They can be triggered by an incorrect lifestyle, insufficient or excessive load on the body, and injuries.
Prices for orthopedic corsets and posture correctors
Table. Symptoms that require an MRI.
| Symptom | Characteristic |
| Heart-like pain | Most often, the cause of this type of pain is osteochondrosis (from the point of view of the musculoskeletal system). Tomography will reveal the true cause. |
| Discomfort between the shoulder blades | Such symptoms are characteristic of osteochondrosis, scoliosis and kyphosis, and can be provoked by protrusions, the presence of hernias, and injuries. Due to the fact that MRI demonstrates the condition of all tissues, identifying these pathologies is not difficult. |
| Girdle pain in the chest area | Often observed in cases of problems with the functioning of internal organs, including the heart. They can also signal pathological changes in the spine. |
| Intercostal neuralgia | The pain syndrome in this disease is quite obvious. The causes may be intervertebral hernia, osteochondrosis. |
| Chest tightness | A common sign of developing osteochondrosis. May have a different character. |
On a note! Tomography is usually prescribed by a doctor, but you can undergo it at your own request without medical indications.
You can get an MRI without a doctor's prescription
Contraindications
There are few contraindications for examining the thoracic spine using MRI. One of the main ones is non-removable metal objects or devices that can affect the magnetic field. This:
- metal implants, prostheses, vascular clips;
- insulin pumps, cardiac and nerve stimulators, hearing aids.
Relative contraindications to scanning are claustrophobia, hyperkinesis and other conditions in which it will be difficult for the patient to stay in the tunnel, remaining calm and still. Sometimes they resort to sedatives or put the subject into medicated sleep. For the same reason, the procedure is rarely prescribed for children under 7 years of age.
Persons whose life support is supported by hardware are not allowed to participate in the procedure. MRI is not recommended for pregnant women in the first trimester. There are restrictions on body weight (up to 130 kg), which is explained by the design of the equipment.
MRI of the thoracic region with contrast is contraindicated in pregnant women, nursing mothers and patients suffering from renal failure, as well as in cases of allergies to the components of the drug.
Alternative research methods
MRI is considered to be the most informative and safe examination. Tomography does not carry radiation, which makes it possible to perform it repeatedly. Doctors have no doubts about the accuracy of the results obtained.
Pathologies of the thoracic spine can be diagnosed using other methods. Alternatives to MRI are:
- X-ray;
- CT scan.
These diagnostic methods can detect fractures and metastases (pathologies of bone structures). Pathologies arising in the spinal cord area can be examined using computed tomography. To study hernias, cartilage neoplasms, and circulatory disorders, it is better to use magnetic resonance imaging with contrast.
Computed tomography is used by doctors to detect pathologies of the spinal column and bone tissue injuries. Carrying out MSCT involves exposing the body to x-rays. Multislice computed tomography is performed using special equipment that emits X-rays. MSCT provides an opportunity to study in detail the features of the vertebrae, nerve roots, the condition of the spinal cord, spinal canal, ligaments, discs, and blood vessels. Doctors receive high-resolution images. This makes it possible for the diagnostic method to detect small pathologies in the thoracic region.
X-ray of the spine is the most popular diagnostic method. It is prescribed if the patient complains of discomfort in the back after physical activity.
X-rays show certain pathologies of the spine:
- bone diseases;
- pathological changes in the structure and shape of bones;
- complications after a fracture, dislocation;
- osteoporosis;
- metastases;
- decreased mobility, curvature of joints.
Ultrasound of the spine is prescribed in the presence of the following conditions:
- dizziness;
- poor posture;
- impaired sensitivity of the limbs;
- headache;
- joint pain;
- discomfort in different parts of the back;
- difficulty moving in the spine.
The advantages of this diagnostic are the absence of ionizing radiation and moderate cost.
PET CT is an examination that is carried out through special. apparatus. The operating principle of the device is to use tracer radioactive chemicals. This form of chemical substances are usually accumulated by cancer cells. PET does not provide a detailed picture of the organ, like CT and MRI. The pictures show only the location of the indicator. Positron emission tomography detects the slightest metabolic disturbances.
The diagnostic value of such an examination lies in the possibility of detecting primary cancer cells. Combining PET with CT is considered the most accurate diagnosis. This combination makes it possible to avoid the development of serious pathologies. The only risk is considered to be the possibility of cell damage from a radioactive substance.
Survey results
The results are displayed on the workstation screen as a three-dimensional image. The diagnostician studies the data array (enlarges the required areas, examines the sections, rotates the model), compares them with normal indicators and gives a conclusion. The patient is given an overview image of the thoracic region, a disk with files and a written transcript.
Based on the nature of the shape, color, and contours, the diagnostician determines the presence of anomalies and the degree of their development. Thus, indicating in the transcript the fact of the presence of hyperechoic areas, he means inflammatory processes that are displayed on the screen in lighter shades. Other signs of pathologies:
- the formation of meningioma is clearly manifested in areas of calcification;
- neuroma resembles an hourglass shape;
- dark spots indicate thickening of the spinal cord.
In the transcript, the diagnostician describes only the signs, and the diagnosis is made by a neurologist, neurosurgeon, traumatologist or other specialist. Therefore, you need to ask your doctor questions about the identified diseases.
What happens after the study
After the end of the tomography session, the patient does not need rest or recovery. He can go back to his business while the transcript is being prepared.
As a rule, the conclusion is issued within an hour. In difficult cases, preparing a description may take up to a day.
Based on the transcript, the attending physician recommends contacting:
- to an oncologist – when tumor-like formations are detected;
- to a traumatologist - if a disc or vertebra is displaced;
- to a neurosurgeon - if there are indications for surgical intervention;
- to a vertebrologist – for complex treatment of osteochondrosis;
- to a neurologist for the treatment of neurological diseases - when diagnosing spinal cord pathologies and neurological symptoms.
When is the procedure scheduled?
The procedure is carried out at the request of the attending physician to make an accurate diagnosis or make certain adjustments to the treatment process. MRI is also performed in the preoperative period.
MRI is indicated for diagnosing:
- Encephalomyelitis and multiple sclerosis;
- Neuralgia, osteochondrosis, intervertebral hernia;
- Ankylosing spondylitis;
- Deformities of the spinal column;
- congenital anomalies of the vertebrae;
- problems with the vessels of the spinal cord - stroke, hemorrhages and others;
- spinal injuries, bruises, fractures;
- infectious pathologies;
- neoplasms and metastases;
- inflammatory processes.
Problems in this part of the spine contribute to the appearance of pain in the heart, kidneys, and liver.
Benefits and Alternatives
MRI of the thoracic spine is an informative method, indispensable for obtaining a picture of the condition of soft tissues, cartilage, and brain structures. It is as accurate as possible in diagnosing pathologies of joints, blood vessels, and the nervous system.
Another advantage is absolute safety. There is no ionizing radiation during the study, and electromagnetic pulses are not capable of causing harm.
An alternative to magnetic resonance imaging for examining the spine is computed tomography (CT). Although these methods cannot be called interchangeable. CT is based on the analysis of the passage of X-rays (therefore the degree of safety is lower), it gives a more detailed picture of the condition of hard (bone) tissues and more effectively detects bleeding.
What can be seen in the photographs?
The course of further treatment and even surgical intervention depends on what the image shows. Magnetic resonance imaging is assessed according to various parameters:
- The structure and size of the spinal cord and spinal column. If there are uneven contours, increased or decreased sizes, or incorrect location, the patient is diagnosed with post-traumatic deformities, ischemic changes or transverse myelitis.
- Spinal cord hemorrhages can be seen when examining the subarachnoid space on T2-weighted images.
- If the images show changes in the diameter of the spinal cord, an intramedullary tumor can be diagnosed. In addition, MRI makes it possible to distinguish between neuroma and meningioma.
- From the images, it is possible to diagnose the presence of calcium salt deposits and petrification in the surrounding soft tissues.
- With the help of contrast agents injected into the subarachnoid space, cystic formations can be detected.
- When single foci of increased hyperechogenicity are detected, spondylitis, hemangioma, consequences of syphilis and tuberculosis are diagnosed.
With this diagnostic, you can take pictures of the vertebrae, soft tissues that surround the spinal column, spinal cord, blood vessels and nerve endings. An experienced doctor will see in the images displacement of the vertebrae, the presence of a neoplasm, cysts in the initial stages of development, impaired blood flow, changes in the structure of cartilage tissue and developmental anomalies.
The thoracic spine is often examined to identify diseases of the internal organs - lungs, heart, trachea, vascular system, and so on. Such diagnostics allows us to identify disturbances in the functioning of the heart valves, the structure of the heart muscle, lymph flow and blood flow. If the lungs are examined, the photographs will show the condition and structure of the tissues, the size of the organ and its parts, and the condition of the pleura. MRI results can detect degenerative and inflammatory processes, tumor formations and metastases.
Progress of the procedure
What is the sequence and how is an MRI of the thoracic spine done? The entire procedure is performed in the supine position. The patient should remove their clothing down to their underwear and the patient is dressed in a hospital gown or given a sheet to cover. To reduce the likelihood of patient mobility during the examination, fixing devices are used - belts on the arms and legs.
Depending on the type of MRI machine, the couch slides into a tunnel with magnetic sensors. If an open-type tomograph is installed in the clinic, then its upper and lower parts are moved onto the sternum area.
During diagnostics, the patient and the doctor can communicate using the speaker and microphone built into the tomograph. If the patient before the procedure warned the doctor about some intolerance to closed spaces, he is asked to wear headphones with music or earplugs, since the device makes tapping noises during operation, which can aggravate and provoke an attack of claustrophobia.
The chest scan lasts from 30 minutes to one hour. Many patients find it difficult to remain still for so long, so sedatives and even light general anesthesia can be used. It is also recommended to abstain from food and water for about 6-7 hours.
If a study is planned with the administration of narcotic drugs, the doctor must make sure that there is no drug allergy and find out the tolerance of sedatives. Anesthesia is often used when examining young children (up to 6-7 years old) who cannot lie still for a long time.
Depending on the configuration of the room in which the MRI machine is installed, the child may be offered to watch cartoons. With the doctor's permission, a close relative can stay with the child to reduce the baby's nervousness. In this case, the medical staff gives mom or dad a special lead apron and collar.
How much does a tomography cost?
In different cities of Russia, the cost may vary significantly. The pricing policy depends on the level of the clinic or medical center, the qualifications of the doctor who conducts the diagnosis, and the actual scope of the study. Removing three sections of the spine will cost an order of magnitude more than performing an MRI of only the lumbar or thoracic region. It is worth comparing prices in several medical organizations at once.
| City | Price per procedure in rubles |
| Moscow | 3.000 – 9.000 |
| Saint Petersburg | 5.000 – 10.000 |
| Voronezh | 2.500 – 12.000 |
| Omsk | 4.000 – 8.000 |
| Vologda | 4.500 – 10.850 |
| Samara | 3.000 – 12.100 |
| Saratov | 2.990 – 8.900 |
Magnetic resonance imaging is a quick and affordable way to find the cause of pain in different parts of the spine. The diagnosis is quite new and is carried out only according to the indications of your attending physician. You can also sign up for this procedure yourself at your own expense, which will save a lot of time. Cost may vary in different regions of the country.
Preparing for diagnosis
Many people do not know how to prepare for an MRI of the spine, whether they can eat before the examination, etc. MRI of the entire spine (regardless of which part is planned to be scanned) does not require significant preparation.
It is worth paying attention to some important points in preparation for examining the spine using MRI:
- Before starting the diagnosis, it is necessary to remove from the body all objects that attract the magnet (glasses, jewelry, watches, etc.).
- You should warn your doctor in advance about the presence of bronchial asthma and allergic reactions.
- Before an MRI of the spine, you should tell the doctor that there are metal implants or electronic devices in the body: their presence can cause serious complications, malfunction or distort the results and affect the course of the study itself.
- As for nutrition, you can eat as usual before an MRI. You should take medications as usual unless your doctor asks you to take a temporary break.
How is an MRI examination of the spine performed?
Let's take a closer look at how the MRI procedure of the spine works. First, the patient lies down on a table-couch, after which he is secured using straps to prevent involuntary movements during scanning. Then the table automatically slides into the machine itself.
How long an MRI takes depends on the indications for the procedure, but on average, the study takes about 45 minutes (but can last up to 2 hours). If a person is nervous, the doctor may offer him sedatives. When an MRI is performed on new generation equipment (it is quite spacious), then the fear of a confined space may not arise. An MRI is performed on equipment equipped with a special intercom, so if phenomena such as fear, nausea or breathing problems occur, you just need to say so and the doctor will hear everything via communication.
Important! The patient should be prepared for the fact that there will be quite a lot of noise and knocking inside the device (comparable to hitting metal with a hammer). No need to worry! This is normal operation of the motors and magnetic coil - it is absolutely safe! Sometimes you may be offered sound-isolating headphones before the procedure begins.
What does the diagnostic equipment look like? The standard equipment is a pipe surrounded by magnets. The patient is brought inside on a table that can be easily pulled out. Open type tomographs are a device with a short tunnel that does not completely surround the patient’s body.
Open-type tomographs are designed for examining very obese patients and people suffering from claustrophobia. Some modern open-type MR equipment has holes on the sides, but when using new magnets, this does not affect the quality and accuracy of the resulting image. Some studies are not performed on an open-type MRI machine.
The MRI report in the form of photographs after the procedure is given to the patient in printed or electronic form.
Above, we figured out how an MRI of the spine is done and what its duration is. Now let's figure out what its essence is. The method consists of recording electromagnetic resonance, which is emitted by protons in a created magnetic field. The signals captured by special sensors are processed by complex computer programs to produce a series of images showing a thin section of tissue. The results of MRI of the spine are studied by a radiologist from various angles, which allows you to visually distinguish healthy tissue from those affected and changed by the disease.
Magnetic resonance imaging of the spine can provide a detailed picture of the condition of the spine, making it the most sensitive method of examining the spine known today:
- Allows you to identify diseases in the early stages;
- Not all parts of the spine can be examined, but only the parts of the spine of interest: for example, only the cervical or lumbar;
- Allows you to examine the spinal cord, nerve endings, blood vessels, lymph nodes;
- Magnetic tomography is non-invasive.
- It lasts a long time compared to other procedures, but the patient is not irradiated.
- The patient does not prepare for the procedure - this is not necessary.
- Magnetic resonance diagnostic method is allowed for everyone and has almost no strict contraindications.
- If the diagnosis was carried out without anesthesia, then there is no recovery period.