In 2005, Australian scientists Robin Warren and Barry Marshall refuted the doctrine of the role of poor nutrition, hyperacidity, heredity and chronic stress in the origin of gastritis and peptic ulcers. They were able to prove that often a variety of stomach problems have a specific culprit - the Helicobacter pylori bacterium.
The bacterium easily adapts to an aggressive environment. In some cases, the immune system copes with infection; if not, the doctor diagnoses “gastritis” or “ulcer”. In 1994, WHO even recognized the connection between the bacterium and cancer of the digestive system, so the presence of Helicobacter pylori in the body is a reason to undergo complex therapy. But how to get tested for Helicobacter pylori, where?
Prevalence of Helicobacter pylori
It is believed that almost 70% of the world's population is infected with Helicobacter. Many people carry the bacteria without knowing it and pass it on to healthy people. Helicobacter pylori can indeed hide in the body for years and begin its “subversive” activities in extremely favorable circumstances: with chronic stress and fatigue, exhaustion of the body, decreased immunity, concomitant diseases, unhealthy diet and unhealthy lifestyle.
As for Russia, registered cases of infection in Moscow alone amount to 60% of the total population of the capital. And this is one of the most developed cities in Russia. Doctors say that in different regions the prevalence of the bacterium reaches 70-90%, which is much higher than in Europe or the United States. This high prevalence is explained by the relatively low standard of living of the majority of the population, neglect of hygiene standards and living in unsanitary conditions.
Indications for diagnosis
Doctors recommend regularly taking basic tests in order to detect and treat disorders in a timely manner. But not everyone does this. As a rule, we only go to the hospital if we are already sick. This is what happens with Helicobacter pylori.
It is imperative to turn to diagnostic methods for bacteria in the body as soon as possible if you have the following symptoms:
- Periodic abdominal pain, usually during or after eating. This is due to stagnation and problems with digestion due to low enzyme levels.
- Painful sensations on an empty stomach, which subside when eating. In this case, you can feel how food goes down the esophagus, and if you drink a glass of water, you can feel how the water flows - this sensation appears more clearly and indicates that there are damaged places on the walls.
- The appearance or increase in heartburn. Single heartburn (thrust of gastric juice into the esophagus with irritation of its walls) is a normal variant, but repeated heartburn requires consultation with a doctor and testing.
- Feeling of heaviness even after eating a small amount of food. In this case, the person feels as if the food has stood up and is not digested, “staying in the throat.”
- Frequent nausea and periodic vomiting that is not caused by other reasons (for example, toxicosis in early pregnancy).
- Constant discomfort in the stomach, aching pain, slight heaviness, loss of appetite. If symptoms appear, but then quickly pass, this may indicate the initial stage of the adverse effects of Helicobacter pylori on the mucous membrane.
- Blood and other unusual impurities in the stool. If an adult can determine what hurts, then in the case of children everything is not so simple. That is why you need to pay attention to the baby’s stool, his general condition and movements.
- Frequently recurring diarrhea, constipation, defecation disorders.
- Increased flatulence and rumbling in the stomach.
All of the above signs do not indicate one hundred percent presence of infection in the body. Such symptoms, both in combination and individually, may indicate the presence of a completely different problem, or even be a variant of the norm in a particular case.
How does infection occur and who is tested for Helicobacter pylori?
Helicobacter pylori “lives” in the lower part of the stomach, tolerates the effects of gastric juice well, and is transmitted through saliva. Therefore, infection, as a rule, occurs through close contact or using the same utensils. According to statistics, more than 60% of people living on our planet are infected with Helicobacter, but not everyone has health problems. Why? It all depends on the state of the immune system and the presence of risk factors: stress, bad habits, poor diet. Urgent diagnosis is needed for those who have the following symptoms:
- heaviness in the stomach and heartburn;
- pain in the stomach (especially if it goes away after eating);
- physical aversion to meat food.
Relatives of those diagnosed with helicobacteriosis are also at risk.
Diagnostic methods for Helicobacter pylori
What test should I take for Helicobacter pylori? There are several methods for diagnosing bacteria, which differ in accuracy, the need for preparation, processing time for results, and so on. The first thing the doctor will do is take a medical history. The patient will be asked about symptoms, diet and nutrition, concomitant diseases, medical history, pathologies that close relatives have and can be inherited. Only then will the doctor give a direction for a certain type of analysis.
The presence of harmful bacteria in the body can be detected in various ways. If Helicobacter pylori is suspected, the following tests may be prescribed:
- Laboratory blood test for the presence of antibodies to Helicobacter pylori. If antibodies are detected, it means that the body recognizes the bacterium.
- Stool antigen test. The stool test is aimed at identifying the genetic material of the pathogen in the stool.
- Breath test. A rapid analysis will determine the activity of Helicobacter pylori in the stomach based on the composition of exhaled air.
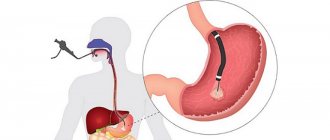
- Gastroscopy for Helicobacter.
- Cytological examination. The method is the most accurate among those listed.
What test should be taken for Helicobacter pylori? To increase the accuracy of diagnosis, it is advisable to take at least two tests. If a bacterium has been identified, then after a course of therapy it is necessary to do a repeat study.
How to get tested for Helicobacter pylori? Preliminary preparation (both the activities themselves and its necessity in principle) depends on the type of research.
Composition of the gastrointestinal microflora
The oral cavity is the entrance gate for microorganisms. Optimal and stable conditions for the life of microorganisms in the oral cavity (temperature, humidity, nutrition, etc.) lead to the fact that the qualitative composition of the microflora is extremely diverse and constant. The total number of microorganisms in 1 ml of saliva is approximately at the same level as in the distal parts of the colon and is 10^7 and 10^8, but differs in species specificity. Streptococci dominate among bacteria, accounting for 30-60%.
The stomach contents of 10% of healthy people are sterile due to the bacteriostatic and bactericidal action of hydrochloric acid and lysozyme, with preserved gastric secretion, does not exceed 10^3 microorganisms in 1 ml of gastric juice and anaerobic microorganisms predominate.
According to Drazer BA et al, 1969, Bauchop N., 1971, Browning et al., 1974 and others, in healthy individuals the following are observed in the gastric mucosa and gastric juice: bacteroids, lactobacilli, enterobacteria, veillonella, streptococci, staphylococci, micrococci , Neisseria, Campylobacter, etc., in total more than 14-22 species of bacteria. The microflora is dominated by staphylococci and streptococci, gram-negative bacteria.
Research in recent years, according to various authors, has shown that in healthy people, Helicobacter pylori is isolated from 6 to 85% and antibodies to Helicobacter are detected in 46%; in some people, candida is detected in the stomach along with Helicobacter. The bulk of bacteria lives in the pyloric (outlet) section of the stomach; in healthy individuals, H. pylori is isolated in 44.4% of cases, streptococci in 55.5%, staphylococci in 61.1%, lactic acid lactobacilli in 50%, 22. 2% fungi of the genus Candida, etc. From biopsy samples of the gastric mucosa of different parts of the stomach, H. pylori was found - in 33.3%, staphylococci - in 61.1%, streptococci and lactobacilli were found in 44.4% of cases and in 27.7% — fungi of the genus Candida and other microorganisms. It seems extremely interesting to combine the detection of microorganisms in the mucous membrane of various parts of the stomach.
This diversity of representatives of the gastric microflora constitutes the microecology of the stomach in a healthy person and its disruption leads to the manifestation of the pathogenic properties of microorganisms belonging to the opportunistic microflora (H. pylori, staphylococci, streptococci, Candida, corynobacteria and others) and found in excess quantities in the stomach, along with other causative factors, may contribute to or support pathological processes in the stomach.
Enzyme immunoassay blood test for antibodies
This type of study is prescribed to determine the presence of antibodies to Helicobacter pylori in the patient’s blood. In medical practice, it is generally accepted that antibodies to certain bacteria and infections appear for a reason, but only in case of infection as a response of the body’s immune system.
An enzyme immunoassay can only determine Helicobacter if one to three weeks or more have passed since the infection. If the infection occurred just a few days ago, the test may give a false negative result, since the body has not yet had time to react properly to the appearance of the bacteria.
A false positive result can be given for two reasons:
- The human factor, i.e. the mistake of a laboratory assistant who mixed up the research material, wrote the conclusion incorrectly, and so on.
- Recent therapy, during which a person was cured of Helicobacter, but antibodies are still present in the blood. A control test can be carried out no earlier than a month after complex therapy, but even in this case you can get a positive result in the absence of bacteria in the body. In some cases (depending on individual characteristics and some other factors), antibodies remain in the blood for life.
How to take a blood test for Helicobacter pylori? Is advance preparation necessary? On the eve of the study, you should avoid eating excessively fatty foods and drinking alcoholic beverages, and avoid nervous and physical stress. Blood is drawn from a vein in the morning, on an empty stomach. The procedure is painless, but different patients tolerate it differently, so after the analysis it is better to drink sweet tea and eat a piece of dark chocolate.
How to determine the presence of Helicobacter in the stomach
It is not possible to see such a tiny organism with a length of only 2-3 microns with the eye, nor is it possible to carry out diagnostics at home.
The patient can only assume the presence of gastritis based on the corresponding symptoms: epigastric pain after eating, heaviness and discomfort in the stomach, heartburn, belching of air or sour, metallic taste in the mouth. These signs of increased acidity very often accompany gastritis associated with a pathogenic microbe.
But it is possible to reliably determine whether the Helicobacter pylori bacterium has settled in the body or not only in the diagnostic department of an outpatient clinic, hospital or laboratory.
There are special methods that make it possible to detect with high reliability both the microbe itself and its metabolic products, as well as the antibodies produced by the body in response to the introduction of the microbe:
- Bacteriological
Detection of a pathogen in smears from a section of the inner wall of the stomach or cultivation of the microorganism on nutrient media.
- Serological
Detection of antibodies in the blood, microbial antigens in the stool.
- Morphological
Detection of N. rulori under a microscope by coating a research sample with special dyes.
- Molecular genetic
Polymerase chain reaction methods.
- Biochemical
Urease test, breath test.
All of the above methods can be classified into two large groups:
- Invasive. Diagnostic methods based on endoscopic examination - FGDS, with taking a biopsy sample. A section of the inner wall of the stomach can then be subjected to cytological, cultural examination, and a urease test.
- Non-invasive. Other methods of detecting infection in which FGDS is not performed.
Where to get a blood test in Moscow
Where can you get tested for Helicobacter pylori in Moscow? First, you can go to a public clinic. A therapist or gastroenterologist, if deemed necessary, will give a referral to a laboratory for testing. Secondly, you can donate blood to identify the bacteria in any private clinic, for example, Invitro or Litech.
In both cases, the results will be ready the next day, however, in private medical centers you can make an additional payment for urgency and receive a specialist’s conclusion within 1-2 hours. The cost of the analysis will be 500-1000 rubles, depending on the pricing policy of the clinic and the urgency of preparing the results. The test can be done free of charge in a public hospital.
Stool antigen test for Helicobacter
The stool test is one of the most patient-friendly methods for diagnosing Helicobacter pylori. Firstly, the study does not require personal presence in the outpatient clinic, and secondly, the material is collected painlessly (non-invasively, that is, without damaging the skin, as when drawing blood), in conditions that are comfortable for the patient. So there is a definite answer to the question of what test to take for Helicobacter pylori, for example, for a child - this is a stool test. This analysis is especially convenient for diagnosing the disease in children, the elderly and seriously ill patients.
However, the effectiveness of stool examination in determining the presence of Helicobacter pylori is insufficient. The number of harmful bacteria, if they exist in the digestive system, decreases when passing through the intestines, and the pathogen is exposed to acids. As a result, the test may give a false negative result. But currently, a special method is used with which specialists can determine even particles of Helicobacter genetic material in feces.
How to take a stool test for Helicobacter pylori? For three days, you must completely stop using suppositories; before collecting the material, you cannot stimulate stool with an enema, castor or other oil. A few days before the analysis, you should exclude from your diet foods rich in fiber, containing a lot of dyes and salts, and you should stop using medications that stimulate intestinal function.
4.1. Laboratory diagnostic methods for Helicobacter pylori infection
Table of contents
To view the text of the book, click on the desired chapter in the table of contents
Next part
4.1.1. Quantitative determination of IgG to H. Pylori using immunoenzyme BPT ImmunoComb
Previous part
Chapter 4. Description of medical technology
Appearance
To select a treatment option, timely and reliable diagnosis of H. Pylori is necessary.
All methods for diagnosing H. Pylori currently used can be divided into direct and indirect (indirect). Into invasive and non-invasive [5, 7]. Invasive methods require a biopsy of the gastric mucosa during endoscopic examination, non-invasive methods do not require a biopsy. Direct methods allow direct detection of H. Pylori. Indirect methods record not the bacterium itself, but the consequences of its persistence in the body.
Most direct methods are based on invasive methods of collecting material. Direct diagnosis of H. Pylori infection is a rather labor-intensive and time-delayed process [13].
After the adoption of the Maastricht Consensus [14], the concept of “testing and endoscopy” existed for several years in European countries [15]. The latter was that upon initial treatment the patient was tested for the presence of H. Pylori infection, and if the results were positive, an endoscopic examination was required. However, the experience of daily practice has shown an unjustified increase in the number of gastroscopy, which was not compensated by positive effects in the form of improved symptoms or an increase in the quality of life of patients. The need for gastroscopy for gastric dyspepsia is dictated by the oncological alertness of doctors. At the same time, it is known that for young patients in the absence of alarming symptoms in the form of weight loss or anemia, in the vast majority of cases, malignant neoplasms of the stomach are not typical. Therefore, for primary patients with peptic ulcer disease, the concept of “test and treat”, adopted at the Maastricht Consensus II in 2000, began to be used as a mandatory concept [10, 16-19]. Health authorities in many countries recommend the same approach for the management of primary young patients. Age limits in recommendations vary depending on the incidence of gastric cancer in a particular population (Table 1). The age threshold is 45 - 55 years [20-26].
Table 1. Threshold age when using the “test and treat” concept
| Organization | Threshold age, years |
| British Gastroenterological Society | < 55 |
| European Society of Primary Care in Gastroenterology | < 45 |
| European H. Pylori Study Group | < 45 |
| American Gastroenterological Association | < 45 |
| Leadership of the Scottish Interuniversity Network | < 55 |
In accordance with the developed concept of the Maastricht Consensus II, the European and Russian groups adopted diagnostic algorithms that determine the primary diagnosis of H. Pylori infections using non-invasive methods: serological, respiratory, PCR in feces and saliva.
In Russia, serological tests based on latex agglutination and the sandwich method are registered for the rapid diagnosis of H.Pylori: FastRead H.Pylori® (CQI-biomed) and Pyloriset® Dry (Orion Diagnostica). The advantage of these techniques is the ease of their implementation and the speed of the results obtained. The disadvantages include a low degree of sensitivity and specificity, as well as the impossibility of quantitative determination of antibodies to H. Pylori, which does not allow their use to monitor eradication.
Among non-invasive methods for diagnosing H. Pylori, the serological enzyme immunoassay is the most common abroad: IgG and IgM antibodies to H. Pylori are determined in the patient’s blood [27-32]. These tests are optimal for epidemiological studies and screening. Such studies are carried out in all Western countries. An example is a survey conducted in Italy using ELISA tests of 1010 donors, in 298 of whom IgG antibodies to H. Pylori were determined [23]. During subsequent gastroscopy, 70 (23.5%) people from the IgG seropositive group were diagnosed with peptic ulcers, 41 (13.8%) with erosive duodenitis, and 2 (0.7%) with stomach cancer. Unfortunately, similar planned studies are not carried out in Russia to identify whether the population is infected with H. Pylori, although screening aimed at detecting antibodies to H. Pylori helps to identify people with gastroduodeal pathology. Timely diagnosis and subsequent adequate therapy help prevent relapses of the disease and exclude H. Pylori infection in large groups of the population.
Until recently, serological tests were considered only from the standpoint of detecting H. Pylori in patients before treatment. Indeed, there were limitations that made it difficult to monitor the effectiveness of H. pylori eradication with their help. The latter is due to the fact that the initial value of the concentration of specific antibodies to H. Pylori in the blood serum of patients, established by standard ELISA tests, varies within significant limits, and its decrease after eradication of the bacterium is nonlinear. The modern generation of ELISA tests, thanks to the improvement of antigen sorption technology and modification of this method, makes it possible to quantitatively assess the degree of H. Pylori invasion, as well as the degree of eradication [33-37]. Various authors have proven that a decrease in the titer of specific antibodies to H. Pylori by 40% from the initial level allows us to establish eradication in more than 90% of patients by 3 months after the end of treatment. Seronegativity in all cured patients occurs after 12 months [38].
Table 2 presents literature data on the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the most commonly used serological tests in the world [39].
Table 2. Characteristics of serological tests for detecting HP
| Name of the test system | Sensitivity,% | Specificity,% | PPV | NPV |
| Oxoid Unipath, Latex agglutination | 93 | 83 | 87 | 91 |
| Pyloriset dry Orion, Murex latex | 77 | 100 | 100 | 80 |
| GAP IgG ELISA Bio-Rad, ELISA | 100 | 84 | 90 | 100 |
| ImmunoComb Orzhenix, ELISA | 98,1 | 86 | 100 | 97 |
| Pyloriset EIA-G Orion, Murex | 93 | 90 | 91 | 92 |
| Helisal OneStep, Cortecs Diagnostics | 84,1 | 63,0 | 73,3 | 76,6 |
As can be seen from the presented data, the sensitivity and specificity of ELISA test systems are higher than similar indicators of serological tests based on latex agglutination and the sandwich method.
When choosing diagnostic methods for Helicobacteriosis for this medical technology, the following factors were taken into account:
- sensitivity, specificity and reliability of tests;
- possibility of quantitative determination of antibodies to H. Pylori;
- uneven provision of various institutes, clinics, hospitals and clinics with modern diagnostic equipment and reagents;
- the need to strengthen the diagnostic service of primary health care with modern high-tech, affordable diagnostic methods.
Of those registered in the Russian Federation, the above requirements are met by the immunoenzyme Quick Simple Tests ImmunoComb H.PILORI IGG (Orzhenix), as the most sensitive, specific, allowing for quantitative determination of the titer of IgG antibodies in serum, plasma or whole blood. BPT ImmunoKombne require special qualifications of personnel and additional equipment. The ImmunoComb technique is based on an original modification of an enzyme-linked immunosorbent assay: the teeth of a plastic comb are sensitized with the corresponding antigens or antibodies, the cells of the baths are filled with ready-made conjugate solutions, washing buffers and a dye. During analysis, the comb teeth are brought into contact with the test samples in the first row of the bath, and then sequentially transferred from cell to cell. If the result is positive, dots (colored antigen-antibody complexes) appear on the ridge tooth. The correctness of the analysis is confirmed by the appearance of a control spot on the tooth. Recording of results - visual (to quantify the results, compare the color intensity of the points in the experiment with the standard color scale included in the kit) or automatic using the CombScan device. The kit allows you to conduct from 1 to 36 analyses, analysis time - 66 minutes, shelf life of the kits 9 months.
Immunocomb test systems are certified CE 0459 and are widely used in more than one hundred countries around the world. ImmunoComb tests meet all quality standards established by Directive 98/79/EC of the European Parliament and of the Council for in-vitro diagnostics.
The production of ImmunoComb test systems has a GMP Certificate and complies with WHO standards. The quality of the tests is confirmed by international standards SI ISO 9001:1994, and ISO 13485:1996 and European standards EN 928:2001, EN 928:1996, EN 980:1997, EN 13612:2002, EN 13640:2002, EN 13641:2002, EN 46001:1996
As reliable, highly sensitive and specific tests, ImmunoComb is selected for the programs of WHO, UNESCO, and the Red Cross. Tested and approved by the P. Ehrlich Institute (Germany), the A. Fournier Institute (France), AFSSAPS, GISC named after. Tarasevich.
Currently, BPT ImmunoComb is completed in Russia by the joint venture ZAO Biograd (St. Petersburg) from reagents produced by Orzhenix.
In 1997, at GISC named after. L.A. Tarasevich, during State tests for the purpose of registration of the Immunoenzyme BPT ImmunoComb H.PILORI IGG company Orzheniks, a comparative analysis of the proposed method with the reference ELISA test system was carried out (Registration Certificate MZMPR No. 97/316). The comparison was carried out on 30 human sera from adults and children with pathology of the digestive tract and healthy people or patients with damage to other organs. To analyze the data obtained, a contingency table was compiled for two signs: the first sign is the detection of IgG antibodies to H. Pylori in sera using the Orzhenix method and the second sign is the detection of these antibodies using the Bio-Rad method. Four sera were discarded because could not be assessed using the reference method. The data are presented in Table 3 [40].
Table 3. Relationship between detection of antibodies to H. Pylori using two methods
| Bio-Rad | Positive | Negative | Sum |
| Orzhenix | |||
| Positive | 19 | 2 | 21 |
| Negative | 0 | 5 | 5 |
| Sum | 19 | 7 | 26 |
l1 = 21, m1 = 19, n = 26
l2 = 5, m2 = 7
Statistical processing of the data showed a relatively large value = 16.8, indicating that the features are strongly associated with each other. We also note that the correlation coefficient in this case turns out to be equal to 0.8, and this also indicates the presence of a strong connection between the two characteristics under consideration.
Thus, based on the data of the experiment, we can conclude that the compared methods are approximately equivalent.
Clinical trials were carried out in the gastroenterology clinic of Children's Clinical Hospital No. 7 in Moscow.
A total of 95 sera were examined.
At the children's hospital, 41 sera from children with various gastropathologies and 18 from healthy children and children with other diagnoses not related to disorders of the gastrointestinal tract were studied. In parallel with the serological method, based on the use of the ImmunoComb ImmunoComb H.PILORI IGG diagnostic kit, the diagnosis of patients was established using a combination of clinical diagnostic methods: endoscopic examination, fluoroscopy, etc. When comparing data from clinical diagnostics and serological research, the following figures were obtained: in children suffering from various forms of gastritis, gastroduodenitis, peptic ulcer and polyposis, an increased level of IgG antibodies to H. pylori was detected in 24 cases, which was 58.5%. When examining adult patients (a total of 36 patients in the group), a coincidence of positive results of serological analysis and clinical diagnosis was found in 97.2% of cases; in five patients, the data of the serological study were confirmed by the histological method (in preparations of biopsy specimens of the antrum and body of the stomach, stained with Giemsa), the cytological method (in smears of biopsy specimens, stained with Giemsa) and the urease method using the Denol test. A positive result of a serological test in such a group of patients is natural.
A parallel determination of the sensitivity and specificity of drugs from Orzhenix and Bio-Rad on 30 sera revealed similar results:
- sensitivity of the ImmunoComb test system from Orzhenix – 85%,
- The sensitivity of the Bio-Rad test system is 80%.
If we take the data obtained using the Bio-Rad reference drug as a starting point, then the sensitivity of the ImmunoComb H.PILORI IGG test is 100%, and the specificity is 71% (see Table 3) [40].
With comparable characteristics of the compared tests, in the conclusion of the GISC named after. Tarasevich [40] noted that ImmunoComb tests do not require additional equipment, allow you to obtain the analysis result in 66 minutes and document it, and make individual testing available, along with group testing. The presence of internal control in ImmunoComb tests ensures error-free analysis and maximum reliability of the result.
ImmunoComb is an original modification of the Enzyme Immunoassay - the only Enzyme ImmunoQuick Simple Tests. Unlike other BPT and rapid tests, the sensitivity and specificity of ImmunoComb reaches, and in some cases exceeds, the characteristics of classical ELISA tests, which require expensive equipment, special premises and personnel training. Equipping the primary medical care diagnostic service with the BPT ImmunoComb H.PILORI IGG will allow for a timely and reliable diagnosis and the prescription of adequate drug therapy.
Where to get a stool test for Helicobacter pylori
In Moscow, you can do a stool test to detect Helicobacter in both private medical centers and public clinics. Where to get a stool test (Helicobacter pylori) in the capital if you choose a private clinic? K, MC in Maryino, “Capital Medical Clinic”, Clinic “Capital”, “Family MC”, “Paracelsus”, “Good Doctor”, “Medical On Group”, “Clinic of Expert Medical Technologies”, “ABC Medicine”, “ Prima Medica", "Edem", St. Andrew's Hospitals, "K+31" and so on.
A gastroenterologist at the clinic will tell you how to get tested for Helicobacter pylori. You can get a consultation in any private clinic, but for reasons of economy it is better, of course, to get tested in any state clinic - the method is not innovative, so you don’t need special equipment, and there are qualified doctors in district clinics.
As for the cost, the study will cost 500-4000 rubles. The most expensive clinics: “Stolitsa” on Letchika Babushkina, MC on Botkinsky, “Stolitsa” on Arbat. The cheapest places are at ABC Medicine, Doctor Ozone, and Good Doctor.
How to get tested for Helicobacter pylori? Change your diet a little a few days before the test, give up alcohol and some medications. The material must be collected in a clean container; special medical kits for stool analysis can be purchased at pharmacies.
When to get tested after Helicobacter pylori treatment? A repeat study can be carried out 3 weeks after the end of the course of therapy. The attending physician will give specific recommendations.
13C/14C urease breath test
UDT is also based on the detection of urease activity of NR. In the presence of NR, hydrolysis of a urea solution taken orally, labeled with a carbon isotope (13C or 14C), occurs. Carbon dioxide (13CO2 or 14CO2) enters the blood and is eventually released through the lungs in the exhaled air. Air samples are taken initially and after a certain time (when using 13C-urea - 30 minutes) after taking the test solution. The increase in labeled CO2 is expressed as delta over baseline (DOB). Typically, DOB >2.0‰ is used as a criterion for the presence of HP infection. The DOB value has been shown to positively correlate with the bacterial load of HP [30]. The sensitivity of 13C-UDT is 96%, specificity is 93% [31].
Initially, UDT was developed using urea labeled with the weakly radioactive isotope 14C, but now it has almost completely been replaced by a test with urea labeled with the stable non-radioactive isotope 13C [31]. 13C-UDT is preferred over 14C-UDT because it avoids even minimal exposure to radiation. However, the lower cost of the test and equipment makes 14C-UDT popular in developing countries. The diagnostic accuracy of 13C-UDT and 14C-UDT is no different, and both tests can be considered the “gold standard” among non-invasive methods for diagnosing HP [32]. False-positive results are rare, but can be observed after performing an endoscopy with a biopsy immediately before the test, in patients who have undergone gastrectomy, and also with a significant decrease in gastric secretion.
UDT is also based on the detection of urease activity of NR. In the presence of NR, hydrolysis of a urea solution taken orally, labeled with a carbon isotope (13C or 14C), occurs.
A small number of false negative results may be due to violations of the methodology for taking and storing exhaled air samples, physical activity the day before and during the test. As with most other tests, a reliable UDT result can be obtained after 2 weeks of PPI discontinuation and no earlier than 4 weeks after stopping antibiotics and bismuth preparations. The Maastricht V consensus ranks urea-labeled UDT as the best method for diagnosing HP with high sensitivity and specificity and excellent performance both for the initial diagnosis of infection and for assessing the effectiveness of eradication [10].
In Russia, a breath test with unlabeled urea (“Helic-test”) has become widespread. The results of an open multicenter study of the effectiveness of breath tests demonstrated its insufficient sensitivity (78%) and low specificity (62%) [33]. The authors of another Helic-test study noted that the low specificity of NH3-urease tests and, as a consequence, the high frequency of false-positive results do not allow their use for the primary diagnosis of infection and monitoring the effectiveness of HP eradication [34].
Breathing urease Helic test
Breath analysis is based on the fact that the bacterium produces special enzymes that can be detected when exhaled. How to get tested for Helicobacter pylori? The patient is asked to breathe through a tube located deep in the mouth. From time to time, the doctor reminds you to swallow saliva so as not to spoil the test results. Typically, two samples of exhaled air are taken.
The main advantages of such a test are its high efficiency, relative safety of the study and convenience for the patient. The test time does not exceed 40 minutes.
General information about H. pylori testing methods
There are several methods for detecting H. pylori. Direct methods allow direct identification of the microorganism itself. Most direct methods require a sample of mucosal tissue (biopsy) and/or stomach and duodenal contents (aspirate), which are usually obtained during an endoscopic examination. Thus, direct research methods are usually invasive. In contrast, indirect methods do not detect the microorganism itself, but indirect signs of infection, for example, specific antibodies in the blood serum (serological tests) or the content of a labeled carbon atom in the exhaled air (breath urease test). Since indirect tests do not require endoscopic examination, they are called non-invasive. Both direct and indirect tests for H. pylori have their advantages and disadvantages. To accurately diagnose helicobacteriosis, several tests are required. In this regard, a comprehensive analysis that includes all the necessary tests for H. pylori is especially convenient for the doctor and the patient.
One of the most sensitive methods for detecting H. pylori is real-time polymerase chain reaction (RT-PCR). RT-PCR is a molecular diagnostic method that allows one to detect fragments of genetic material (DNA) of an infectious agent in biological material (for example, in a tissue sample). Since the analysis is based on the detection of genetic material, RT-PCR allows one to detect the presence of any forms of H. pylori (not only active spiral forms, but also inactive cocci, non-cultivable ones), as a result of which the study is characterized by very high sensitivity, exceeding the sensitivity of the bacteriological culture method.
Theoretically, the presence of 1 DNA molecule is sufficient to carry out RT-PCR. In practice, the concentration of the pathogen in the sample should be about 10-100 CFU/ml. This high sensitivity of the test means that a negative test result allows H. pylori to be excluded as the cause of the disease. This is of fundamental importance in the differential diagnosis of NSAID-associated, stress and ischemic gastritis and ulcers.
It should be noted that despite the very high sensitivity of the test (85-98%), false negative results are still possible. For example, a false negative result can be obtained if the bacterial load is very low (for example, while taking certain antibiotics). Diagnostic errors can be avoided by combining this direct test with serological tests.
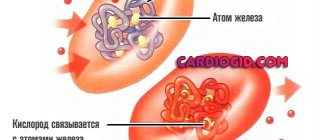
H. pylori infection is accompanied by a significant increase in immunoglobulins of the IgG and IgA classes in the blood serum
H. pylori infection is accompanied by a significant increase in IgG and IgA class immunoglobulins in the blood serum. These immunoglobulins (antibodies) are detected in the blood using indirect tests. IgG is found in 95-100% of cases of helicobacteriosis, and IgA in 68-80%. The study allows you to determine the antibody titer, that is, it is quantitative. Typically, high antibody titers are more characteristic of an active, ongoing infection. It should be noted, however, that there is no clear correlation between the antibody titer and the severity of the infection.
Serological tests, like the RT-PCR method, have some limitations. Thus, the result of the analysis depends on the characteristics of the patient’s immune response. The immune response of patients taking cytostatic drugs and the elderly is characterized by a reduced production of specific antibodies (any, including to H. pylori). For this reason, in order to avoid diagnostic errors, it is advisable to supplement serological tests with direct tests. This feature was taken into account when compiling a comprehensive analysis for H. pylori.
Thus, a comprehensive analysis for H. pylori is a combination of necessary and sufficient tests to identify this microorganism. The comprehensive analysis is not intended to monitor treatment. The result of both RT-PCR and the study of IgG and IgA immunoglobulins will remain positive even in the case of complete eradication of H. pylori. The false positive result of RT-PCR in this case is due to the ability of this method to detect the DNA of any, even destroyed microorganisms, while the false positive result of serological tests is due to the peculiarities of the dynamics of the immune response.
Tips for preparing for the test
How to get tested for Helicobacter pylori? Preparation for a breath test requires serious preparation. First, you should slightly modify your diet on the eve of the study:
- exclude legumes, brown bread, cabbage and apples (foods that can cause increased gas formation in the digestive tract);
- give up alcoholic beverages and, on the day of the study, chew gum and cigarettes;
- do not drink liquid an hour before the test;
- Only an early and light dinner is allowed; after 10 pm on the day before the test you can no longer eat;
- in the morning before the test, you need to brush your teeth and rinse your mouth with clean water; you should not use mouth fresheners or rinses;
- The attending physician must be informed about all medications that the patient took 2-3 days before the test.
What does a histological examination of a biopsy show?
With inflammation, the infiltration of leukocytes – pus – into the cavity sharply increases. On the surface of the epithelium, small follicles and lymphoid aggregates are distinguished. At high magnification, Helicobacter pylori cells are visible both in the mucus and on the section in the biopsy sample. Physicians are assisted in observation by standard hematoxylin and eosin staining. However, this does not identify the bacterium.
Worfin-Sterry dyes
In this case, Worfin-Sterry or Gims dyes are used. In some situations, triple formulations help. A Ghent dye made from uranyl nitrate is used, and in combination with a microwave oven, doctors inject lead nitrate. Heating reduces the time to acquire the desired shade to 28 minutes. It has been proven that this gap is reduced by at least three times.
The expected results are obtained with Ghent and El-Tsimati dyes. Dif-Quick is an inexpensive alternative. In doubtful situations, when a diagnosis is being checked, it is recommended to use El-Tsimati dye. This is a way to detect Helicobacter on the epithelium of the duodenum. Incorrect selection of dyes often leads to negative diagnoses.
Experts advise taking 2 biopsy samples from the antrum and the same number from the body of the stomach. Microorganisms are predominantly concentrated in the surface layer. False negative results occur in several cases:
- Areas of metaplasia.
- Atrophied areas of the mucosa.
- Taking proton pump inhibitors or antibiotics.