General information
Clostridiosis (clostridium spp) is an infectious disease with an acute course. It is caused by clostridia - gram-positive anaerobic bacteria that can produce endospores. Thanks to this, they are well preserved in the external environment. It is the varieties of these bacteria that produce the most toxic poisons: botulinum toxin, tetanospasmin, ε-toxin. They cause very serious diseases: tetanus , botulism , gas gangrene , etc. But most often they are affected by the bacterium Clostridium difficile. Normally, these bacteria are part of the microflora of the gastrointestinal tract and genital tract in women. Clostridium difficile is a representative of normal microflora; it causes colitis and enterocolitis if it multiplies too actively. The toxin produced by the bacterium clostridium perfringens can cause foodborne illness, and the toxin produced by clostridium botulinum causes botulism.
Features of diseases caused by clostridia
The main distinguishing feature of all clostridioses is the clear expression of necrotic and toxic factors that prevail over inflammatory processes. Therefore, the characteristic symptoms of diseases of this group are swelling, necrotic lesions and gas formation in the tissues.
Pseudomembranous colitis
The appearance of pseudomembranous colitis, the causative agent of which is Cl. difficile is often recorded in hospital settings or after undergoing a long course of antibiotic therapy. This is explained by the fact that clostridia are immune to most antimicrobial drugs and disinfectants that have a detrimental effect on other microorganisms. Against the background of a decrease in the amount of healthy microflora, enterocolitis caused by Clostridium difficile develops. They manifest themselves with the following symptoms:
- severe diarrhea with mucus in the stool;
- increased body temperature;
- nausea and vomiting;
- abdominal pain;
- increased fatigue;
- headache.
The mild form of the disease goes away immediately after stopping the antibiotic. When transitioning to a severe form, the following occurs:
- dehydration;
- circulatory disorders;
- the appearance of blood in the stool;
- convulsions;
- decrease in the total volume of urine excreted.
A complication of pseudomembranous colitis is intestinal rupture followed by peritonitis, leading to death.
The peculiarity of the pathology is relapses, which appear 3-27 days after recovery.
Botulism
The most dangerous infection is botulism, since botulinum toxins produced by Cl. botulinum, stronger than other clostridia. Getting into the human digestive tract with food, these poisons are quickly absorbed into the blood, causing severe damage to the nervous system, ending without treatment in paralysis of the respiratory center and death.
Tetanus
Cl. tetani produces tetanus toxin, which causes tonic muscle contractions. In addition, against the background of the underlying disease, clostridium provokes ruptures of ligaments, tendons and muscles, bone fractures, pulmonary edema and pneumonia.
A feature of tetanus clostridiosis in infants is the ability of the bacillus to secrete exotoxins in the digestive tract and provoke clinical signs of botulism. In a child’s body, after a year, the microorganism loses this property.
Gas gangrene
An infection that affects the skin. Very often develops after injuries, wounds, amputations. Gangrene is an affected, dead area of skin that gradually invades healthy areas.
Clostridia of gas gangrene include Clostridium perfringens, Cl. novyi, Cl. septicum and some other strains of bacteria. The disease is characterized by a high rate of development, with clinical signs appearing already 6 hours after infection. These include:
- fever;
- blue discoloration of the skin in the area of penetration of bacilli;
- pain and swelling of the wound edges;
- release of gas bubbles with an unpleasant putrid odor from the wound when pressure is applied;
- crepitus of the affected area upon palpation.
Doctors identify four specific symptoms of gas gangrene:
- Melnikov's symptom. A ligature applied to an infected limb, after a quarter of an hour, strongly digs into the skin due to the rapid increase in tissue volume.
- Spatula sign. When applying light blows with a metal spatula, a tympanic crunching sound is heard.
- Champagne cork symptom. Removing the tampon from the wound is accompanied by a popping sound.
- Krause's sign. Accumulations of gas bubbles between muscle fibers have a “herringbone” shape on an x-ray.
Pathogenesis
- Clostridium difficile is a gram-positive rod that produces two exotoxins: enterotoxin A and cytotoxin B. Both of them provoke diarrhea syndrome. Clostridium difficile in the form of spores demonstrates high resistance in the external environment and can survive in the intestines even at high concentrations of a number of antibiotics . Clostridia difficile is the main causative agent of pseudomembranous colitis, a dangerous condition for newborns and young children. In addition, they provoke other enterocolitis and colitis after irrational antibiotic treatment. The pathogen is transmitted by contact. The disease caused by this pathogen develops during or after treatment with broad-spectrum antibiotics. Under the influence of certain antibacterial drugs ( lincomycin , clindamycin , ampicillin , etc.), changes occur in the intestinal microflora and colonies of clostridium difficile appear. They actively reproduce and provoke disease. The disease can also develop as a result of exogenous infection during or immediately after antibacterial treatment. The disease develops immediately after treatment is discontinued or after a few weeks; it can be protracted or become chronic.
- Clostridium perfringens is a gram-positive bacteria, the causative agent of toxic infections and gas gangrene. Clostridium perfringens is a representative of opportunistic microflora; they persist in the external environment for a long time. The bacteria Clostridium perfringens causes foodborne illnesses. And when Clostridium perfringens gets into an open wound, they produce toxins that damage surrounding tissues and create conditions for further spread of infection. C. perfringens type A is the main etiological factor of gas gangrene.
- Clostridium botulinum is an anaerobic bacterium that grows in the absence of oxygen. Produces spores that are widely distributed in soil, water, etc. Bacteria enter food products, grow in them and produce toxins . After consuming contaminated food, mainly canned food, a person becomes infected with botulism.
- Clostridium tetani is a spore-forming, Gram-positive, anaerobic bacterium. It is the causative agent of tetanus. Transmitted by contact. Bacteria produce tetanospasmin , which affects the nervous system and provokes tonic contractions of striated muscles. It is neutralized by antitetanus serum. The bacterium also produces tetanolysin .
Forms and symptoms
Botulism is a dangerous infection that develops as a result of exposure of the human body to botulinum toxin, a waste product of the bacterium Clostridium botulinum. The first clinical signs of the pathology are: severe epigastric pain, paroxysmal headache, loose stools, repeated vomiting, general malaise, fever. Suddenly, vision is impaired, double vision appears, the clarity of objects is lost, and spots float in front of the eyes. Botulism is manifested by aphonia, dysphagia, ophthalmoplegia, paralysis and paresis of the pharyngeal and laryngeal muscles. Patients choke on liquid food, their phonation and articulation are impaired, their voice becomes nasal, nasal, and hoarse. The height of the disease is manifested by unsteadiness of gait, muscle hypotonia, dysuria, pale skin, tachycardia. In the final stage of the disease, symptoms of respiratory dysfunction predominate: shortness of breath, a feeling of constriction or tightness in the chest, suffocation.
Tetanus is an acute infectious disease that develops through contact infection with the tetanus bacillus Clostridium tetani, which is widespread everywhere. The causative agent C.tetani produces a powerful poison - tetanus neurotoxin, which affects the motor cells of the spinal cord and brain. Paralysis of the heart muscle and respiratory center is the cause of death in patients with tetanus. The disease develops mainly in individuals aged 3-7 years. This is due to the high mobility of children and their frequent traumatization. The incidence of tetanus is highest in the southern regions with a developed agricultural sector, especially in the warm season.
Gas gangrene is a specific lesion of deep wound surfaces caused by Clostridium perfringens. A couple of days after receiving a serious injury, symptoms of pathology appear. The wound creates the necessary conditions for the growth and development of clostridia: there is no oxygen, there are dead cells. Bacteria in the outbreak produce toxins, which leads to severe intoxication of the body. The affected tissues swell and die. Symptoms of the pathology are: crepitus that occurs upon palpation of the affected tissue; foul-smelling discharge from a wound; feverish condition.
Gas gangrene
Pseudomembranous colitis is a consequence of antibiotic therapy. The patient develops intestinal dysbiosis with the predominant activity of Clostridium difficile. The microbe colonizes the intestinal mucosa and secretes enterotoxin and cytotoxin. Inflammation of the mucous membrane is accompanied by the formation of “pseudomembranes,” which are fibrinous deposits. In the absence of active therapy for colitis, severe complications develop - perforation of the intestinal wall, peritonitis and death. Typically, this disease occurs in the elderly, cancer patients, and patients after surgery. The pathology has an acute onset. Patients develop fever, flatulence, cramping pain in the abdomen, persistent vomiting, belching, headache and other symptoms of intoxication. They develop anorexia, cachexia, unkemptness, loss of body weight, tenesmus, straining, moral depression, and depression. Immunity decreases sharply and diarrhea occurs. Loose stools contain fibrin deposits and emit a putrid odor.
Antibiotic-associated diarrhea develops in hospital patients who have undergone long-term antibiotic therapy. Clostridia that live in the intestines become resistant to drugs. Pain in the umbilical area quickly spreads throughout the abdomen. The stool becomes more frequent, but the general condition of the patients remains satisfactory. Newborns and babies in the first year of life do not suffer from this pathology, since they receive antibodies against clostridia antigens from their mother's milk.
Necrotic enteritis is inflammation of the intestinal wall with the formation of foci of necrosis, erosions and ulcers. Patients develop fever, chills, dyspepsia, loose stools with bloody foam. Specialists detect hepatosplenomegaly, severe bloating, indicating intestinal paresis. The development of bleeding, thrombosis of arterioles and venules, and perforation of ulcers is possible. Necrotizing enteritis usually develops in weakened individuals, children and the elderly.
Foodborne illness caused by clostridia is manifested by the classic symptoms of food poisoning: fever, diarrhea, dyspepsia, lack of appetite, abdominal pain. Dyspeptic and intoxication syndromes are the basis of this form of pathology. Patients become lethargic and restless. Symptoms last 3-4 days and then subside.
Classification
To date, more than one hundred species of clostridia have been identified. In medicine, their classification is based on several principles. Based on morphology, the following groups are distinguished:
- rods with a round, terminal spore (C. tetani);
- rods with an oval subterminal spore (C. botulinum);
- with a subterminal or centrally located oval spore (causative agents of gas gangrene).
By type of pathological processes:
- enteral clostridioses (C. botulinum, C. perfringens, C. difficile);
- traumatic and post-traumatic (C. tetani, C. perfringens, C. novyi, C. histolyticum, C. septicum);
- generalized infections: septicemia , sepsis .
How to treat clostridiosis?
If clostridia detected in a child’s stool is the cause of his poor health, then treatment must be done immediately. Treatment for each type of clostridiosis will be specific and may include taking the following groups of drugs:
- Antibacterial agents to which the detected species of clostridia are sensitive (Metronidazole, Vancomycin).
- Probiotics and prebiotics to restore intestinal microflora (Linex, Bifidumbacterin, Lactofiltrum, Hilak-Forte).
- Enterosorbents as symptomatic treatment (Smecta, Activated carbon, Enterosgel).
- Administration of solutions to eliminate symptoms of dehydration (saline, glucose).
- Vitamin preparations, especially group B.
- Enzyme preparations (Mezim, Creon, Omez).
It is necessary to treat clostrizia in a timely manner, since children are highly susceptible to the influence of toxins released by these bacteria and have a hard time suffering from such diseases.
If clostridia is detected in a child’s stool, you should consult a doctor to understand whether the threat is real. If yes, then you should start treatment after consultation and diagnosis, and if not, then you just need to continue to observe the rules of personal hygiene to avoid infection with pathogenic types of clostridia.
Causes
Normally, clostridia are present in the intestinal microflora in adults and children. Clostridia in the feces of an adult should not exceed 105 CFU/g. But, if they are activated and, accordingly, multiply too quickly, this leads to a deterioration in well-being and the development of the disease. The activation of these bacteria can be triggered by some external and internal factors:
- Consumption of low-quality food - stitched, low-quality, spoiled products, as well as fast food and other junk food.
- Regular stressful situations.
- Unfavorable environmental conditions.
- Constant lack of sleep, insomnia .
- Weakened immunity .
- Taking antibiotics, hormonal drugs, immunosuppressants.
- Intestinal infections.
- Immaturity of the central nervous system.
- Frequent colds, flu .
- Surgical operations.
Treatment
If a certain amount of clostridia is found in an adult, this is a normal state of balance of the intestinal microbial flora, which does not need to be interfered with at all. That is, no treatment is needed, even prophylactic.
Be sure to read:
List of intestinal antiseptics and their use
Treatment of clostridial infection is necessary only if there is a change in the functioning of the digestive canal and/or a change in the general condition. Therapy involves the use of diet, medications and lifestyle adjustments.
Hygiene and dietary nutrition
Contamination with clostridia occurs easily and unnoticed, so the patient must:
- wash your hands frequently and thoroughly with soap;
- use only an individual set of dishes and household items (comb, toothbrush);
- Minimize direct contact with other people to avoid infecting them.
Dietary nutrition plays an important role in the treatment of any intestinal infection. During the period of severe clinical symptoms, the following products are allowed:
- fermented milk;
- boiled or baked vegetables and fruits;
- porridge with water;
- steamed lean fish and meats.
After restoration of the digestive canal, the patient should adhere to the well-known principles of a healthy diet.
Drug treatment
Any attempts at self-treatment can only do harm. Preventive use of even the most advertised remedy can upset the delicate balance of the intestinal microbial flora. Therefore, only a doctor can make all appointments. In complex therapy the following are used:
- antibiotics with a predominant effect on anaerobic flora (metronidazole);
- infusions of saline and colloid solutions;
- enzymes for faster restoration of digestive processes;
- multivitamin complexes;
- immunomodulators to increase immunological reactivity.
The duration of complex therapy is 7-10 days, in some cases – longer.
Symptoms
Clostridiosis does not have a typical clinical picture. Manifestations depend on which system the pathological process began in. But still, several signs stand out that appear regardless of the type of pathogen:
- Increased body temperature – it can reach 39 degrees.
- The appearance of sharp abdominal pain of a spastic nature. When palpation is performed, the pain becomes more pronounced, the walls of the abdominal cavity become tense.
- Flatulence , bloating.
- Weight loss due to lack of appetite and deterioration in health.
- Diarrhea , blood and parts of food are sometimes detected in liquid stool.
- Nausea, frequent vomiting, sometimes the presence of blood in the vomit.
Clostridiosis difficile develops as pseudomembranous colitis, in more rare cases - diarrheal syndrome or necrotizing enterocolitis.
As a type of pseudomembranous colitis, the disease most often develops in newborns and infants. The disease begins acutely - the body temperature rises, the child spits up, vomits, and diarrhea syndrome develops. Watery stools contain mucus and sometimes blood. Often the child defecates thick mucus with fibrous patches. The stool may also be purulent. The skin takes on a gray-pale color, and a network of veins is visible on the abdomen. Children experience bloating and refuse to eat. Accordingly, babies lose weight. It is possible to develop bleeding in the intestines, which is an extremely life-threatening condition.
The disease is severe in newborns, especially in premature babies. Without proper treatment, death is possible.
Clostridia in the analysis are increased
If the volume of clostridia in tests for dysbacteriosis exceeds normal values, then this indicates increased production of indole and skatole in the body. The reason for this phenomenon may be the consumption of excessive amounts of protein foods . In the body of a healthy person, clostridia themselves are responsible for the processing of protein products, and their metabolic products contribute to intestinal motility and rapid excretion of feces.
But with an increase in the volume of microorganisms, the ingestion of excess amounts of indole and skatole can cause putrefactive dyspepsia .
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
With an increase in the volume of clostridia against the background of dysbacteriosis, a person may be susceptible to necrotic enteritis, antibiotic-associated diarrhea and other diseases that can even cause death.
For this reason, it is important to follow preventive measures.
These include careful adherence to sanitary and hygiene standards, especially keeping food and hands clean, since clostridia are bacteria that grow and develop in the soil.
Tests and diagnostics
To make a diagnosis, a specialist must study the patient’s medical history, paying attention to whether antibiotic therapy was carried out.
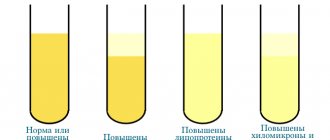
A laboratory test of stool is required to check for the presence of Clostridium difficile and their toxins. If necessary, an endoscopic examination of the large intestine is performed, which reveals characteristic signs - yellowish plaques on the mucosa, a thick layer of overlays, ulcerated areas, which can be important in the process of differential diagnosis. Radiography may be performed.
A blood test is also performed, in which nonspecific changes are noted in the manifest forms of infection.
Symptoms of increased levels of Clostridium difficile
With an increase in the level of clostridia in the intestines, children and adults develop pseudomembranous colitis, which occurs in the form of acute dysbiosis caused by taking antibacterial drugs (lincomycin, tetracycline, amoxicillin, erythromycin, etc.). Sometimes an imbalance of intestinal microflora is provoked by taking immunosuppressants, cytostatics or laxatives.
The patient experiences the following symptoms:
- bloating;
- loose stools;
- impurities of mucus and blood in the stool;
- stomach ache;
- signs of intoxication (weakness, headaches, fever, etc.).
Due to the release of toxins by clostridia, plaque (pseudomembrane) forms on the intestinal walls. Over a long period of time, the waste products of these bacteria can lead to complete erosion of the intestinal wall and the development of peritonitis.
Prevention
To avoid clostridiosis, you must adhere to the following preventive measures:
- Do not take broad-spectrum antibiotics without a doctor’s prescription, especially for long courses. The risk of clostridiosis increases especially strongly when using ampicillin and aminoglycosides (enteral forms).
- It is important to maintain good hygiene.
- It is necessary to properly process food thermally and not eat spoiled or expired foods or canned food.
Which doctor should I contact?
If diarrhea, bloating, vomiting, fever and abdominal pain occur, you should consult a gastroenterologist. After conducting stool tests and determining the type of clostridia, the doctor prescribes treatment. If necessary, the examination of the patient is supplemented by radiography and colonoscopy.
Detection of clostridia in stool does not always indicate the development of the disease. A certain type of such microorganisms belongs to opportunistic microflora and at a certain level does not cause the development of any signs of digestive disorders. If there is a significant increase in indicators or pathogenic varieties of clostridia are detected, treatment is prescribed aimed at suppressing the growth of these microorganisms and restoring normal intestinal microflora.
Diet
Diet for intestinal dysbiosis
- Efficacy: therapeutic effect after 15-21 days
- Time frame: 1-2 months
- Cost of food: 1280-1360 rubles per week
If an adult or child is undergoing treatment for an illness caused by clostridia, he must adhere to a special diet.
It is important to exclude the following foods from your diet:
- Those that have a laxative effect: legumes, cabbage, beets, dried apricots, prunes, etc.
- I love any kind of preservation.
- Pickled and spicy foods.
- Fast food, any sausages.
- Mushrooms, onions, garlic, radishes, radishes.
- Fried, fatty foods.
- Sweets, soda.
- Alcoholic drinks.
The following products and dishes must be included in the menu:
- Those that have a binding effect: raisin decoction, rice, bananas, etc.
- Products with lactic acid bacteria: yogurt, kefir.
The diet can be composed of the following products:
- Meat and fish of lean varieties.
- Boiled and baked vegetables, herbs.
- Non-acidic berries and fruits.
- Eggs.
- Cereals.
- Vegetable oils.
You need to eat in small portions and often. Avoid very hot and very cold foods.
Clostridium perfringens
These clostridia produce a toxin (poison). The toxin is very persistent and persists even at temperatures of 100 degrees Celsius. Clostridium perfringens causes severe poisoning (gastroenteritis).
How is Clostridium perfringens transmitted?
The infection is most often found in meat and poultry. Infection of people most often occurs due to non-compliance with the technology for preparing and storing large quantities of food.
Clostridia strains that contaminate meat may persist during primary processing. During repeated processing, their spores are formed. During an outbreak of acute infection, up to 70% of those in contact with the infection may become ill.
Symptoms
Symptoms of food poisoning appear 12-24 hours after the contaminated food is eaten.
There are Clostridia perfringens types A and C.
When infected with Clostridium perfringens type A, moderate gastroenteritis develops with the following symptoms:
- stomach ache,
- watery diarrhea.
When infected with Clostridium perfringens type C, necrotizing enteritis with severe symptoms may develop:
- sharp pain in the abdomen,
- bloody diarrhea,
- nausea,
- shock,
- peritonitis.
Treatment
Type A disease is treated with antibiotics.
In case of development of necrotizing gastroenteritis, urgent surgical intervention is necessary.
Prevention
Prevention of the disease is compliance with sanitary requirements when storing meat, especially in catering establishments.
Can Clostridium perfringens be cured?
In most cases, the disease is cured completely
It is important to start treatment as early as possible to prevent the development of necrosis
List of sources
- Atlas of medical microbiology, virology and immunology: Textbook for students of medical universities / Ed. A. A. Vorobyova, A. S. Bykova. - M.: Medical Information Agency, 2003. - P. 66. - 236 p. — ISBN 5-89481-136-8.
- Kovaleva E.P., Semina N.A., Semenenko T.A., Galkin V.V. Handbook of Hospital Epidemiologists. – M.: Chrysostom, 1999. – P. 136–139.
- Medical microbiology./ Ed. V.I. Pokrovsky, O.K. Pozdeev. – M: GEOTAR MEDICINE, 1999.
- Uchaikin V.F., Nisevich N.I., Shamsheva O.V.. Infectious diseases in children: textbook. - M.; GEOTAR-Medka, 2011.-688 p.. 2011
Preparing for analysis
The patient collects feces at home. It is advisable to examine stool only in the presence of loose stools (10–15 ml of watery stool); it is not advisable to examine samples of formed stool.
A stool test for clostridia and toxins is prescribed by a gastroenterologist or therapist if pseudomembranous colitis is suspected, which is provoked by taking medications. You need to undergo an examination if you have negative symptoms: intoxication, diarrhea, blood in the stool, acute pain in the abdomen. In order for the results of the analysis for clostridia and toxins to be indicative, you need to avoid taking medications and laxatives 24 hours before the procedure.
How to prepare to submit the material
Before taking the test, you don’t have to adhere to a strict diet, change your diet, or do some preparation.
The day before the examination for toxins and the presence of clostridia, the use of medications administered through the anus is excluded, and medications that affect the contraction of the intestinal walls are discontinued:
- sympathomimetic agents;
- enzymatic preparations.
On the day of the clostridium test, the stool is placed in a sterile plastic container. A sample that has fallen into the toilet and had contact with water is not suitable. Using a plastic spatula, 5-6 parts of feces are selected and transferred to a container issued by the hospital for collecting biomaterial. The sample should not contain urine, blood, or secretions. Take the stool to the laboratory within 8-10 hours; the sample must be placed in the cold. Optimal storage temperature: 3-7 °C.
What slows down and accelerates the growth and reproduction of bacteria
Among the external and internal influences that provoke excessive growth of clostridia, the following are known:
- unbalanced diet (especially with excess carbohydrates);
- repeated episodes of infectious diseases that weaken the immune system;
- chronic diseases of the digestive canal, which cause fecal retention.
Everything that is included in the concept of a healthy lifestyle slows down the growth of clostridia and their predominance over normal microflora:
- proper nutrition;
- absence of chronic pathology or its stable remission;
- regular bowel movements.
Self-infection is also possible, that is, the introduction of clostridia from the surface of mucous membranes due to poor personal hygiene.
Independent laboratory Chance BioGeneral clinical analysis of stool
(stercobilin, bilirubin, feed digestibility, general microscopy, without helminth eggs and protozoa)
With the help of scatological research it is possible to identify:
- problems associated with impaired digestion of feed components;
- problems associated with impaired intake of proteins and fat-soluble vitamins
- excessive growth of opportunistic microflora, leading to fermentation processes in the intestines;
- the presence of an inflammatory process
Due to the high risk of false-positive reactions and, as a result, erroneous interpretation of the results, it was decided to exclude the “occult blood” test method from the “General stool analysis”.
Since for an objective assessment of feed digestibility it is necessary to follow the usual diet for a given animal (nature of food, frequency of feeding), it is generally impossible to avoid the presence of substances in the feces that affect the result of the occult blood test.
Sources of falsely false occult blood results include feeding raw and undercooked meats and some commercial foods (containing food colorings and vitamin supplements), so stool occult blood testing should be performed as a separate test.
Due to the high risk of false-positive reactions and, as a result, erroneous interpretation of the results, it was decided to exclude the “occult blood” test method from the “General stool analysis”.
Since for an objective assessment of feed digestibility it is necessary to follow the usual diet for a given animal (nature of food, frequency of feeding), it is generally impossible to avoid the presence of substances in the feces that affect the result of the occult blood test. Sources of erroneously false occult blood results include: feeding raw and undercooked meats and some commercial foods (containing food colorings and vitamin supplements)
Marina Dzhem: To obtain a reliable result, we ask you to follow the rules for preparing an animal for testing for “occult blood”
Collection, storage, delivery of material: Stool is collected in a clean, dry, disposable plastic container (stool bottle with a spatula with a red or blue lid). Stool must be delivered to the laboratory no later than 12 hours after defecation, stored in the refrigerator until examination .
The study of fecal digestibility of herbivores in this format does not provide useful clinical information.
Contraindications for taking the test: Taking laxatives, including petroleum jelly, Taking activated charcoal, After enemas and x-ray examination of the stomach and intestines)
Table. Clinical and diagnostic significance of elements found in feces (according to: Morozova V.T., Mironova I.I., Martishevskaya R.L.).
| Elements of feces | Pathogenesis | Clinical situation |
| Muscle fibers Undigested | Achlorhydria, achylia, accelerated evacuation, hyperchlorhydria | Chronic atrophic gastritis, malignant tumor, peptic ulcer |
| Overcooked | Expedited evacuation | Pancreatic insufficiency |
| StarchUndigested (a lot)In the stage of digestion | Normal and increased gastric secretion, accelerated evacuation, fermentative dyspepsia-chlorhydria | Chronic gastritis, enteritis, colitis, pancreatic insufficiency |
| Digestible fiber (detection) | AhiliaHypersecretion | Insufficiency of gastric digestion |
| Indigestible fiber (large amounts) | Dysbacteriosis, dysbiosis of the thick gastrointestinal tract | Persistent or recurrent dyspeptic disorders |
| Fat: Neutral (increased) | Lipase deficiency | Acute and chronic pancreatitis, obstructive jaundice, infectious hepatitis, enteritis, colitis, gastroenteritis |
| Fatty acid salts (increased) | Acholia due to obstruction or intrahepatic cholestasis | |
| Slime (enlarged) | Inflammation of the mucous membrane | Enteritis, enterocolitis, gastroenteritis |
Other diseases
Cl.perfringeus is a dangerous pathogen that enters the body through the digestive system. It leads to a structural change in cells. The situation is dangerous and can lead to necrosis. Gastroenterocolitis is severe. It most often develops in children with weak immunity and the presence of other diseases of the gastrointestinal tract. Pathology is diagnosed only if certain groups of bacteria have been identified in the analysis.
The symptoms are specific and always appear quite clearly. Clostridiosis is characterized by the presence of the following manifestations:
- Constant presence of nausea and vomiting.
- The baby feels unwell due to severe pain in the tummy.
- In addition, blood, pus or mucus can be observed in the stool.
To completely eliminate the disease, antibiotics must be used. Disintoxicating colloidal solutions will help improve the condition of a small patient.
Cl.deficile is a pathogen that poses a great danger to young children. Against this background, pseudomembranous colitis develops. Only a long course of antibacterial drugs can eliminate it.
Prevention of clostridiosis - compliance with the rules and regulations of personal hygiene
The clinical picture is in many ways similar to the case described above. The disease has severe symptoms and requires a long, properly selected course of treatment. Clostridiosis is diagnosed based on medical history and confirmed by a number of laboratory tests. To eliminate the disease, you will also need to take a long course of broad-spectrum antibiotics.
According to Dr. Komarovsky, a child with such a diagnosis should be given as little medication as possible. A pediatrician should monitor changes in the young patient's condition. To eliminate dysbacteriosis, it will be quite enough to adjust the diet and normalize the baby’s sleep pattern. Medicines only worsen the functioning of the immune system, so the disease continues for a long period.
Clostridiosis is a dangerous disease. It can negatively affect the health of a small child. Against this background, metabolism is disrupted. If you have symptoms of the disease, you should immediately visit your doctor's office. He will be able to assess the condition of a small patient and prevent the pathology from becoming severe. Parents must ensure strict compliance with all instructions of the attending physician.