What are monocytes and what are they responsible for?
Monocytes are part of white blood cells and the general immune system. Macrophages have the ability to absorb harmful bacteria of a sufficiently large size that they are not accessible to other cells. They also work in an environment where the pH value is high, very actively fighting infectious pathogens, which numerous neutrophil microphages cannot do.
Monocytes in a child’s blood perform a number of important functions.
And most importantly, in the place where the inflammatory process directly occurs, the cells absorb all harmful microorganisms, as well as dead immune particles. As a result of this work of monocytes, damage heals faster and better.
Some features of monocytes
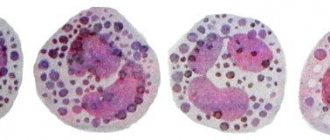
The vast majority of monocytes originate in the bone marrow from a multipatent stem cell, and from a monoblast (ancestor), pass through the stages of promyelomonocyte and promonocyte. Promonocyte is the last stage before the monocyte, the immaturity of which is indicated by a paler, loose nucleus and remnants of nucleoli. Promonocytes contain azurophilic granules (by the way, mature monocytes also have them), but, nevertheless, these cells belong to the agranulocytic series, since the granules of monocytes (lymphocytes, immature cells, histogenic elements) are stained with azure and are a product of protein discolloidosis of the cytoplasm. A certain (small) number of monocytes are formed in the lymph nodes and connective tissue elements of other organs.
The cytoplasm of mature monocytes contains various hydrolytic enzymes (lipases, proteases, verdoperoxidase, carbohydrase), and other biologically active substances, but the presence of lactoferrin and myeloperoxidase can only be detected in trace amounts.
Unlike other cells (for example, neutrophils), the body manages to accelerate the production of monocytes in the bone marrow only slightly, only two or three times. Outside the bone marrow, all cells belonging to phagocytic mononuclear cells proliferate very weakly and limitedly; cells that reach the tissues are replaced only by monocytes circulating in the blood.
Having entered the peripheral blood, monocytes live in it for no more than 3 days, then move to the surrounding tissues, where they finally mature into histiocytes or various highly differentiated macrophages (Kupffer cells of the liver, alveolar macrophages of the lungs).
The norm of monocytes in the blood of a child
Monocytes are elevated in a child, usually due to pathology in the body. White blood cells belong to the group of leukocytes responsible for protecting the body from pests. This group includes: microphages-neutrophils, the main blood cells responsible for the production of antibodies - lymphocytes, a subtype of leukocytes - eosinophils and large granulocytes-basophils.
Monocytes differ from all these cells in size - they are the largest and most active.
A clinical blood test shows in detail all changes in the leukocyte formula. The number of monocytes is determined as a percentage of all other types of leukocytes per 1 liter of blood and should change with the age of the child. Only from the age of 16 until the age of 18, the level of large white cells remains within limits not exceeding 8% of the total leukocyte variety.
Monocytes, what does a child need them for?
Each of the blood components (erythrocytes, leukocytes, monocytes, eosinophils and others) performs a specific function in the body, sometimes several functions. This is how monocytes play an important role in protecting the child. When any foreign material enters the baby’s body, monocytes begin to work. So, their functions can be divided into several areas:
- Participation in cellular immunity. They fight any infection (viruses, bacteria, fungi), toxins, dying cells, poisons and tumor cells.
- After the inflammatory process, dead cells (microbes and leukocytes), toxins, and tissue breakdown products remain in the lesion. Monocytes act as scavengers and remove all these components from this lesion. They also prepare the site of inflammation for regeneration (restoration).
- Protecting healthy tissues from inflamed ones. Monocytes surround the site of inflammation, creating a protective wall. All this prevents inflammation from spreading throughout the body. The same thing happens during the period of destruction of the foreign body, since it is surrounded by a protective layer of monocytes.
Table of monocyte levels by age
To determine the number of macrophages in a blood test, it is necessary to know the age of the child - the number of large white blood cells changes with age.
Normal monocyte count by age:
| Age indicator: days, months, years | MON% |
| 0-1 day | from 3% to 11% |
| from 2 days to 14 days | from 5% to 14% |
| from 14 days to 12 months | from 4% to 11% |
| from 12 months to 24 months | from 3% to 11% |
| from 2 years to 5 years | from 3% to 9% |
| from 5 years to 16 years | from 3% to 9% |
Preparing for the examination
Blood in the urine of a child - possible causes in infants
It is not only foreign proteins that influence the increase in monocytes in the blood. Incorrect preparation of the child for upcoming tests can also increase the number of leukocytes. To make the test reliable, the mother adheres to the following recommendations:
- the day before going to the laboratory, the child is not given fatty or fried foods; if the baby is breastfed, this recommendation applies to the mother’s diet;
- the day before the study, outdoor games and other types of physical activity, as well as stressful situations are excluded;
- a detailed blood test is taken on an empty stomach; Infants should have their last feeding no later than 2 hours before testing.
Important! If the child is taking any medications and they cannot be stopped, the doctor should take this into account when reviewing the results of the study.
What is dangerous about deviation from the norm?
Macrophages are part of the blood immune system, responsible for the timely neutralization and destruction of any viruses, bacteria, microorganisms, parasites, and fungi. In the event of a disturbance in the production of monocytes, the body may be left either without protection or, conversely, excessive production of leukocytes can provoke autoimmune aggression.
Dangers of deviation from the norm:
- the body remains without protection from harmful microorganisms;
- there is no component that promotes favorable conditions for recovery and healing of tissues in the body;
- risk of neoplasms;
- intoxication of the body due to the lack of timely removal of accumulated toxins.
How are monocytes formed?
As soon as foreign microorganisms enter the child’s body, the immune system immediately starts working and begins to synthesize antibodies. Monocyte cells resist pathogen proteins. The more of them are found in the blood, the higher the degree of the disease.
A monocyte is the largest type of white blood cell and is produced by the bone marrow. Elements enter the bloodstream through not yet fully matured cells and live there for about 30 hours. Circulating throughout the body, monocytes settle in tissues, turning into macrophages, whose life cycle is 1.5-2 months.
Experts call these cells “orderlies” that cleanse and renew the blood. The process of destroying microbes is called phagocytosis. It is based on the absorption of pathogenic microbes by monocytes and their digestion.
This type of leukocyte has other “responsibilities”:
- neutralization of parasites;
- “eating” tumor tissues;
- removal of dead cells from the body.
Note! If a child’s monocytes are higher than normal, this means that the immune system is actively fighting microbes, parasites, cancer cells, and allergenic proteins.
Reasons for deviation of monocytes from the norm
The reduced monocyte count in children is small. Because of this, the percentage of deviation is considered to be from 0 to 2 units. In case of such a result, the pediatrician raises the question of monocytopenia syndrome or low levels of macrophages-monocytes in the blood. But this pathological condition is not an independent disease, but a consequence of pathological disorders in the body.
Also, a decrease in monocytes confirms poor functioning of the immune system.
Possible reasons for the decrease in macrophages:
- exhaustion;
- psycho-emotional stress;
- infectious pathologies;
- damage to body tissues in the form of a wound or bruise;
- treatment with ionizing radiation;
- surgical intervention;
- systemic steroid therapy;
- cytostatic treatment;
- impaired hemoglobin synthesis due to iron deficiency;
- general infection of the body by pathogenic microbes that have entered the blood;
- disease of the soft spongy tissue inside the bone;
- high fever;
- normocytic anemia;
- purulent wounds on the surface of the skin;
- acute mental shock;
- blood cancer.
If monocytopenia is detected, the pediatrician prescribes additional tests and examination to find out the cause. An increased level of macrophages is commonly called monocytosis. This condition is not an independent disease, but a secondary one.
Reasons for increased monocytes in the blood in children:
- systemic autoimmune pathologies;
- Epstein-Bar virus infection;
- blood cancer;
- pathological excess of red blood cells in the blood;
- viral pathology is the third disease;
- helminthic infestation;
- joint pathologies;
- erosive gastritis;
- inflammation of the stomach;
- intoxication of the body with chlorine and phosphorus;
- inflammation of the inner lining of the heart;
- Besnier-Beck-Schaumann disease;
- infection with the single-celled parasite Toxoplasma;
- zoonotic infection;
- mycoses;
- infection with Koch's bacillus;
- intrauterine infection of the fetus with the bacterium tryponema pallidum;
- suppuration in the child’s body;
- process after suffering an acute respiratory infection;
- inflammation of the small intestine;
- damage to body tissues in the form of a wound or bruise;
- growth of new teeth;
- a characteristic feature of a given child’s organism (not a pathology).
Characteristics of monocytes
As already mentioned, monocytes are cells that are part of the leukocyte series. They are considered the largest of the white bodies. Their nucleus is also relatively large in size, it is slightly shifted from the center of the cell to the periphery. Monocyte cells are synthesized in the bone marrow, from where they are released into the blood after maturation. They circulate in the blood serum for a very short time - only 72 hours. After this, they spread to almost all tissues of the body. Here they turn into other cells of the immune system - tissue macrophages.
The greatest activity is provided by cells found in the blood - primary monocytes. Tissue macrophages have slightly less functionality.
The main functions of the monocyte-macrophage system include:
1. Phagocytosis – “devouring” bacteria and viruses;
2. Impact on microorganisms using toxic substances;
3. Detrimental effect on parasites penetrating the child’s body;
4. Active influence on the development of inflammation;
5. Participation in tissue regeneration and repair;
6. Ensuring the protection of the child’s body from tumors;
7. Regulation of the formation of new cells of the immune system;
8. Destruction of dead and old leukocyte cells;
9. Control of the production of acute phase proteins - specific substances produced in the liver.
Thus, monocytes perform a huge range of functions, which is why their role in the child’s body is very large.
Symptoms of deviation from the norm
Monocytes are elevated in a child for certain reasons and are accompanied by various symptoms. Abnormal values in the leukocyte formula are accompanied by certain manifestations from the body.
Symptoms of an increased number of monocytes in the body:
- enlargement of peripheral organs of the lymphatic system;
- lack of physical strength and energy;
- chronic fatigue syndrome;
- low-grade body temperature;
- swelling of the nasal mucosa;
- painful sensations in the abdomen;
- sensation preceding vomiting.
Manifestations of a reduced number of macrophages:
- severe intoxication due to the lack of the required number of monocytes absorbing harmful microorganisms;
- skin rashes;
- severe weakness;
- muscle pain;
- frequent colds;
- constant nasal congestion;
- cough;
- joint pain;
- aches throughout the body;
- decreased body temperature;
- hypotension;
- Strong headache;
- bleeding gums;
- small hematomas on the body.
Consequences of relegation
Monocytes in a child’s body perform a variety of functions and their reduction is fraught with certain cavities:
- Weak fight against pathogenic bacteria.
- Insufficient regulation of the immune response and inflammatory reactions.
- Insufficient control over the restoration of damaged tissue.
- Weak antitumor effect.
- Dysregulation of bone marrow functions to produce all blood cells.
- Poor digestion of defective cells.
Which doctor should I contact?
To determine any pathology in a child, you should first visit a pediatrician. During the consultation, the specialist will perform an examination and also ask about any concerns you have. Draw conclusions and prescribe the necessary examinations.
Indications for analysis
An increased or decreased content of monocytes is detected by the general leukocyte formula of a clinical blood test. The indication for prescribing an examination is primarily a change in the child’s age.
And also to determine:
- possible pathological changes during treatment of the primary disease;
- symptoms of unknown etiology in a child;
- in order to analyze the implementation of the prescribed treatment;
- determine the level of the pathological process in the body;
- as a preventive measure to prevent relapse of long-term diseases;
- complications during the treatment of the underlying pathology.
How to prepare for a general blood test?
In order to get a valid test result, you need to properly prepare for the test, and this should be done in advance.
There are certain rules for preparing the body for the procedure for passing the UAC:
- A clinical blood test should be taken on an empty stomach or otherwise - at least 7 hours must pass between the last meal and testing. It is also necessary to remember that juices, teas, compotes, coffee, cocoa are food, albeit liquid, and you should abstain from it. You can and should only drink clean water without gas;
- in some cases, at the discretion of the pediatrician, a general blood test should be done after a meal, but not earlier than 60 minutes before the test. In this case, the food should be low-fat - unsweetened porridge without adding butter, tea without sugar or a glass of kefir, an apple or pear;
- It is necessary 24-48 hours before the examination to exclude from the child’s diet all sweets, fried, smoked, fatty foods (if such foods are present in the diet), chips, crackers, carbonated drinks;
- due to daily fluctuations in blood counts, clinical testing must be done before 10 a.m.;
- If a pediatrician has prescribed a general analysis of venous blood, then you should know what factors can affect the indicators: physical stress, all kinds of jumps, running around, quickly climbing stairs, as well as psycho-emotional arousal or tension. It is necessary to calm the child. Avoid physical education and sports a few days before testing;
- when taking systemic medications, before the study it is necessary to warn the laboratory doctor about the use of medications;
- in the case when a control clinical blood test should be done during drug treatment, then you need to stop taking the drugs before the test, and drink them after taking blood;
- When performing testing to determine the presence of infection, it must be remembered that the result may be negative if there are obvious clinical symptoms of the disease. This fact indicates the individual characteristics of the child’s immune system and does not exclude the presence of pathology. You just need to repeat the analysis result;
- testing (especially repeated testing) must be carried out in the same laboratory for correct interpretation of the results.
Proper preparation for a clinical blood test will contribute to a more accurate test result and a correct diagnosis.
Rules for donating blood
Monocytes (increased in a child due to an incorrect test) are cells that are included in the leukocyte formula of a general blood test. In order to get a real test result that corresponds to reality, it is necessary not only to properly prepare for the test, but also to pass it correctly.
Before undergoing OAC, many patients wonder where to donate blood: from a vein or a finger, and what is the best way to do this. As a rule, for a clinical blood test, taking blood from a finger or capillaries is usually sufficient. If the pediatrician wants to see a more detailed test result, blood is donated from a vein.
This examination is considered more accurate. The explanation for this fact is that during the procedure the finger is squeezed, and the capillaries narrow from the puncture with a scarifier (conditioned reflex) - distorts the result. There is also an opinion that some blood cells settle on the laboratory glass tube, and this fact reduces the information content of the test.
In order to pass the UAC, there are two ways and, accordingly, the same number of rules.
Taking blood from a vein is the most suitable option for a small patient - although it is a longer procedure than with a scarifier, it is less painful.
Process description:
- before entering the manipulation room, it is necessary to calm the child as much as possible;
- in the office you should sit near the table for drawing blood on a chair, and if the child is small, then sit him in your arms. At the same time, you should reassure the baby so that he does not worry;
- Next, the healthcare worker will take a special tourniquet tape and pull the arm just above the elbow. It will be necessary to play a little with the child and work with your fist;
- at this time, the specialist will probe the vein on the elbow, wipe the skin with cotton wool and alcohol, and use a vacuum syringe to draw blood from the vein;
- The duration of the procedure will take a minimum of time;
- Having collected the required amount of blood, the laboratory assistant will press the puncture site with a cotton swab soaked in a sterile medical liquid;
Rules for taking a clinical finger blood test:
- first of all, the parent must calm the child before entering the manipulation room;
- if the child begins to develop strong whims and fear, this may affect the result of the analysis;
- Having entered the office, you should sit down at the manipulation table and place the baby in your arms;
- it is necessary to give the health worker the opportunity to work with the child’s ring finger for a very short time in a calm state;
- the specialist will wipe the skin before the test with cotton wool and alcohol or chlorhexidine;
- using a scarifier or lancet (which greatly simplifies the procedure and makes it less painful), the laboratory assistant will make a puncture in the finger and take blood for the test;
- In infants, the blood test is not taken from the toe - testing is carried out on the heel.
This place has a very well developed capillary network.
Analysis transcript
To determine pathology in a child, it is necessary to correctly interpret test results. A good pediatrician will definitely pay attention to the general leukocyte count, as well as the ESR.
Increased lymphocytes and macrophages:
- the presence of a viral infection in the child’s body;
- active functioning of the immune system;
- ARI or cold.
Decreased lymphocytes and increased monocytes:
- exhaustion;
- general weakening of the immune system.
Simultaneous increase in the number of macrophages and eosinophils:
- allergic reactions;
- helminthic infestations;
- chronic inflammation of the skin;
- seasonal rhinoconjunctivitis;
- long-term disease of the respiratory system;
- malignant blood lesion;
- neoplasms in the lymphatic system.
Increased granulocyte-basophils and monocytes:
- systemic lupus erythematosus;
- rheumatoid arthritis;
- allergic asthma;
- hives.
Increased number of azurophilic granules and macrophages:
- bacterial infections;
- mycoses.
High ROE in monocytosis:
- autoimmune pathological processes;
- allergic reactions;
- heart disease of inflammatory etiology;
- kidney inflammation;
- pneumonia;
- sepsis.
What test do you need to take?
The child has feces like plasticine - possible causes
A general blood test will not provide information about the number of monocytes in a child. The study reveals only the presence of all leukocytes, without dividing them into types.
Therefore, the doctor will prescribe a clinical (detailed) test - leukogram. It is used to determine the content of each type of white cells and their quantitative indicator.
Taking blood for analysis
The detailed analysis also contains information about other blood components, the main ones of which are lymphocytes, neutrophils, eosinophils, ESR, basophils. Deviation from the norm of each of these components will present a clearer picture and allow the doctor to answer the following questions:
- what is the state of the child’s immunity;
- what is the nature of the infection (bacterial or viral);
- at what stage of development is the inflammatory process;
- Are there any complications and pathologies?
An analysis of monocytes and other blood components in combination with existing symptoms will help determine the underlying disease and select the right medications.
What are monocytosis and monocytopenia?
Monocytes are elevated in a child - this is monocytosis. A decrease in the number of cells in the blood is called monocytopenia. Monocytosis is an increase in the number of white blood cells in the blood. This pathological manifestation is not an independent diagnosis (only in the case of the peculiarities of the child’s body).
As a rule, an increase in the number of macrophages is provoked by some reason. In a child's body, monocytosis is a manifestation of the fact that the immune system and blood system cannot cope with the attack of harmful bacteria or viruses. Sometimes an increase in blood monocytes is evidence of a recent inflammatory process in the body or psycho-emotional stress, which is not a deviation.
Monocytosis usually manifests itself as symptoms of a disease that provokes an increase in the level of macrophages in the blood and this, as a rule, is the onset of inflammatory or viral diseases.
Symptoms:
- fatigue;
- weakening of the body;
- changes in mood;
- cold symptoms;
- low-grade fever.
An increase in monocytes in the blood without symptoms or abnormalities in itself is not a disorder. But when monocytosis is detected, it is necessary to monitor the general condition of the child’s body and do control clinical tests at certain intervals so as not to miss the onset of progression of the pathological process.
A decrease in the number of monocytes in the blood or monocytopenia. With this process, the child’s total number of macrophages drops below 2%, which may indicate a sharp decrease in the body’s immune defense. There are a lot of reasons for a decrease - from stressful situations when a child cannot cope with psychological or physical stress to cancer.
If monocytopenia is detected, the pediatrician must prescribe certain additional examinations and make recommendations based on the results. As a rule, monocytopenia requires nutritional correction and restorative procedures. If pathologies are detected, corrective therapy should be prescribed.
Measurement and norm
To determine the number of these blood cells, you need to take a blood test, which in this case is taken from your finger.
The procedure must be carried out on an empty stomach - before this, the child should not eat for 8 hours. You are only allowed to drink a glass of water before going to bed, and another one in the morning before the hospital. In addition, on the previous day it is better not to give the child fatty foods and limit his mobility in order to avoid unnecessary stress and overload for the body. If your child regularly takes certain medications, the doctor should be aware of this - most pharmaceutical drugs distort the results of the monocyte test.
An adult's blood should contain 40-700 million monocytes per liter, depending on the current state of the body.
Such a wide variation is explained not only by the individual characteristics of people, but also by the influence of various stressful situations and even the reaction to seasonal climate changes
In addition, not only the absolute content of cells is important, but also their ratio with other types of white blood cells. In particular, in a person over 16 years of age, the proportion of monocytes should be 1-8%
A level of 9-11% is borderline, but the disease can only be discussed when it persists for more than a month.
https://www.youtube.com/watch?v=1iU7p3nSuKU
But in children everything is much more complicated - the number of leukocytes in their blood changes with age. Accordingly, the number of monocytes is constantly falling, so the norms for each age group will be different. In particular, the blood of children should contain the following absolute number of such cells:
- up to 3 days - 0.18-2.4 billion per liter;
- up to 1 year - 0.17-1.9 billion per liter;
- up to 3 years - 0.15 - 1.7 billion per liter;
- up to 7 years - 0.14-1.5 billion per liter;
The relative content of monocytes in children can be in the range of 3-11%, and even in borderline cases there is no talk of pathology.
Types of monocytosis
Monocytosis is classified into types - percentage (relative) and complete (absolute). Percentage monocytosis can be diagnosed in a clinical blood test based on the ratio of macrophages to other cells of the leukocyte formula. In this case, the level of monocytes, compared to other parts of the immune system, will be higher in percentage terms.
Complete monocytosis does not appear in relation to other types of leukocytes, but together with them.
A large increase in all indicators of the immune system is a criterion for establishing the syndrome of complete or absolute monocytosis. In this case, further examination is required to find out the cause of the pathological change in the CBC.
Carrying out diagnostics
The only way to determine whether a child has elevated monocytes or not is to undergo a general clinical blood test.
In some cases, monocytosis syndrome in children is detected completely by accident. This usually happens during hospital treatment with regular tests for a completely different reason.
If the examination is carried out for the presence of monocytosis, then it is necessary to properly prepare for the tests. The baby should be protected from increased physical activity. Taking medications is also not recommended.
If these factors are excluded, the test results will be more accurate.
How is additional examination of children with monocytosis carried out?
The pediatrician builds the principles of examination for monocytosis on the basis of additional changes in the leukocyte formula:
- with a simultaneous increase in macrophages and cells responsible for humoral immunity (lymphocytes), there will be a suspicion of viruses and infections. It is necessary to pass tests for the presence of foreign microorganisms;
- an increase in monocytes and microphages - eosinophils, is an indicator of the presence of parasites. You should donate blood and feces for helminthic infestations;
- if cardiac pathology is suspected, a lipid complex and rheumatic tests are necessary;
- an increased number of basophils together with macrophages is an indicator of autoimmune aggression. It is necessary to do an ANA profile analysis.
Any additional examinations are prescribed by a pediatrician only after consultation and examination of the child.
Symptoms of elevated monocytes
Monocytosis may be accidentally detected in a child during a routine medical examination. It is usually diagnosed during a targeted examination when the following indications are present:
- fatigue and weakness;
- cough, runny nose;
- feverish condition;
- abdominal pain and diarrhea;
- swelling of the lymph nodes.
Donated blood for testing - the child’s leukocytes are elevated, reasons
Any of these symptoms is already a reason to suspect an inflammatory process or the penetration of infection into the child’s body. Laboratory tests will help determine the severity of the disease.
Note! Natural phenomena can also increase the number of monocytes: teething, restoration of the body after surgery, critical days in a teenage girl.
How to normalize monocyte levels
Any deviations in the functioning of large cells of the leukocyte formula are not an independent disease, and first of all it is necessary to find out the true cause of the changes. But it is necessary to monitor the child’s quality of life - this will be the best preventive method.
It is necessary to provide:
- nutrition balanced in proteins, fats and carbohydrates, appropriate for age;
- correct drinking regime;
- consumption of vitamin complexes;
- in the absence of pathologies - balanced physical activity;
- correct wakefulness and sleep patterns.
How the analysis is done
In children's clinics, blood for a detailed analysis is usually taken from the ring finger, after first puncturing its pad. Sometimes a puncture is made in the heel of a newborn with a scarifier, from which lymphatic capillary fluid is collected into a test tube with a glass tube.
A blood smear is applied to a glass slide and placed into a microscope. Using this instrument, leukocytes are examined. It is not difficult to determine the quantitative composition of each element in a sample - they differ in shape, size and a number of other specific characteristics. This is exactly how a simple calculation of the leukocyte formula occurs.
How else is research done?
In some cases, venous fluid is required, taken from the blood vessel with a syringe. When examining a sample taken, laboratory assistants use hematological analyzers. A test tube with blood is placed in a special device. The device itself is filled with all kinds of reagents that must interact with the lymphatic fluid.
Hematology analyzer
In a matter of seconds, the analyzer will provide information on hematocrit, hemoglobin level, size, shape and number of red blood cells, leukocytes, platelets and other components. The device converts the received information into graphs and issues them in the form of special forms.
Analyzers are able to quickly and effectively determine the leukocyte formula, for which blood is taken from a child.
Analysis without pain
Any analysis is inconvenient for children, since the procedure is painful. In paid clinics, they use an alternative option, as opposed to a metal scarifier, - a plastic lancet. The device looks like a fountain pen and works according to the following principle:
- pressed the button;
- the spring worked;
- she pushed the needle to the desired depth.
The tip of the lancet is so thin that the injection is painless, and the amount of blood is sufficient to draw for testing.
Lancet for blood collection
The device provides the baby with maximum comfort during the procedure, but is not always used, as it costs many times more than a simple scarifier.
Doctor Komarovsky's opinion
The famous doctor Komarovsky has the following opinion regarding monocytosis: in order to avoid deviations in the number of macrophages, it is necessary to monitor your baby’s immunity from birth.
To do this, you need to constantly walk with the child, monitor the air humidity in the house, constantly remember about ventilation, after walks in the fresh air and in the morning, after sleep, you need to rinse the child’s nose with a hypertonic solution. Do not indulge in unauthorized use of antibacterial agents, which leads to disruption of the immune system.
The doctor says that disease is easier to prevent than to treat. In order not to miss an increase in the level of monocytes in the child’s blood, and, accordingly, a pathological process, it is necessary to undergo a timely preventive examination by a pediatrician.
Article design: Oleg Lozinsky
What does it mean when monocytes and lymphocytes are elevated at the same time?
Against the background of the penetration of foreign agents into the body, a triggering reaction of the immune response occurs. To achieve this, the number of specific blood cells increases compared to the normal state. The protection of the immune system ensures the constancy of the internal environment of the child’s body. This is achieved through the production of special substances against specific pathogens (antibodies) or the direct destruction of a foreign agent. Thus, an increase in the level of lymphocytes and monocytes in the child’s bloodstream occurs against the background of activation of his immune system.
Normal in children
This indicator differs from the norm for an adult and depends directly on the age of the child. The standards are presented in the table below.
| Age of child | Norm, % |
| newborns | 3-12 |
| up to a year | 4-10 |
| from one year to 15 years | 3-9 |
| after 15 years | 1-8 |
Decoding a child's blood test
Having received the results of the study of the biomaterial, the doctor immediately pays attention to this parameter - whether the child’s monocytes are normal or deviation from it. To decipher the test, it is also necessary to take into account the age for which its values are acceptable:
- in children under one year of age, the norm is considered to be in the range of 3-12%;
- for a child from 12 months to 15 years, the permissible value is 3-9%;
- in adolescents, monocytes account for about 1-8%.
In addition to the relative parameter, the absolute parameter is also taken into account, showing the number of monocytes in 1 liter of blood. In this case, the lower permissible limit for each age is the same and is 0.05 * 109 / liter. The normal upper limit is:
- at the age of up to one year – 1*109 (in 1 l);
- up to 2 years – 0.6;
- at 3-4 years – 0.5;
- from 5 to 15 years – 0.4.
Ideally, the absolute value should decrease. When a child's abs monocytes are elevated and do not meet age standards, they speak of the development of monocytosis.
Leukocyte formula table
If you believe Dr. Komarovsky, who devoted an entire section to blood tests in his medical reference book, the norm is a conditional concept. Therefore, when comparing the test results of your child with the standard tables, you should not immediately fall into despair, because the average data is indicated there.
To make a diagnosis, it is necessary to pay attention to the indicators of all blood elements presented in the detailed analysis. They can increase along with monocytes, remain normal, or be low.
Associated blood elements
| Name | Description |
| Lymphocytes | Not a single process in the body’s defense system is possible without this element. Its “responsibilities” include detection, recognition, and fight against antigens. Lymphocytes synthesize antibodies and perform a number of other protective functions. If, along with monocytes, there is an increase in this component, they speak of a well-functioning immune system fighting viral and bacterial infections. When, on the contrary, during monocytosis, lymphocytes are lower than normal, this is evidence of a weakened immune system. |
| Basophils | If the analysis shows an excess of this type of leukocytes, the causes may be an autoimmune disease, allergy or internal infection (but not an acute respiratory infection). Under normal conditions, these elements should be no more than 1%; they are necessary for blood clotting. |
| Neutrophils | If monocytes and this type of leukocyte increase simultaneously, the body is said to be infected with fungal spores or bacteria. In this case, lymphocytes are usually low. These elements, in turn, are divided into subtypes: • segmented, emerging from the bone marrow as fully mature cells; • “babies” among neutrophils – myelocytes; • a leukocyte in the “adolescent” stage is called a metamyelocyte. This last element develops very quickly and turns into a band neutrophil. The more of them found in the blood, the more serious the bactericidal attack on the immune system. |
| Eosinophils | Allergic reactions leading to the development of bronchial asthma, hay fever, and atopic dermatitis can increase this indicator. Eosinophils above normal are an indicator of infection with intestinal parasites or worms. In rare situations, a similar picture indicates a blood disease: leukemia or lymphoma. |
| ESR | With monocytosis, an elevated level of erythrocyte sedimentation rate indicates the presence of inflammatory processes (autoimmune, allergic, infectious) in the child’s body. |
Considering the information in this table, it is important to compare the increase in monocytes in the child’s blood with the quantitative indicators of all types of leukocytes. This will allow you to see a clear picture of the disease.
Decryption options
An increasing level of monocytes in children is more often associated with colds, respiratory infections and gastrointestinal disorders. More serious pathologies are also possible. Therefore, when considering a blood test, the doctor pays attention to the following points:
- if the percentage of monocytes is slightly elevated, and the percentage of other types of leukocytes is reduced, while their total number is normal, this indicates relative monocytosis; it is not dangerous and may appear as a sign of a recent illness;
- in some cases, relative monocytosis is interpreted as an indicator of the norm if it is based on heredity (this must be confirmed by laboratory tests of the blood of other family members);
- absolute monocytosis is classified when this type of leukocytes exceeds the equivalent per liter of material; This indicator indicates a pathology hidden in the body.
In the fight against foreign bodies in pathology, monocytes are consumed at high speed. Therefore, the bone marrow has to work harder to replace the missing cells to replace the dead ones.
Pathological causes include an autoimmune state of the body, inflammatory processes in the gastrointestinal tract and oral cavity, infections due to previous operations, poisoning, oncology, tuberculosis, syphilis.
Additional Research
If the child’s blood has elevated monocytes, and the interpretation of the tests does not make it possible to make an unambiguous diagnosis, they resort to additional examinations, with the involvement of doctors of other specialties:
- When there is a suspicion of a fungal, viral or bacterial nature of the pathology, the child is referred to an infectious disease specialist who will prescribe the following tests:
- coptogram;
- bacteriological culture and testing for parasite eggs;
- serological test to confirm pathogens;
- Clinical urine analysis;
- swabs from the throat and nose.
- If the infection is not detected, and the stomach hurts, there is a suspicion of pathology in the abdominal cavity; the child is sent for an ultrasound and consultation with a surgeon or gastroenterologist;
- Monocytosis may accompany another pathology - mononucleosis; therefore, the doctor will definitely examine the lymph nodes and prescribe a special blood test for atypical nuclear cells;
Additional tests
- If, during examination of the baby, a murmur is heard in the baby’s heart, an autoimmune disease may be suspected; in this case, elevated monocytes are supported by rheumatic tests and blood sampling for biochemistry.
From all that has been said, a conclusion suggests itself: a clinical analysis alone is not enough to understand why the baby is not feeling well. Having discovered an overestimated level of monocytes when deciphering the test, correlate it with the indicators of other types of leukocytes. To confirm or refute the presence of pathology, additional examinations and consultations with specialized doctors will be required.
Even a small volume of blood is enough to establish the quantitative content of monocytes and other leukocytes in it. An increased level of enzyme elements indicates the active functioning of the immune system. Deciphering the specific changes obtained during testing will tell you the cause of the baby’s illness, which will allow you to choose the most effective therapy.