5556
Reduced levels of total bilirubin can lead to serious complications. Doctors note that this condition indicates pathological conditions in the body.
Bilirubin is a half-life product of hemoglobin. The substance is responsible for the correct chemical composition of bile produced by the bone marrow and spleen.
Bilirubin is a red-brown bile substance that combines with glucuronic acid. It passes through all the bile ducts, after which it enters the duodenum. The average lifespan of a bilirubin cell is 100 days.
What is bilirubin
Bilirubin is a liver enzyme that enters the bloodstream and is distributed throughout the body. It can be of two types - direct and indirect.
Direct bilirubin is a fraction of the total bilirubin - it is practically non-toxic and completely soluble. This substance is produced by the human liver and after some time enters the intestines. Direct bilirubin enters the blood and then returns to the liver. Also, some of these cells are sent to the large intestine, from where they are excreted naturally.
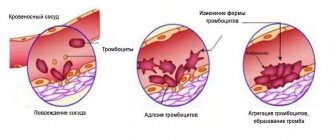
Indirect bilirubin is a bile pigment, the formation of which requires non-working red blood cells. It is present in the blood serum and is excreted by the urinary system. If the concentration of this substance changes, the doctor sends the patient for an extended study, which will help determine the cause of the deviation. The rate of this component depends on its shape. The highest rate is observed in newborns - 3-4 weeks after birth.
Low bilirubin and blood standards
Bilirubin levels vary depending on age
The average total blood bilirubin in a healthy person varies between 8-20.5 µmol/l. Free bilirubin makes up about 75% of the total, and bound bilirubin makes up about 25%. In newborns, indicators may differ significantly from the average and approach normal only after a month:
| Age | Total bilirubin | Free | Connected |
| 1-3 days of life | 23-190 | 22,5-179 | 0,5-11 |
| 4-6 days of life | 28-210 | 27-197 | 1-13 |
| From a month to 14 years | 3-20 | 2-16 | 1-4 |
If for some reason the body begins to produce fewer red blood cells, their destruction also slows down. This condition is rare and indicates a decrease in the amount of bilirubin pigment.
If the indicators deviate from the norm, it is recommended to retake the analysis. The result may be influenced by several factors: the study was not carried out on an empty stomach, or in the evening hours, when physiological indicators decrease. The results of the analysis may also be affected by:
- eating fatty foods the day before the test;
- drug therapy with nicotinic acid, atazinovir, diuretics and many other drugs;
- prolonged fasting;
- physical or mental overload;
- long exposure to the sun;
- the presence of a contrast agent in the blood after other studies.
When is a bilirubin test prescribed?
It is impossible to recognize the signs of low bilirubin - they simply do not exist. If a patient develops anemia, he begins to feel a constant headache, increased fatigue, drowsiness, pallor and dry skin. His hair also splits and his nails break. Visual acuity may decrease.
With coronary heart disease, shortness of breath and constant weakness occur against the background of low bilirubin. If such a condition is accompanied by tuberculosis, then the patient experiences a prolonged cough, increased body temperature, and decreased body weight. Constant monitoring of bilirubin levels is mandatory for pregnant women. This analysis is also required:
- With stagnation of bile and various types of jaundice;
- Hyperbilirubinemia or cholelithiasis;
- For diseases of the biliary tract or liver pathologies;
- With enlarged liver and spleen;
- For diseases of the cardiovascular system;
- For infectious diseases associated with liver damage;
- With long-term use of medications;
- For hemolytic anemia;
- For oncological diseases of the gastrointestinal tract.
Biochemical blood test (11 indicators)
Properly performed laboratory diagnostics ensures the timely formulation of the correct diagnosis, and, consequently, the prescription of adequate treatment, which accelerates the patient’s recovery process. It is also important to monitor the effectiveness of treatment and subsequent monitoring of blood counts after treatment.
Realizing this, more and more animal owners are now
trying to prevent diseases, thereby preventing the possibility of recurrence of the disease
.
After all, more than 50% of the information
The doctor can obtain information about the patient based on biochemical blood parameters.
Blood chemistry
is a laboratory research method that reflects the functional state of the organs (liver, kidneys, heart) and body systems of the animal. With its help, you can “see” inflammatory or rheumatic processes in the animal’s body and thereby prescribe or adjust treatment.
ATTENTION!!! On Timiryazev 46 (veterinary hospital "SQ-lap") and on Filimonova 25G (veterinary clinic "SQ-lap"), if the blood test was taken before 8.00 am, the result will be ready after 17.00 on the same day, if after 8.00 am, then the next day after 17.00.
LDH (LDG) - LACTATE DEHYDROGENASE
LDH
– an important enzyme in glucose metabolism, with its participation pyruvic acid is converted into lactic acid (and vice versa). Lactic acid is the end product of glucose metabolism in cells in the absence of oxygen. LDH is present in all cells of the body, being a kind of “backup option” for glucose metabolism without oxygen. Energy is always needed, but there are situations when oxygen simply does not reach the tissue (for example, when a blood clot blocks a vessel). The level of LDH increases during tissue destruction (it is artificially increased during hemolysis of red blood cells due to improper collection and storage of blood). It is represented by five isoenzymes (LDH1 – LDH5).
An increase is observed:
- damage to myocardial tissue (In this case, the ↑ enzyme itself will be observed 8-11 hours after a heart attack. After 40-73 hours, its activity reaches its maximum. The LDH indicator ↑ is 2-5 times. This critical level remains for another 10 days, but the period may fluctuate depending on the size of the area of the heart muscle that was damaged.)
- leukemia
- necrotic processes
- tumors
- hepatitis
- pancreatitis
- jades
- muscular dystrophies, damage to skeletal muscles
- hemolytic anemia
- circulatory failure
- leptospirosis
- infectious peritonitis of cats.
Decrease value
LDH has no diagnostic value when there is uremia (increased urea concentration).
GPT (ALT, ALT) - ALANINE AMINOTRANSFERASE
Alanine aminotransferase
– the main indicator of cytolysis, an intracellular enzyme involved in the metabolism of amino acids. It can be used even to determine the slightest problems with the liver. Determination of alanine aminotransferase is more informative than determination of aspartate aminotransferase for establishing liver dysfunction. The absolute values of alanine aminotransferase are not directly related to the severity of liver problems, therefore, serial indicators of alanine aminotransferase levels directly over time will become more accurate here. It is found in high concentrations in the liver, kidneys, cardiac and skeletal muscles. Released when tissue is damaged, especially when the liver is damaged.
An increased value gives:
- cell necrosis
- acute and chronic hepatitis
- viral and toxic hepatitis
- cholangitis
- fatty liver
- liver tumors
- use of anticoagulants cardiac muscle necrosis, skeletal muscle necrosis or injury
Reduced value
has no diagnostic value.
DE RITIS COEFFICIENT
De Ritis coefficient
(
dc Ritis coefficient
) is the ratio of
AST
to
ALT
and is a highly reliable marker of damage and necrosis of liver cells (hepatocytes) or myocardium (cardiomyocytes).
The calculation of this coefficient is of greater value in making or confirming a diagnosis than individual AST or ALT values.
Normally, the de Ritis coefficient is 1.3±0.43.
De Ritis coefficient greater than 2
indicates
heart damage
, and
less than 1
indicates
liver damage
.
GOT (AST, AST) - ASPARATE AMINOTRANSFERASE
AST
– Intracellular enzyme involved in amino acid metabolism. It is found in high concentrations in the liver, heart, skeletal muscles, brain, and red blood cells. Normally, the level of this substance in the blood is low. However, if a certain tissue or organ is damaged (heart, liver), AST is released from the damaged cells and the level increases. The amount of this substance in the blood directly depends on the degree of tissue damage. To determine liver damage, determine the value of ALT and AST
Increased value
gives:
- necrosis of liver cells of any etiology
- acute and chronic hepatitis
- fatty liver
- brain tissue damage
- kidney
- use of anticoagulants
- vitamin C
a decrease in value
:
- against the background of vitamin B6 deficiency
- the presence of extensive liver damage (necrosis, cirrhosis).
ALB - ALBUMINS
Albumin
- the most homogeneous fraction of simple proteins, almost exclusively synthesized in the liver. About 40% of albumins are found in plasma, the rest in the intercellular fluid. The main functions of albumins are maintaining oncotic pressure, as well as participating in the transport of small endo- and exogenous substances (free fatty acids, bilirubin, steroid hormones, magnesium, calcium, drugs, etc.). The determination of albumin is used to diagnose liver and kidney diseases, rheumatic diseases, and oncological diseases.
Increased value
gives:
- state of dehydration
- burns
- acute infections
- vomiting, diarrhea
a decrease in value
:
- nutritional dystrophy
- acute and chronic hepatitis
- cirrhosis of the liver
- diseases of the gastrointestinal tract
- nephrotic syndrome
T-Pro - TOTAL PROTEIN
Total protein
Serum consists mainly of albumins and globulins. The globulin level is calculated by subtracting the albumin level from the total protein level. Hypoproteinemia indicates hypoalbuminemia, because. albumin is the main whey protein. Serum protein concentration is determined by nutritional status, liver function, kidney function, hydration and various pathological processes. Protein concentration determines colloid osmotic (oncotic) pressure. Determination of protein in blood serum is used to diagnose liver diseases, kidney diseases, cancer, malnutrition and extensive burns.
Increased value
gives:
- dehydration, venous stasis
- inflammatory processes
- infections
- hyperimmunoglobulinemia
- myeloma (pathological protein)
- injuries and burns
Decrease value
we observe:
- protein loss in gastroenteropathy
- nephrotic syndrome
- decreased protein synthesis
- chronic hepatitis
- hepatosis
- protein malabsorption
- tumors
- gastrointestinal disorder
- parasitosis
- acute and chronic blood loss
- vomiting, diarrhea
- diabetes insipidus
T-Bil - TOTAL BILIRUBIN
Bilirubin
is a rich yellow-brown pigment produced in many organs and tissues and is a product of the final breakdown of hemoglobin and other heme-containing proteins in the cells of the liver, bone marrow and spleen.
Bilirubin is present in the body in two forms:
- direct (connected),
- indirect (free).
Total bilirubin does not exist in its pure form, but is defined as the total amount of direct and indirect, and, normally, direct bilirubin should account for 75% of the total.
Bilirubin is a product of hemoglobin metabolism and is conjugated in the liver with glucuronic acid to form mono- and diglucuronides secreted in the bile (direct bilirubin). Serum bilirubin levels increase with liver disease, biliary obstruction, or hemolysis. Hemolysis produces unconjugated (indirect) bilirubin, therefore, high total bilirubin will be observed with normal direct bilirubin. Increases if there is:
- damage to liver cells of various types
- obstruction of the bile ducts
- hemolytic anemia (B12 deficiency)
- intoxication
Decreased if there is:
- bone marrow diseases
- anemia
- hypoplasia
- fibrosis
ALP - ALKALINE PHOSPHATASE
Alkaline phosphatase
– hydrolysis enzyme, carries out dephosphorylation of many types of molecules (nucleotides, proteins, alkaloids, etc.). Present in almost all tissues of the human body. Its main location in cells is the cell membrane. The most important diagnostic isoenzymes of ALP are: intestinal (location, respectively, intestines), nonspecific (activity is high in the tissues of the liver, bones and kidneys), placental. Main indications for use: liver disease, pathology of the biliary tract, obstruction of bile outflow, cholelithiasis, cancer of the head of the pancreas, bone diseases (osteodystrophy, bone tumors), osteoporosis. ALP is produced in relatively equal proportions by the liver and bones. In young animals during the growth period, the activity of alkaline phosphatase increases several times and is not an informative indicator.
Increased value if:
- healing of fractures begins
- observe tumors and bone disease, osteomalacia, osteoporosis
- hypothyroidism, hypovitaminosis C
- cholangitis
- obstruction of the bile ducts
- gallbladder tumors;
- abscess, cirrhosis, liver cancer, hepatitis
- lung carcinoma
- breast fibroadenoma
- muscle disease
- bacterial infections of the gastrointestinal tract
- pregnancy
Reduced value if:
- hypothyroidism
- weakening of osteoblastic processes
- anemia
- use corticosteroids
CRE - CREATININE
Creatinine
It is considered one of the final products in the body of direct protein metabolism, which allows us to determine the state of the muscular system and human kidneys. Creatinine is one of the elements of residual nitrogen. In turn, residual nitrogen is a collection of non-protein substances in the blood that contain nitrogen.
It promotes the removal of urea, ammonia, and uric acid from the body through the kidneys. It is by the level of creatinine in the blood (and other components of residual nitrogen) that the state of the animal’s excretory system is judged.
Creatinine, as the final product of breakdown reactions, is not consumed in the body for other metabolic processes. This is a compound that is harmful to tissues and should be eliminated from the body as much as possible. An increase in creatinine levels can be physiological, not due to disease, or pathological. In the second case, the main cause of hypercreatinemia is renal failure in any type of kidney damage, in which creatinine numbers can increase several times. Physiological hypercreatinemia can never be represented by a large deviation from the norm. Under no circumstances should you even try to cope with elevated creatinine levels in the blood on your own. This symptom may be the small tip of a large iceberg of illness. Any corrective and therapeutic measures must be supervised by a specialist!
Increases with:
- renal failure
- hyperthyroidism
- the use of furosemide, vitamin C, glucose, indomethacin
- Glomerulonephritis (an early sign, increases before uric acid)
- severe cardiac decompensation
- blockage of the urinary tract
- osteodystrophy
- a persistent increase in creatinine indicates a malfunction of the renal filter
- a doubling of blood creatinine corresponds to a 50% decrease in kidney filtration
- intestinal obstruction
- liver atrophy
- pneumonia
- diabetes mellitus
- increasing urea content
The prognosis of the disease depends on the value of creatinine:
- up to 3 mg%=265 µmol/l careful
- 3-4 mg%=265-354 µmol/l doubtful
- over 4 mg%=354 µmol/l unfavorable
- over 5 mg%=442 µmol/l lethal
Reasons for a possible erroneous increase in creatinine levels:
- presence of ketone bodies
- >1000 not treated
- <40 – may be cancer or cirrhosis.
- the urea/creatinine ratio (0.08 or less) predicts the rate of development of renal failure
Reduction at:
- pregnancy
- age-related decreases in muscle mass
GGT (GGT) - GAMMAGLUTAMIL TRANSFERASE
Gamma-glutamyl transpeptidase (GGT)
- an enzyme that can be found in many parenchymal organs. It is involved in the exchange of nucleic acids and the “construction” of protein molecules. Most gamma-glutamyl transpeptidases are contained in the kidneys, liver and pancreas. In addition, the enzyme is present in the brain, intestines, spleen and skeletal muscles, and in the prostate gland. Inside the cell, GGT is found in the membrane, cytoplasm, and lysosomes.
Determining the level of GGT in the blood is used to diagnose diseases of the liver and biliary tract.
Increases if there is:
- cholangitis
- cholecystitis
- cholelithiasis
- acute viral hepatitis.
- toxic liver damage
- fatty liver
- tumors of the liver and other organs with metastases to the liver
- pancreatitis acute and chronic.
- cholelithiasis
- helminthiasis
- tumors of the pancreas and prostate gland.
- exacerbation of chronic pyelonephritis or glomerulonephritis
Decreases at
decompensated cirrhosis of the liver.
CPK - CREATINE KINASE
Creatine kinase
– a cytosolic enzyme that stimulates the conversion of creatine into creatine phosphate and provides energy for muscle contraction. The reaction, catalyzed by creatine kinase, provides energy for muscle contraction. There are creatine kinase contained in the mitochondria and cytoplasm of cells. This enzyme is used to diagnose muscular dystrophy, myopathy, myocardial infarction and diseases of the central nervous system.
Increases when present in the body:
- degenerative myopathies - ↑ 10-50 times
- small focal infarction - ↑ after 2-3 hours from the attack, after 13-30 hours ↑. 5-10 times, returns to normal within 2-3 days
- large-focal infarction - ↑ 15-20 times on days 5-8.
- with myocarditis
- inflammation and dystrophy of skeletal muscles
- generalized seizures
- tachycardia
- IM injection of analgesics and narcotics
- hyperthermia
- after physical activity, surgery
- acute rheumatism (rheumatoid arthritis, ↑ 5-6 times)
- decreased blood supply to muscles
- congestive heart failure
- diabetes
Decreases when:
- thyrotoxicosis
- under the influence of UV rays
AMY-WIDE - AMYLASE
Amylase
– alpha-amylase is the name of a digestive enzyme responsible for the breakdown and processing of complex carbohydrates in food into simpler compounds. The main part of amylase is produced in the pancreas, less - in the salivary glands and other organs. Once in the digestive system, the enzyme acts on starch and glycogen in food, converting them into glucose, which is absorbed in the intestines. Along with carbohydrates, amylase enters the bloodstream and is removed from the body by the kidneys. The concentration of amylase levels in the blood allows us to evaluate the functioning of the pancreas and the general condition of the patient’s digestive system. In horses, amylase is represented mainly by the beta fraction.
It increases if we observe:
- pancreatitis, mumps, renal failure (acute and chronic)
- poisoning
- diabetes
- acute hepatitis
- primary biliary cirrhosis of the liver
- volvulus of the stomach and intestines
- peritonitis
- disturbance of electrolyte metabolism
Decreased if:
- pancreatic necrosis
- thyrotoxicosis
- poisoning with arsenic, barbiturates and carbon tetrachloride
- use of anticoagulants
URIC ACID - URIC ACID
It is the main product of the catabolism of purine bases, which come partly from the diet and partly through synthesis in the body. It is formed in the liver as a result of the breakdown of nucleotides, deamination of aminopurines and subsequent oxidation of oxypurines. It is excreted from the body by the kidneys, due to which excess nitrogen is removed from the body.
In healthy animals, the level of uric acid may increase slightly with a high purine content in the feed, and decrease with a low-purine diet. Foods rich in purines include red meat, liver, kidneys, brains, tongue, and legumes.
It increases if we observe:
- leukemia, myeloma, lymphoma;
- renal failure;
- acidosis, toxicosis, incl. toxicosis of pregnant women;
- prolonged fasting;
- taking salicylates, diuretics, cytostatics;
- physiological increase (increased physical activity, diet rich in purine bases);
- increased catabolic processes in cancer;
- pernicious (B12-deficiency) anemia;
- diabetes.
Decreased if it goes:
- taking radiocontrast agents, glucocorticoids, azathioprine;
- xanthinuria;
- defects of the proximal tubules of the kidneys;
- low purine diet.
GLU - GLUCOSE
The main source of energy for cells, tissues and the brain is glucose
. It is a nutrient delivered to organ tissue by blood molecules. In turn, it enters the blood from the liver and intestines. Blood glucose level is the main indicator of carbohydrate metabolism. Since glucose is evenly distributed between plasma and formed elements, its amount can be determined both in whole blood and in serum and plasma.
Typically, a healthy body independently regulates glucose levels in order to ensure proper functioning of metabolic and metabolic processes. The range of fluctuations in normal blood sugar is quite narrow, which is why it is possible to quickly and accurately determine the occurrence of disturbances in carbohydrate metabolic processes.
Increases if there is:
- diabetes
- stress, shock
- stroke, myocardial infarction
- excessive physical activity
- chronic liver and kidney diseases
- acute pancreatitis (passing phenomenon when the disease subsides)
- diseases of the kidneys, small intestines
- sometimes with heart failure
- phosphorus poisoning
- benzene, chloroform,
- with insufficient hormonal activity of the endocrine glands
- pancreatic cirrhosis
- toxic, traumatic, mechanical irritation of the central nervous system
- with increased hormonal activity of the thyroid gland
- with strong emotional and mental arousal
- use of corticosteroids, nicotinic acid, vitamin C, diuretics
Decreases if we observe:
- starvation
- diseases of the liver, pancreas
- decreased secretion of growth hormones, thyroxine, glucocorticoids
- stomach cancer, fibrosarcoma
- liver parenchyma damage
- insulin shock
- poisoning
BUN (UREA) - UREA
Urea
is the final product after the breakdown of proteins. It is excreted from the body through the kidneys, an organ that is responsible for the complete elimination of urea from the body. All the rest of its accumulation already indicates the presence of significant problems with the body. Urea is formed in the liver from ammonia and carbon dioxide with the participation of enzymes, being the end product of a number of reactions. The accumulation of urea and other nitrogen-containing compounds in the blood due to renal failure leads to the development of uremia.
Increases if there is:
- renal failure
- excessive protein nutrition
- acute hemolytic anemia
- shock, stress
- vomiting, diarrhea
- acute myocardial infarction
- dehydration
- cardiovascular diseases
- anuria
- prostate tumors
- stones in the urinary tract
- peritonitis
- burns
- intestinal blockage
- severe liver damage
- prolonged high temperature
- pyometra
- increased diuresis
Prerenal factors:
dehydration, increased catabolism, hyperthyroidism, intestinal bleeding, necrosis, hypoadrenocorticism, hypoalbuminemia,
Renal factors:
for acute and chronic nephritis, ruptures of the bladder or ureters, wrinkled kidney, nephrocalcinosis, neoplasia,
Postrenal factors:
calculi, neoplasia, prostate disease.
Prognosis for chronic renal failure
depends on the value of the indicators: with values higher -
- 500%=25.0mmol/l careful
- 200 mg%=33.3 mmol/l doubtful
- 300 mg%=50.0 mmol/l unfavorable
- 3 mmol/l lethal
Decreases when:
- low intake of protein into the body, but can be used as a marker of intoxication, because causes swelling
- severe liver diseases
- pregnancy
T-Cho - TOTAL CHOLESTEROL
— indicator of lipid metabolism. It is found in the blood and tissues of the body in free and esterified forms.
It is a component of cellular plasma membranes, as well as mitochondrial membranes and the endoplasmic reticulum (in smaller quantities). Cholesterol is a precursor to sex hormones, corticosteroids, bile acids, and vitamin D.
Up to 80% of cholesterol is synthesized in the liver, and the rest enters the body with products of animal origin (fatty meat, butter, eggs).
Total cholesterol consists of low- and high-density lipoproteins (LDL and HDL) and about a fifth of triglycerides.
We observe an increase if there is:
- atherosclerosis, coronary heart disease, myocardial infarction;
- liver diseases;
- intra- and extrahepatic cholestasis (primary biliary cirrhosis, extrahepatic jaundice);
- kidney disease (glomerulonephritis, nephrotic syndrome, chronic renal failure);
- chronic pancreatitis and malignant tumors of the pancreas;
- diabetes;
- hypothyroidism;
- deficiency of somatotropic hormone (GH);
- obesity;
- pregnancy;
- prescription of drugs: beta blockers, thiazide diuretics, corticosteroids, aspirin, sulfonamides,
- gout;
- a diet rich in carbohydrates and fats.
We observe a decrease if there is:
- cachexia, starvation;
- malabsorption syndrome;
- severe acute diseases and infections;
- hepatocyte necrosis, end-stage liver cirrhosis, hepatocarcinoma;
- sepsis;
- hyperthyroidism;
- chronic heart failure;
- hypo- and a-betalipoproteinemia;
- megaloblastic anemia;
- chronic obstructive pulmonary diseases, pulmonary tuberculosis;
- taking cholesterol-lowering drugs (cholestyramine);
- prescription of certain medications (clomiphene, estrogens, interferon, neomycin, thyroxine, ketoconazole);
- acute infections.
Ca - TOTAL CALCIUM
Blood calcium level
- an important indicator, since this macroelement is involved in many processes in the body: it is necessary for the formation of bone tissue, is involved in the functioning of muscles, nerves and the cardiovascular system, and is important for metabolism in general. Calcium performs many functions in the body: it participates in the processes of muscle contraction, the mechanisms of hormone secretion, the regulation of the activity of many enzymes, and the process of blood clotting. The level of calcium in the blood serum is one of the most stable indicators, which is maintained by regulating calcium metabolism in bone tissue. Serum calcium is the sum of calcium ions, incl. bound to proteins (mainly albumin). The level of calcium ions is regulated by parathyroid hormone, calcitonin and vitamin D. In addition, calcium metabolism is influenced by glucocorticoids, thyroid, sex hormones, changes in the content of calcium complexing ions in the blood, especially phosphates, magnesium levels and some other factors.
We observe increased content if there is:
- gangrene
- enteritis
- hyperparathyroidism
- fractures and bone tumors
- lymphoma
- leukemia
- sarcoidosis
- vitamin D overdose
- peretonitis
- pancreatic insufficiency
- obstructive jaundice
- tumors of the parathyroid and parathyroid glands
- vascular calcification
- stone formation
We observe a reduced content if there is:
- hypoparathyroidism
- hypovitaminosis D, rickets
- chronic renal failure
- cirrhosis of the liver
- pancreatitis
- exudative diathesis
- osteomalacia
- eczema
- use of anticonvulsants
- pregnancy
Mg - MAGNESIUM
Magnesium
, first of all, is an intracellular cation (60% is found in bones); it is an essential cofactor of numerous enzyme systems, especially ATPases. Magnesium is found in red blood cells, muscles, liver and other organs and tissues. Many vital processes of the body depend on magnesium content. Magnesium influences neuromuscular response and excitability. The concentration of magnesium in the extracellular fluid is determined by its absorption from the intestine, excretion by the kidneys, and exchange with bones and intracellular fluid.
We observe increased content if there is:
- dehydration combined with hypercalcemia
- renal failure
- tissue trauma
- hypocortisolism
- hypothyroidism
- diabetic acidosis
- taking acetylsalicylate (long-term)
We will observe a decrease if there is:
- thyrotoxicosis
- pregnancy
- diarrhea
- vomit
- cirrhosis of the liver
- excessive use of diuretics, calcium salts, citrates (during blood transfusion).
- lack of magnesium in food
- hypokalemia
- eclamsia
- acute pancreatitis
- hyperparathyroidism
P - PHOSPHORUS
Phosphorus
– a vital macroelement for the animal, which is the main component of all cells of the body. It is involved in most metabolic processes in the body and is necessary for the formation of tissues (especially nerve and bone). Phosphorus is needed by the body for energy production, muscle and nervous system functions, and bone growth. Phosphates, being a kind of buffer, play an important role in maintaining the acid-base balance. Phosphorus enters the body with food. Found in many foods, it is absorbed fairly quickly in the small intestine. About 70-80% of phosphorus in the body is bound to calcium, forming the framework of bones and teeth, 10% is in muscles and about 1% in nervous tissue. The remaining part is contained in all cells of the body as an energy reserve. Normally, about 1% of all phosphorus is in the blood.
The phosphorus level is used to diagnose various pathological conditions that cause disturbances in phosphorus-calcium metabolism and to monitor their treatment (together with checking the level of calcium, parathyroid hormone and/or vitamin D. The indicator must be assessed in combination with calcium and alkaline phosphatase.
An increased value gives:
- lymphoma
- leukemia
- ketosis
- for diabetes
- healing bone fractures
- use of diuretics
- renal failure
- massive blood transfusions
- hypoparathyroidism
- hypervitaminosis D
- bone tumors, acromegaly
The reduced value gives:
- hyperparathyroidism,
- hypovitaminosis D (rickets, osteomalacia)
- diseases of the gastrointestinal tract
- renal failure
- nephroscrosis, hydronephrosis
- polycystic kidney disease or neoplasm
- eating disorder
- severe diarrhea and vomiting
- infusion of intravenous glucose
- insulin therapy
- anticonvulsants
- use of drugs.
OUR DEAR CLIENTS
, the information provided here is provided for informational purposes only.
STRONGLY NOT RECOMMENDED
independently
decipher
and
prescribe treatment
.
This should be done EXCLUSIVELY BY THE TREATING DOCTOR
, since a large number of different factors and diagnostic methods need to be taken into account.
It is a comprehensive examination
that gives the attending physician
a complete picture of your pet’s disease
and will allow you to determine the correct tactics for therapy and prevention.
Preparing for analysis
To get the correct test results, the patient is sent for a biochemical blood test. To obtain correct results, you should prepare for the study. The following rules must be observed:
- 3 days before the test, avoid eating fatty, fried foods, which cause the liver to work intensively;
- For a week, you should eliminate alcoholic beverages from your diet and stop smoking;
- Stop taking medications several weeks before the test;
- It is worth completely minimizing physical activity and psychological stress, which also affects chemical processes in the body;
- Try to drink as much clean water as possible - this will help start metabolic processes.
If you follow all the preparatory rules for the tests, you will be able to obtain the correct results of clinical studies.
If you get a bad result, you will definitely be sent for a repeat test - it will help eliminate the possibility of a medical error.
Why does bilirubin decrease during pregnancy?
Reduced bilirubin is observed in the blood of women during pregnancy. This is explained by several factors:
- The red blood cell count naturally decreases at this time.
- During the gestational period, many diseases worsen - chronic ones, those in remission. Other pathologies that were not previously apparent also make themselves felt.
Since low bilirubin is associated with kidney disease, tuberculosis, and anemia, it is necessary to detect the main factor threatening the health of the mother and unborn child.
A biochemical blood test during pregnancy is prescribed to confirm or refute the diagnosis.
Reasons for decreased bilirubin
In a normal and healthy person, there is from 3 to 15 µmol/l in the blood. Immediately after birth, the child lacks this pigment; it appears only at 4-5 weeks of life. The amount of bilirubin does not depend on gender. Statistics show that this figure is usually lower in women. The following reasons can provoke a decrease in this pigment in the blood:
- Kidney failure - this organ does not perform the necessary functions, which is why toxins entering the blood destroy bilirubin. This is usually a chronic pathology, but it can also occur against the background of a long-term inflammatory process;
- Aplastic anemia is a rare disease of the circulatory system that occurs against the background of autoimmune diseases, radiation, poisoning and toxins;
- Acute leukemia is a disease of the bone marrow when it cannot produce enough red blood cells;
- Nutritional exhaustion is a condition that occurs against the background of an unbalanced diet or during intense physical activity;
- Intoxication due to tuberculosis - usually occurs in adolescents and children who develop tuberculosis. Bacteria interfere with the normal functioning of hematopoiesis.
To prescribe effective treatment for this condition, the doctor needs to determine the exact cause that contributed to the development of the degenerative process.
Otherwise, drug therapy will not be sufficiently effective. In 5% of cases, low bilirubin is diagnosed due to medical error - because of this, all patients undergo re-examination.
Treatment
To normalize the level of bilirubin, it is necessary to have a comprehensive effect on the body. People who suffer from this problem first need to completely reconsider their diet. It must contain the required amount of proteins that are responsible for the transfer of oxygen to the liver. You can get it from red meats, buckwheat, and offal.
In addition, you should start taking medications and liver enzymes that make the liver easier to function. The treating specialist can prescribe them. Try to visit your doctor regularly to prevent dangerous complications from occurring.
Prevention
Statistics show that a decrease in bilirubin levels almost always occurs due to the same reasons. To prevent this situation, it is recommended to adhere to the following rules:
- Try to reconsider your diet - the diet should be balanced and nutritious. Try to eat meat every day;
- Give up all bad habits - smoking, alcoholic and carbonated drinks, strong coffee are prohibited;
- Try to spend as much time as possible outdoors and exercise regularly. This improves metabolic processes.
If the patient’s level of bilirubin in the blood decreases, the doctor sends him for an extensive diagnostic examination. It may indicate the development of multiple pathologies. It is very important to provide timely assistance to a person, which will help prevent the occurrence of dangerous negative consequences.
© 2020 – 2020, . All rights reserved.