After laboratory diagnosis of a smear, the gynecologist often informs the patient that she has mixed microflora in the smear. What it is? During a laboratory test, a physician identifies the presence and concentration of harmful microorganisms, the presence of an inflammatory process, and fungus in the biomaterial.
Such diagnostics makes it possible to detect dangerous diseases at a very early stage of development, even before the first alarming symptoms appear. Even a preventive visit to a gynecologist involves taking a smear to analyze the microflora of the cervix and vagina.
In a healthy woman, the ratio of beneficial to harmful bacteria in the genitals is 95:5. If this balance is disturbed, a mixed microflora is diagnosed. It is especially dangerous for girls who are pregnant.
Mixed flora - is it bad?
A gynecological smear is a fairly informative study that clearly indicates the problem, its location and degree of danger. With the help of this analysis, which every woman who comes to see a gynecologist must periodically take, it is possible to identify the source of inflammation and the bacteria that provokes its development in a fairly short time.
Based on the results of the smear, you can not only identify the presence of pathogenic (disease-causing) microorganisms, but also understand what percentage they are in with “beneficial” bacteria. If the alkaline environment of the vagina predominates over the acidic one, this always indicates an imbalance. Normally, lactobacilli predominate in a woman’s vaginal environment—they should be at least 95%. The remaining 5% is occupied by leukocytes, epithelial cells and a mass of microorganisms and “bad” bacteria. Such a small amount of harmful microorganisms does not harm a woman’s health and does not manifest itself as unpleasant symptoms. This percentage ratio of “good” to “bad” bacteria is called the absolute norm, and the woman is gynecologically healthy - there is no inflammation or infection.
The result of a gynecological smear “mixed flora” may indicate that foreign bacteria predominate in the vagina or are present in levels exceeding the permissible norm. Depending on which pathogenic microorganisms predominate in the vagina, therapy should be prescribed. Treatment in each individual case is significantly different, because the body is inhabited by different groups of bacteria and infections, and, accordingly, it is necessary to fight them using different methods.
The smear analysis should be deciphered by an experienced doctor, who will prescribe the medications that will help you get rid of the problems. In the future, I would like to wish you to make it a rule to take a smear test at least once every six months. Then the health of the microflora can be kept under control, and the doctor will be aware of your individual characteristics, selecting the most effective and efficient treatment regimens.
What does brown discharge with an unpleasant odor indicate?
Regardless of the color of the discharge that worries a woman, its unpleasant odor always indicates the presence of an infection. It is not necessary that the infection will lead to the development of an inflammatory process (if it does exist, then an increased number of leukocytes will be detected in the smear), but the risk of developing other diseases is quite likely.
Brown discharge in general should always cause concern in women, because... indicate that they contain blood. Among the most likely causes of their appearance are: pathology of the mucous membrane tissue (endometritis). With this disorder, the classic symptom is brown discharge with an unpleasant odor. Most often they appear before menstruation, but can also be observed in the middle of the cycle, so you could easily confuse them with menstruation, which was later mistakenly confirmed by doctors. As a rule, such discharge is accompanied by unpleasant nagging pain in the lower abdomen.
The main danger of endometritis is the likelihood of it becoming chronic. Women suffering from the chronic form of this disease always have problems while carrying a child, because... pregnancy is constantly under threat of miscarriage. This is not surprising, because the fertilized egg is implanted in the mucosal tissues - the endometrium. There are no guarantees that the egg will implant into the endometrium affected by the disease.
But this is just one version of why brown discharge bothered you. If they recur after treatment, I advise you to visit your doctor again and be more thoroughly checked for any abnormalities.
Sincerely, Natalia.
Mixed flora in a smear in women is sometimes diagnosed during a laboratory test. This is one type of analysis that allows you to identify pathogenic microorganisms in the vagina, their numbers, the possible development of inflammation, as well as the percentage of healthy and pathogenic flora. Analysis of a smear for flora can reveal the presence of fungus and pathogenic microbes (cocci, staphylococci) in the genitals.
Among the varieties of microflora there are:
- rod type, when the number of rods in single leukocytes does not exceed 10 x1 cm2. This is the norm. If it is exceeded, dysbacteriosis or gardnerellosis in the vagina develops. In this form, the microflora is populated by lactobacilli. When deciphering the analysis, doctors take into account the ratio of the number of lactobacilli, leukocytes and erythrocytes;
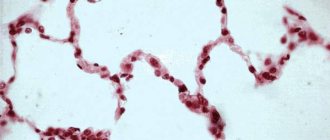
- coccobacillary when detecting an increased content of leukocytes and the complete absence of Dederlein's bacillus. When thick mucus with an unpleasant odor is released from the vagina. Such flora is diagnosed with the development of bacterial vaginosis. Treatment with antibiotics is required.
What is mixed microflora?
Mixed Flora is an imbalance between beneficial and pathogenic bacteria. When studying biological material, you can see the presence of flat epithelium, a large number of lactobacilli, leukocytes, other microorganisms and potentially dangerous bacteria in the vagina. If their number does not exceed the norm, then this is not harmful to the body. If their number increases, then the development of female diseases is possible.
In particular, during pregnancy the concentration of microorganisms in women is often increased. If such a mixed flora is observed, it will be suggested to undergo treatment to avoid the uncontrolled proliferation of pathogenic agents, in particular staphylococci, gonococci, and coccobacilli.
With mixed flora, there is an imbalance between pathogenic and beneficial microorganisms. A healthy body has more beneficial flora (at least 90%), while pathogenic flora is no more than 5%. It is not harmful to women's health and does not pose a risk for developing diseases.
A mixed flora appears in the background:
- taking antibiotics when the functions of the immune system are reduced, thereby creating favorable conditions for the development of pathogenic bacteria;
- the use of contraceptives that can lead to an imbalance between the number of leukocytes and lactobacilli in the vaginal environment;
- the use of intrauterine devices to protect against unwanted pregnancy, which can create an imbalance in the vaginal environment and lead to the development of coccobacilli.
When the flora is colonized by harmful bacteria, dysbacteriosis in the vagina is observed, the development of an inflammatory process, sexually transmitted diseases, discomfort in the genitals (itching, burning), which makes women nervous and worried. You need to contact a gynecologist to clarify the diagnosis and take a smear. If a smear reveals an increase in the number of pathogenic microorganisms that can provoke the development of an inflammatory process, treatment is required to avoid serious negative consequences.
Treatment with folk remedies
Traditional methods of restoring microflora can be a successful addition to drug therapy, enhancing its effect. To do this, you need to contact a gynecologist and select a traditional medicine method that would be combined with the active ingredient of the drugs used.
- You can prepare medicinal tampons yourself. To do this, brew a chamomile decoction according to the prescription on the pharmacy packaging for the collection of chamomile officinalis. Then dip the tampon into the broth, wring it out lightly and insert it into the vagina.
- You can use a purchased tampon, or make your own from sterile cotton wool and gauze.
- Tampons with kefir and honey are also used. First make sure that there are no allergic reactions to honey - a drop of honey is applied to the wrist, rubbed into the skin, and the reaction is observed for six hours.
- To prepare a tampon, you need to soak it in honey and insert it into the vagina in the morning. In the evening, a tampon with kefir is inserted - it is better to purchase bio-kefir or prepare it yourself using pharmaceutical bacterial starter cultures.
- A tampon can also be moistened with sea buckthorn oil and left for several hours.
- Among douching procedures, douching with chamomile with calendula and kefir is popular. At the same time, the doctor may prescribe douching with medicinal solutions, for example, Furacilin.
Tampons should not be kept in place for longer than four hours. Before douching, consultation with a doctor is required, since the procedure is prohibited during pregnancy, endometritis, and fibroids.
Decoding the smear
The interpretation of the smear is carried out exclusively by a gynecologist to confirm the accuracy of the analysis if doubt arises when unpleasant symptoms appear in women. It is not recommended to decipher the smear yourself, although you still need to know some details.
A smear is taken from the vagina to identify mixed flora and submitted to the laboratory for examination.
Normally, there should be at least 95% lactobacilli that can protect the body from harmful microorganisms. There should be no more than 5% of pathogenic bacilli that are not capable of harming the female body. This percentage ratio can indicate the degree of cleanliness in the vagina.
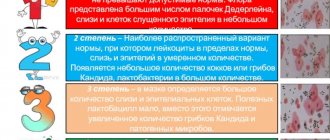
When deciphering a smear, several degrees are distinguished:
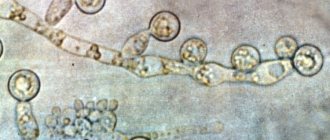
Once pathogenic microflora, cocci, and yeast fungi are confirmed, treatment can no longer be avoided. This indicates the development of an inflammatory process, while women experience burning, itching, unusual vaginal discharge, and increased temperature. This happens with appendicitis, enterobacteriosis, and the appearance of E. coli in the stool. The number of leukocytes in the smear is exceeded, pathogenic microflora is higher than normal. The same situation occurs with bacterial vaginosis caused by streptococci, when itching, burning, and an unpleasant odor are evident. Especially when sperm enters against the background of the release of volatile compounds, indicating the complete absence of lactobacilli, while epithelial cells and leukocytes do not exceed the norm.
What should you pay attention to?
Girls and women should pay attention to the symptoms.
- If severe itching, burning and discharge of unpleasant mucus with an unpleasant odor appear, a venereal disease may develop, which happens in girls at the beginning of puberty or in women with the onset of menopause.
- It is important to pay attention to the rules for taking a smear test for flora. Before the procedure, you should not take baths, use candles, tampons or tablets. You should avoid going to the toilet 2 hours before your smear test.
- You can douche the day before, but only with warm water without using soap or other hygiene products.
- You cannot take a smear during your period, at the beginning or at the end of the cycle.
- When taking a swab from the nasopharynx, you must refrain from eating and drinking water.
- Women pay attention to symptoms. Maybe the lower abdomen hurts, there is redness, itching, nonspecific discharge from the genitals, which happens after long-term use of antibiotics and candidiasis is diagnosed.
It is important for women to know what should and should not be in a smear. In order to check your flora, whether there is any development of the inflammatory process and whether the microorganisms in the smear are normal in order to avoid the development of infectious pathogens: Candida fungus, streptococcus, staphylococcus, gonococcus, gram-negative bacteria. For example, the presence of streptococci in the flora in large quantities can lead to miscarriage, fetal death in pregnant women, the development of inflammatory processes in the genitourinary system, damage to the ureter, bladder and genital organs.
A low level of estrogen in the body indicates the proliferation of the Dederlein bacillus or dysbacteriosis with an increased content of leukocytes and the absence of the Dederlein bacillus, while the ratio between red blood cells and lactobacilli is disturbed. This may happen after long-term use of antibiotics. Leads to cervical erosion and the development of inflammatory processes in the genitourinary system. The growth of pathogenic flora in the vagina inevitably leads to inflammation in the vaginal mucosa, the development of nonspecific inflammation, such as mixed flora.
Causes
The most common reasons are external factors:
- Hypothermia;
- Inadequate regimen for taking hormonal medications;
- Irregular sex life;
- Climate change;
- Long-term treatment with antibiotics;
- Violation of personal hygiene rules;
- Intestinal dysbiosis;
- Infections and inflammatory processes in the pelvic organs;
- Incorrect use of tampons and pads during menstruation, untimely replacement of personal hygiene products.
Normally, the immune system is able to independently regulate the ratio of bacteria, and restoration of the vaginal microflora occurs without the help of medications. If a woman constantly faces one of the risk factors, the normalization of the vaginal microflora is carried out with special preparations.
What does a smear mean during pregnancy?
Each woman’s body is individual and the microflora may have its own characteristics. During pregnancy, the number of pathogenic microorganisms increases and the development of candidiasis, thrush and bacterial vaginosis is possible due to an imbalance in the acid-base balance.
Similar changes in the vaginal flora are observed during infection of the genital organs, exacerbation of chronic diseases, and hormonal changes.
Even at the stage of pregnancy planning, it is important for women to be tested for microflora in the vagina in order to avoid the development of an inflammatory process, which may well occur with unstable immunity and hormonal levels during pregnancy. Pathogenic flora should not be more than 5%. A change in pH, its increase, occurs for a number of reasons: not only with reduced immunity and long-term use of antibiotics, but also with the occurrence of inflammatory diseases, imbalance in the vagina, which, of course, can negatively affect the development of the fetus.
The main thing is to prevent the development of serious illnesses and the spread of candida and coccobacillary flora. Timely smear testing and interpretation of the results allows you to prevent the disease, quickly stop the development of microorganisms, thereby normalizing the pH level in the vaginal environment, and suppressing the activity of microorganisms.
If dysbacteriosis, severe discomfort, an imbalance between pathogenic and opportunistic microorganisms, also coccus bacillus, gonococcus, which are harmful to the body, are detected, their constant growth is noted, then the doctor will prescribe antibiotic treatment. If a mixed flora is detected in a smear during pregnancy, treatment is prescribed in combination to suppress pathogenic agents: staphylococci, gonococci, coccobacilli. Self-medication is unacceptable. If unpleasant symptoms appear, women urgently need to visit a gynecologist.
Flora in the vagina. How to restore vaginal microflora: oral and vaginal medications
Violation of the vaginal microflora - bacterial vaginosis, dysbiosis, (gardnerellosis) non-inflammatory disease.
If the doctor says one of these names, don’t be too alarmed. You can restore the vaginal microflora in a few days, if you have not advanced the condition too much and have not allowed vulvovaginitis (this is already inflammation). How to treat it, at home or see a doctor, depends on how you feel, your general health and the reasons that led to vaginosis. Very often you can restore the vaginal microflora yourself. But a doctor’s examination is a prerequisite.
What causes disruption of the vaginal microflora?
To know how not to get sick or how to recover, it is important to have information about the norms of the condition of the female genital organs and take into account several facts and rules:
- Check your smell. Just as saliva containing alkali is secreted in the mouth, so the uterus secretes special mucus, which creates an already acidic environment in the uterus, cervix, vagina, and vulva. Therefore, normally, women may have translucent, whitish, slightly cheesy discharge with a slight sour-milk odor, sometimes almost like thrush. In such an environment, pathogenic microbes cannot multiply. The vagina is warm, damp, dark. Microorganisms and fungi, beneficial and pathogenic, live there side by side and each perform their own function. The number of pathogenic microorganisms is regulated precisely by the acidic secretions of lactobacilli. As soon as you feel that the usual smell of matsoni and kefir is gone, watch your health and include fermented milk products and sauerkraut in your diet. If after 3–4 days the smell does not change, a feeling of dryness and discomfort appears, consult your doctor.
- There should not be any grayish, much less greenish, discharge. Go get tested and get treatment.
- The smell of rotten fish is a signal for an urgent visit to the gynecologist. Attention! This is not a normal smell for a healthy woman.
- Do not douche under any circumstances unless specifically instructed to do so by your doctor. Constantly washing out the natural flora of the vagina means putting up a sign: “Welcome, infection! Come in, bad bacteria, live here as you want!” Personal hygiene is the washing of the external genitalia and perineum. There is no need to wash or soap yourself inside. It is harmful. It is especially important to remember this for those women who protect themselves by inserting a piece of laundry soap into the vagina.
- The vaginal microflora is capable of self-repair. Therefore, it happens that vaginosis spontaneously appears and disappears in a woman.
- Pathogenic microflora is eliminated due to the release of lactic acid bacteria and their metabolic products - a small amount of hydrogen peroxide.