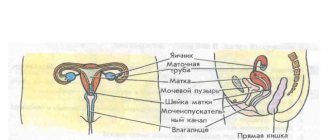
To diagnose various diseases in women, gynecology often uses ultrasound examination, including transvaginal examination. Endometriosis on ultrasound is visualized as tissue that has grown beyond the internal confines of the uterus. Pathological foci can be located in the ovaries, tubes, partly in the abdominal cavity, upper part of the cervix, and in rare cases - in the rectum.
When to do an ultrasound for endometriosis?
Ultrasound for endometriosis is prescribed to patients to monitor the behavior of the mucous membrane and examine nearby organs. If the patient’s diagnosis has already been confirmed, then sonological examinations are scheduled to assess the effectiveness of treatment at intervals of three months. In the remission stage - every six months.
Diagnosis is also carried out if endometriosis is suspected with the following complaints:
- spotting discharge is present for a week before menstruation and two weeks after it;
- long periods, having a brown or rich burgundy hue;
- unstable cycle;
- absence of pregnancy during sexual activity without contraception for 6 months;
- pain in the pelvic area, lower back;
- discomfort during sexual intercourse.
After abortions, spontaneous miscarriages, childbirth, and if an ovarian cyst is suspected, an ultrasound is also prescribed, during which endometriosis may be suspected.
Main forms and symptoms of endometriosis
Endometriosis usually affects women of reproductive age. Often this disease is discovered unexpectedly, for example, during a preventive examination.
It is transvaginal ultrasound that is considered the main method for identifying this pathology.
The types of this disease are distinguished from the location of the foci of tissue proliferation:
- adenomyosis;
- perineal, cervical and vaginal;
- pipe;
- ovarian.
Women suffering from endometriosis may most often experience the following unpleasant symptoms:
- duration of menstruation and their pain;
- the appearance of clots during menstruation;
- chronic pain in the lower abdomen, starting in the middle of the cycle;
- spotting brown discharge outside the menstrual cycle (in the middle, a few days before and after the cycle);
- pain during sexual intercourse, urination, defecation, exertion;
- infertility for unknown reasons.
Types of studies
There are three methods for detecting endometriosis on ultrasound:
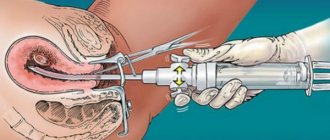
- transvaginal - the most reliable method, involves inserting a sensor into the vagina followed by scanning the pelvic organs and uterine cavity;
- transabdominal - a less revealing diagnostic method, involving scanning through the abdominal wall;
- transrectal - the sensor is inserted through the anus and shows a picture similar in information content to transvaginal examination (for young girls who are not sexually active, it is better to do an ultrasound in this way).
There are more reliable methods for identifying endometriosis.
Diagnosis of a hormone-dependent disease involves the following manipulations:
- colposcopy – determines cervical endometriosis;
- hysteroscopy – identifies lesions in the cavity of the reproductive organ, in the muscle layer and the mouth of the tubes;
- laparoscopy – detects endometriosis of the abdominal cavity, ovaries, intestines and other organs;
- MRI, CT - makes it possible to determine the location of lesions, cysts and the stage of development of the disease.
Tests for diagnosing endometriosis
Endometriosis diagnosis is a difficult issue.
The complexity of the course of this pathology often leads to difficulties in identifying it during ultrasound diagnostics. In this case, patients with unclear symptoms are prescribed other additional research methods.
Only a specialist can decide what types of tests to prescribe for this disease. In some cases, only the laparoscopic method (low-traumatic surgical method) can establish a final conclusion.
Diagnostic methods for detecting endometriosis
- Cytological examination: used for screening diagnosis of many uterine pathologies, however, this method is not able to reveal the full picture of the disease.
- A study on tumor markers: in case of endometriosis, it is indicative, since their number is increased here. In this case, it is possible to assess the severity of the disease and the effect of the therapy. Typically, this method is used in parallel with analysis of hormones (progesterone, prolactin, testosterone).
- Colposcopy: a colposcope is inserted through the vagina using special solutions (acetic acid, iodine, Lugol's solution). However, the method has contraindications (not earlier than 1 month after an abortion and 2 months after childbirth or uterine surgery, intolerance to the medications used).
- Biopsy: A piece of tissue is removed for examination. It is used immediately after menstruation. It requires highly qualified specialists: a surgeon and a pathologist. Otherwise, the disease can be missed. After local anesthesia, a tube with a piston is inserted to collect tissue. After 10-14 days, the result is ready. With this method, the diagnostic accuracy is about 98%.
- Computed tomography: allows you to determine the pathology, its type and connection with other female organs.
- Magnetic resonance imaging: has high resolution and diagnostic accuracy of up to 96%. In this case, nuclear magnetic resonance is used. This method is associated with maintaining the patient's immobility, so it is contraindicated in patients with claustrophobia, patients with pacemakers and hearing aids, and seriously ill patients. This is a painless method; it is only accompanied by noise.
- Laparoscopy: makes a diagnosis with high accuracy - up to 96%. Endometriosis is diagnosed in and outside the uterus. A laparoscope with a flexible cable and lenses connected to a video camera is inserted through a small puncture in the abdominal wall. The device distributes foci of pathologies by color and shape, determining their size and degree of maturity. This is a progressive, low-traumatic method, without complications in the form of scars or any pain. The recovery of patients after it is rapid: laparoscopy is considered the “gold standard” among all types of examinations.
- Hysteroscopy: In this method, the hysteroscope is inserted through the cervix. It is also used to treat pathologies. The procedure requires anesthesia (local or general). To straighten the uterus, carbon dioxide or liquid (saline or saline solution) is first injected into it. This study is carried out on days 8-10 of the cycle. Hysteroscopy has several advantages: the absence of adhesions due to low trauma, excellent viewing of the walls of the uterus, and a minimum of complications.
However, no examination method provides 100% confirmation of the diagnosis of endometriosis. For any method, an important factor is the professionalism and qualifications of the doctor.
Structural changes in the endometrium
When prescribing an ultrasound for endometriosis, the doctor chooses the optimal time for scanning. The diagnostic result depends on the correctness of the set parameter. To understand what day of the cycle to do a pelvic ultrasound, you need to know what structural changes occur in the mucous membrane of the reproductive organ during the menstrual period.
- Proliferation - occurs from the final days of bleeding and ends a few days before ovulation. The structure of the endometrium changes, cells gradually divide, and the thickness of the mucous membrane increases. At this stage, the ultrasound protocol can note pathologies such as polyps and cancer (due to the fact that the endometrium is thin and the tumor remains the same size). Endometriosis is quite difficult to detect at the proliferation stage.
- Secretion begins immediately after ovulation and lasts 10-14 days. During this period, more signs of endometriosis can be detected on ultrasound, if the disease is present. The functional layer of the hollow organ, under the influence of hormones produced by the endocrine gland (corpus luteum), grows, becomes loose and acquires depressions.
- Ischemic – occurs at the final stage of the previous phase. The structural change in the endometrium comes down to the fact that the spiral arteries contract, become damaged, and blood is released from them. This method begins a new menstrual cycle, opening the menstrual phase.
Ultrasonographic stages of development of normal endometrium
The onset of pregnancy depends not only on the functioning of the ovaries, but also on the functional state of the uterine epithelium - the endometrium. Since during folliculometry it is possible to examine the endometrium, a large number of scientists are studying the indicators and echostructure of the inner uterine lining, which are the most optimal for conceiving and bearing a child:
- How the endometrium looks on ultrasound depends on the level of concentration of estrogen and progesterone in the blood plasma. In addition, ultrasonographic features of the structure of the uterine mucosa are directly dependent on the phase of the menstrual cycle. On the days of menstruation, only a thin and broken line of a hyperechoic nature is recorded in the projection of the uterine cavity.
- In the proliferative phase, the anteroposterior size of the uterine mucosa thickens to 3.5 mm, and the echostructure becomes isoechoic and more homogeneous. In this case, ultrasound signs such as a slight decrease in echogenicity and increased homogeneity indicate the rapid development of glands, which also change their location. After ovulation has occurred, the endometrium of the uterus on ultrasound acquires a higher echogenicity due to the accumulation of a large amount of secretion in the dilated ducts of the glands.
- During the periovulatory period, the entire endometrial tissue is somewhat hypoechoic. This sign serves as a reliable criterion that reflects ovulation that has occurred. However, when performing transvaginal echography, this endometrial condition occurs before and after ovulation. During the secretory phase, the thickness of the endometrium reaches its maximum, which is 6-12 mm. At the same time, in the luteal phase, echogenicity is also increased, which is explained by changes in the glandular component and swelling of the endometrial stroma.
- The effect on the endometrium of medications aimed at stimulating ovulation is also proven by ultrasound, although it has no practical significance.
- A diagnostically significant innovation in the functional state of the uterus is the registration of “peristaltic waves” of the epithelial lining of the uterus during transvaginal ultrasound.
Preparation
Depending on the type of endometriosis test chosen, certain preparation frameworks and rules are established. First of all, the doctor selects the day of the cycle when the scan will be performed. All nuances are discussed with a specialist individually.
The regularity of the menstrual cycle and its length play a significant role.
The next stage of preparation includes hygiene procedures.
- Before a transvaginal scan, a woman needs to toilet her external genitalia.
- When choosing a transabdominal research technique, no measures need to be taken. In some cases, to improve visualization of the uterus, the sonologist asks the patient to drink 2 glasses of water 10-15 minutes before the diagnosis and not to urinate after that. This recommendation is individual, so there is no need to fill the bladder without additional requirements.
- Transrectal examination involves inserting a probe into the rectum. To ensure that visualization is not difficult, the digestive tract must be emptied. Preparing for an ultrasound requires the patient to exclude a heavy dinner on the eve of the examination. On the day of diagnosis, you should not eat so as not to cause increased gas formation. A transrectal ultrasound is usually scheduled for the first half of the day, so there should be no difficulty in abstaining from food.
Immediately before the manipulation, a woman should expose her lower abdomen (for transabdominal diagnosis) or undress below the waist (for transvaginal and transrectal methods). The study is performed in a horizontal position and takes on average 10-30 minutes.
On what day of the cycle is it better to do an ultrasound?
Foci of endometriosis can be determined by ultrasound only if the rule is to select the day of the cycle for diagnosis. Patients with regular menstruation are advised to undergo examination shortly before the start of their next menstruation.
It is important to consider that not all women have the same duration of this period:
- with a cycle of 21 days, an ultrasound is performed on days 18-20;
- with a cycle of 35 days, the study is performed on days 30-34;
- with a cycle of 28 days, scanning is carried out on days 25-30.
The closer to menstruation the study is performed, the more likely it is to get an effective answer. Immediately after menstruation, the thickness of the endometrium is minimal. Therefore, the answer to the question of whether endometriosis can be seen before ovulation (when ultrasounds are usually performed) is no. If you do an ultrasound before menstruation, the thickness of the functional layer will be greater, as well as the volume of pathological foci will increase. It will be easier for the sonologist to examine their location.
Patients undergoing menopause undergo an ultrasound scan to determine endometriosis any day. The absence of hormonal changes within a month gives reason to believe that pathological areas do not undergo changes and always remain in the same condition.
In postmenopausal women, endometriosis reverses over the years, except in cases where pathological areas become malignant.
What is the endometrium and its functions
The endometrium is the inner (mucous) layer of the uterus and consists of uterine glands, connective tissue rich in blood vessels and prismatic single-layer epithelium. The structure of the latter consists of the presence of a thin main membrane, basal (from which cells differentiate) and functional layers.
The basal layer is located on the muscular layer and, being relatively permanent, is the source of new cells necessary to restore the functional layer after menstruation. Its normal thickness does not exceed 1.5 cm. In addition, the composition of this layer is rich in the mouths of the glands, which branch widely and penetrate into the functional layer, and connective tissue cells tightly adjacent to each other. It also contains a huge number of small vessels coming from the middle lining of the uterus.
The basal layer reacts extremely poorly to cyclical changes in a woman’s body. Due to its growth, there is a constant regeneration of cells of the functional layer, which were destroyed and exfoliated as a result of menstrual or dysfunctional bleeding, after childbirth or diagnostic curettage of the uterus.
The endometrium undergoes monthly cyclic changes under the influence of sex hormones. In the second period of the menstrual cycle, its thickness increases significantly and, accordingly, local blood circulation increases. If fertilization of the egg does not occur, the cells of the functional layer desquamate, which manifests itself in the form of menstrual bleeding.
The main functions of the inner lining of the uterus are to prepare the environment for a possible pregnancy and to prevent the walls of the uterus from sticking together, which prevents the development of adhesions.
Is endometriosis visible on ultrasound?
It is impossible to say for sure whether a benign process will be visible during an ultrasound. Much depends on the quality of the equipment used for sonography. The qualifications of the specialist performing the examination are also important. Modern sensors, clear monitors, more accurate ultrasound pulses and skills in working with the latest equipment are the key to an accurate ultrasound scanning result.
The stage of development of the pathology matters. At the initial stages, the test result may not identify lesions even if they are present. Cells of the functional layer, located pathologically, are difficult to see on a black and white screen. If the disease is stage 2-4, then it will not be difficult to determine it on an ultrasound. However, it cannot be reliably stated that this is endometriosis. Only differential diagnosis can show the exact identity of the neoplasm.
There are cases when a patient was diagnosed with endometriosis on ultrasound, but this was not subsequently confirmed.
Decoding the results
Using ultrasound, diseases of the female reproductive system are detected:
- endometriosis;
- endometritis;
- endometrial hyperplasia;
- cancer.
Endometriosis
Endometriosis is detected by ultrasound in the form of nodes of various sizes. Specific signs depend on the type of disease. There are external and internal endometriosis. The first includes all manifestations outside the uterus. One of the most common is a retrocervical lesion, located in the tissue between the rectum and uterus. The second includes endometriosis of the body and cervix.
In addition, the disease is divided into:
- focal form, in which the focus is located deep in the muscle;
- diffuse, in which the endometrium penetrates into the wall of the uterus without forming a lesion;
- nodular form, when glandular tissue predominates in the structure of the node.
Sometimes a combination of forms is observed.
The main signs of endometriosis determined by ultrasound:
- Diffuse form - the endometrium is uneven, the uterine wall is thickened, there are inclusions - calcifications.
- Nodular form - the presence of round or oval cystic formations ranging in size from 2 to 30 mm without clear contours, an interstitial node may be detected.
- Focal – thickening of the uterine wall due to the muscular layer, detection of neoplasms in the form of nodes from 2 to 16 mm in diameter with uneven contours.
Postmenopausal endometriosis looks similar to menopausal endometriosis, but the changes are usually clearer and can be seen more easily with ultrasound.
See the full story on the disease, Dr. Myasnikov explains the concepts:
Endometritis
Chronic and acute endometritis is clearly visible during ultrasound examination. Signs of endometritis detected by ultrasound:
- thickening, swelling of the endometrium during acute inflammation;
- depletion of the endometrium with a decrease in its thickness due to chronic endometritis;
- uterine displacement;
- uneven enlargement of the uterine body;
- adhesions.
To view a review on the topic of this pathology:
Endometrial hyperplasia
In unfavorable cases, endometriosis can be complicated by endometrial hyperplasia. This is a process of thickening of the uterine wall, which can result in malignancy - degeneration into cancer. With this disease, pregnancy is impossible. Sonographic signs of endometrial hyperplasia:
- areas of high density;
- thickening of the endometrium;
- presence of small inclusions;
- cysts, neoplasms of various sizes;
- rarely - polyps.
Ultrasound should be performed from the 1st to the 3rd days of the menstrual cycle for women of reproductive age. If a woman has reached menopause, then on any convenient day. During this period, hormonal fluctuations have a stronger effect on the growth of hyperplastic areas. Ultrasound signs of endometrial hyperplasia in menopause:
- thickening of the uterine mucosa;
- polyps and cysts are more common;
- neoplasms with an unclear contour.
If hyperplasia is suspected, a tissue biopsy is performed and the resulting material is examined under a microscope.
In addition, see what hyperplasia looks like:
Cancer
Signs of endometrial cancer detected on ultrasound:
- heterogeneity of contours;
- increased blood flow in the area of education;
- the vessels in the tumor are tortuous and randomly located;
- the density of formation is increased;
- lack of a clear boundary with unchanged uterine tissue.
How well endometriosis is visible on ultrasound depends on its stage:
- The 1st is characterized by minimal changes in the endometrium, which are practically indistinguishable on ultrasound.
- At stage 2, the muscular layer is involved, the wall of the uterus becomes more dense and becomes more visible to ultrasound.
- At the 3rd stage of the disease, the neoplasm grows through the entire wall of the uterus, which is clearly visible on ultrasound.
- The 4th is accompanied by the appearance of pathological foci in the pelvis, peritoneum, intestines, and eyes. Easily diagnosed by ultrasound examination.
Additionally, read the article about uterine cancer on ultrasound.
In addition, watch a video on the topic of oncology:
Endometrioid cyst
In addition to the stage of endometriosis, the experience of the diagnostician and the modernity of the ultrasound machine play a role.
Ovarian endometriosis is often complicated by the appearance of an endometrioid cyst. This is a cavity filled with liquid, which can reach up to 20 cm in diameter. When performing an ultrasound, you can suspect a pathology if you find:
- heterogeneous ovarian inclusions of various structures, shapes, sizes;
- rounded neoplasms;
- swelling of ovarian tissue.
An obstetrician-gynecologist will explain the topic in more detail in the video:
Norms
The basis for diagnosing hyperplasia is determining the thickness of the endometrium using ultrasound. Different periods of a woman’s life have their own standards. This is due to hormonal activity.
In reproductive age, the thickness of the endometrium is maximum on the 19th–23rd day of the cycle; normally it is 1.0–2.1 cm; in the absence of pathology, it becomes loose, fluffy, and before menstruation it decreases to 1.0–1.8 cm.
The thickness of the unchanged endometrium during menopause does not exceed 5 mm. If an increase in this indicator to 7 mm is detected, then a control ultrasound is prescribed after 3–6 months. If a thickening of 8 mm or more is detected, a diagnosis of endometrial hyperplasia is made, and the woman is referred for diagnostic curettage.
In an ultrasound study during menopause, the thickness of the endometrium is taken to be up to 5 mm. Thickening of more than 8 mm is a reason for diagnostic curettage.
With the glandular type of endometrial hyperplasia, you can often find a polyp, which looks like a clearly visible round or oval formation on a broad base or stalk. The length ranges from 1–2 mm to 10–80 mm, rarely more than 80 mm. Clear contours indicate benign quality.
The walls have a smooth hyperechoic junction line
What will show
During an ultrasound examination for endometriosis (suspicion of it), other pathologies may be detected in the patient, for example, endometritis or hyperplasia. With endometritis, inflammation of the mucous membrane of the reproductive organ develops. This is accompanied by uneven thickening. Hyperplasia is characterized by excessive proliferation of cells in the mucous layer of the reproductive organ.
During an ultrasound, the following conditions may indicate endometriosis:
- hypoechoic inclusions in the thickness of the myometrium;
- multilocular neoplasm on the ovary;
- deformation and increase in the volume of the uterus, corresponding to pregnancy by week (from 5 to 7);
- unnatural arrangement of the pelvic organs, indicating a progressive adhesive process.
If there are echo signs of endometriosis, then before starting treatment, it is necessary to carry out a differential diagnosis. In some cases, the detected formations have a different origin and, accordingly, require different treatment. A similar clinical picture has: fibroids, polyps, functional or dermoid ovarian cysts, malignant neoplasms of the pelvic organs.