Share on social media networks:
IVF after laparoscopy is a way to increase the possibility of successful completion of the protocol with the development of pregnancy. Laparoscopic surgery is one of the modern low-traumatic interventions performed for various pathological conditions. A negative result after in vitro fertilization may occur due to diseases that could not be diagnosed by other research methods. Therefore, laparoscopy before IVF allows you to increase the chance of pregnancy after the first embryo transfer. Laparoscopic intervention during a diagnostic study can turn into surgery. This saves time during the recovery period and brings the start of the IVF protocol closer. Using laparoscopy, myomatous nodes, cysts, fallopian tube adhesions and other gynecological diseases that prevent pregnancy are removed.
Experts assure that the course of pregnancy after laparoscopy and without it has no significant differences. Therefore, all fears associated with the need to perform research are unfounded.
What is laparoscopy?
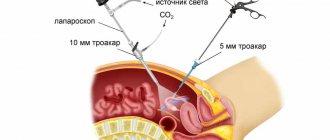
Laparoscopy is a method of examining internal organs using a laparoscope. This is a modern way of performing diagnostics and operations. Laparoscopy is a minimally invasive surgical procedure, which makes the recovery period after surgery much faster.
IVF after laparoscopy has a greater chance of resulting in pregnancy. Other preliminary diagnostic methods may not detect some gynecological diseases. Their presence is often the reason for a negative protocol result. Therefore, laparoscopic examination before in vitro fertilization is necessary in order to timely detect pathology.
During the study, surgical intervention may be performed. The minimum number of incisions does not injure nearby organs and tissues. Therefore, the recovery period after laparoscopy is much shorter than with abdominal surgery. The next advantage of the method is the ability to monitor the progress of the operation through the monitor screen. The doctor assesses the condition of the mucous membranes, the presence or absence of tumors. During laparoscopy, material is collected for histological examination. A biopsy allows you to determine the nature of the formations and make a final diagnosis.
What is follicle puncture?
According to IVF technology, the meeting of male and female germ cells occurs outside the mother’s body. To carry out this procedure, it is necessary to extract female germ cells - oocytes from the ovaries. This operation is carried out by puncturing the ovaries with a special aspiration system with a hollow needle under ultrasound control and collecting fluid containing eggs from functionally mature follicles.
Follicles are small vesicles in the ovaries, in which the development and growth of the egg occurs monthly until the moment of ovulation, when the follicle membranes rupture and the female reproductive cell is released into the abdominal cavity.
Until the moment of ovulation, the egg is reliably protected from external influences by the strong walls of the follicle and a special liquid.
Normally, under natural conditions, only one, rarely two dominant follicles with a full-fledged egg mature in a woman’s ovaries. This number of eggs is not enough to complete an IVF program. Therefore, a woman is prescribed artificial hormonal stimulation of the ovaries in order to obtain a large number of eggs suitable for fertilization.
Important. According to statistics, IVF with hormonal stimulation gives the greatest chance of success the first time - up to 45% of protocols result in pregnancy.
Why is laparoscopy needed before IVF?
Carrying out laparoscopy significantly increases the chance of successful completion of in vitro fertilization. Using this type of diagnosis, the causes leading to infertility are identified. Some of them are not visible on pelvic ultrasound. One of the advantages of laparoscopic intervention is the ability to remove etiological factors during the examination.
The question of whether the intervention is mandatory arises for all women. Experts believe that laparoscopy before IVF increases the number of positive results after the protocol.
Condition of the fallopian tubes
Many chronic gynecological diseases lead to obstruction of the fallopian tubes. Because of this, the fertilized egg cannot penetrate the uterine cavity for further attachment. The most common causes of changes in the condition of the fallopian tubes are:
- Spikes. Occurs after inflammation.
- The presence of pathological fluid in the cavity of the fallopian tubes.
- Deformation of the pipe structure, causing complete or partial obstruction.
- Increased permeability of the walls of the fallopian tubes.
Diagnostic laparoscopy will help identify these conditions. In parallel with the study, the woman’s ability to conceive and bear a child is assessed. When determining the adhesive process in the cavity of the fallopian tubes, surgical intervention is prescribed, the purpose of which is to restore their patency. After treatment, time is required for the body to recover before IVF. On average it takes 3-4 months.
Endometriosis
Pathological proliferation of endometrioid tissue is often detected in women of reproductive age. There is an opinion that therapy for endometriosis does not increase the success of the IVF protocol. However, with natural conception, treatment of endometriosis is a prerequisite for pregnancy.
Laparoscopy allows you to determine the presence of damage to the endometrium of the uterus. The pathology can exist for a long time without any clinical manifestations.
A dangerous complication of endometriosis is the tendency for pathological tissue to spread to nearby organs. The bladder, intestines, and other pelvic organs are similarly affected. The body must be given time to recover after treatment. After 3 months, you are allowed to enter into the in vitro fertilization protocol.
Cyst removal
Cysts interfere with the possibility of successful in vitro fertilization. Laparoscopic surgery is prescribed to remove the formation and restore patency of the fallopian tubes.
Complete restoration of ovarian function is possible. In this case, an IVF protocol is not required, and pregnancy occurs naturally. However, if it is necessary to remove the cyst along with the ovaries, the only way to conceive is in vitro fertilization.
Polycystic ovary syndrome
Characterized by dysfunction of the ovaries. The process of ovulation is absent, leading to infertility.
Using the laparoscopic method, part of the ovary is removed or incisions are made on its capsule. In a similar way, the functional ability of the organ is restored, but for a short period of time. In vitro fertilization is indicated 3 months after laparoscopy.
Uterine fibroids
It is one of the benign neoplasms of the pelvic organs. The presence of myomatous nodes changes the shape of the uterus, leading to disruption of blood microcirculation in the organ.
Performing IVF in the presence of this disease is not advisable, since the deformed uterus is not suitable for bearing a child. Myomatous nodes are removed using laparoscopic surgery. The recovery period takes about 8 months. After this, an IVF protocol can be carried out.
Basal temperature from A to Z
Good afternoon everyone! I've been thinking about creating this topic for a long time and finally got around to it. Apparently I will write a lot, forgive me, this is very important for me! My situation is this: my husband and I have been actively planning for more than 1.5 years; before that, we were using birth control interrupted for 1.5 years. With my first husband, 7 years ago, we didn’t use any protection at all, also for two years, we didn’t plan, but we didn’t use any protection either. My cycles have always been irregular, jumping from 30 to 60 days as they please. At one time, I took OK as prescribed by a doctor to normalize the cycle several times, the last time 4 years ago, the cycle did not normalize. I’ve been planning for the last 2-2.5 years, we normalized the microflora, we started trying for about 1.5 years now. I’ve been taking douf for almost a year, M is on it like a clock, without it the cycle jumped, but the last two have been 30-32 days, which is already an achievement for me. Last summer I had an HSG, the tubes are tortuous but passable, my husband’s SG is pathological 86%, mobility is slightly below normal, my doctor says that it’s more than enough for pregnancy, 2 cycles of clost stimulation, O yes, B no, trying to get pregnant after clost There is also no way to maintain the effect. Hormones - LH and FSH are elevated, but according to ultrasound there is no classic picture of PCOS, there are deviations, but not classic PCOS, androgens are not elevated. And now my G says that it is necessary to do laparotomy and cauterization of the ovaries... I, in principle, already wanted to ask her myself, but then she says that since my LH and FSH are elevated, my ovaries are slightly enlarged, problems with O and the cycle are not If you haven’t had B once in your entire life, even on stimulation, then it happens that the membrane on the ovaries is too dense and it does not allow the ovulated egg to leave the ovary. There is no other way to see this, and this is understandable... So she offers a diagnostic and treatment lapar with cauterization... After this, the effect is 5-6 months, if not zaB, then then IVF. On Tuesday I turned 30 years old... And now I’ve probably been nurturing the thought in my head for about a month now - maybe I should immediately save up for IVF? The price of the issue is as follows: a lapar with anesthesia and a hospital will cost about 50-70 thousand, IVF, as I understand it, 150-200 thousand. We don’t have either money just lying around, due to renovations from scratch in a new building, we are already in debt and loans, it’s not easy to save up even for lapara. That’s why I’m tormented by doubts: maybe I shouldn’t waste my time on lapara. I will now write the pros and cons of IVF and lapar in our case, which have formed in my head. I would like to hear your opinions, additions, and advice. And also the opinions of those who have gone through IVF or laparotomy or both, for whom what helped, for what diagnoses. In general, I collect.
LAPAROSCOPY with cauterization of the ovaries: + they will look inside the endometrium, uterus, tubes, separate adhesions, if any + incisions on the ovaries for the release of the egg + the opportunity to get pregnant naturally + lower cost - it is still a small, but surgical intervention - the likelihood of formation adhesions after surgery - the probability of a healthy couple getting pregnant in each cycle is 20-25%, we are not a healthy couple, judging by my husband’s SG and my hormone cycles, which means ours is even lower - my twisted tubes are scary, I’m afraid that they can lead to VD - a large percentage of pathological sperm in the husband, 86% is the upper limit of the norm, I am afraid that this increases the chance of a miscarriage or ST
IVF: + the procedure is not aimed at trying to overcome infertility, but at trying to get pregnant + the chance of pregnancy is 30-40% according to statistics + the chance of giving birth to twins (for me this is a plus, since I would like it and it’s already been too many years, it’s scary), but it also a minus in its own way, since it is more difficult to bear + the probability of VD is much lower + with our SG it is most likely ICSI, which means the sperm will somehow be selected and the healthiest ones will be chosen, which will greatly reduce the likelihood of V and ST - a rather strong hormonal shock according to the body - the likelihood of getting OHSS - it may well not work out on the first try - quite high cost - a more complicated pregnancy
This is of course not everything, but what I managed to accumulate. I just can’t decide... I have one thought, then another. I am seen at the Center for Obstetrics and Gynecology on Oparina for a fee. I haven’t been going to regular residential complexes for a long time, I don’t come across normal doctors there. It’s clear that I won’t make this decision right away... On Monday I made an appointment with G at the residential complex, which I’ve never visited. I will take her all the examinations done over the last 2 years, I want to hear her opinion. Then my husband will take the SG again and go to the andrologist, let's see what he says. I’ll go to G, who I’m seeing, and ask her opinion about the advisability of lapara, or maybe IVF right away. But I’m already sick of this uncertainty... Therefore, I’m really looking forward to your opinions, advice, personal experience, real-life examples... Thanks in advance to those who read to the end and helped with advice!
How long does it take to do IVF after laparoscopy?
The question “how long does it take to do IVF after laparoscopy” is relevant for all women planning an in vitro fertilization protocol. The timing depends on the pathology for which the intervention was performed.
The body needs to recover after surgery. On average, this period takes up to 3 months. However, for some conditions, recovery may take about 6 months. Laparoscopy before IVF can increase the chance of pregnancy after the first embryo transfer.
When to do repeat IVF
Many patients are interested in the question: when can repeat IVF be done after failure ? After all, we know that the first attempt is not always successful, unfortunately. There are no strict recommendations, but as clinical experience shows, it is better to skip at least 2 menstrual cycles . For what? After an unsuccessful IVF protocol has ended, the body needs time to recover.
Firstly, the ovaries need to “calm down”, as they were forced to work intensively. Often after IVF we observe corpus luteum cysts in the ovaries, which do not immediately disappear, so it takes time to recover, because the presence of cysts in the ovaries is a contraindication for starting stimulation.
Secondly, the body after IVF received a good dose of hormonal drugs, this is also a kind of stress, so it needs a pause to recover.
The menstrual cycle should be restored. Usually, after unsuccessful IVF, the doctor may prescribe a more in-depth examination that goes beyond the scope of the examination of the ART order, and examination and treatment adjustment also require time. Read about the number of attempts in the article: How many attempts can there be with IVF?
Types of laparoscopy
Depending on the purpose for which laparoscopy is performed, several types of intervention are distinguished. These include:
- Diagnostic. It is prescribed to clarify the diagnosis if it has not been possible to determine it in other ways. The advantage of diagnostic laparoscopy is the ability to convert it to surgical laparoscopy.
- Surgical. It is the preferred method of treating many pathological conditions. Using a laparoscope, cysts, neoplasms, adhesions of the fallopian tubes, and myomatous nodes are removed. Surgical laparoscopy allows you to collect material for biopsy.
- Test. It is carried out to evaluate the results after a previously performed laparoscopy.
- Mini-laparoscopy. Method of choice before planned in vitro fertilization. During a mini-laparoscopy, incisions are made that leave no scars. Diagnostic examination or treatment of pathological conditions is performed in a similar manner.
Possible complications after the procedure
The hope for successful IVF after laparoscopy may not be realized for several months after the minimally invasive intervention. Despite the fact that for most patients the likelihood of becoming pregnant after the intervention increases by 1.5-2 times, some women still experience difficulties conceiving, since the causes of infertility have not been completely eliminated. The share of such unsuccessful operations is low - about 1%.
Unfortunately, doctors do not exclude the risk of complications, including those that arise as a result of the use of anesthesia or medical procedures. They are divided into three groups:
- Arising during the intervention. These include perforation of organs and bleeding. These problems are eliminated as part of the operation or require more serious interventions, for example, abdominal surgery (laparotomy). In the latter case, artificial conception is postponed to a later date (usually 9-12 months) until the walls of the organs are completely restored.
- Occurring on the first day after the procedure. These include bleeding, infection of the reproductive organs, and vascular thrombosis in the surgical field. If the doctor detects the presence of inflammatory processes, the woman is prescribed a course of antibiotics and physical therapy. In addition, many women experience digestive problems on the first day after surgery, which can be eliminated by following a diet and moderate physical activity.
- Distant, occurring several weeks after the intervention. These include the formation of adhesions of the wall of the uterus and fallopian tubes. Such consequences are typical for the removal of extensive foci of endometriosis inside the uterus, as a result of which large growths form on its walls, or they fuse together. Such pathologies are eliminated through repeated intervention.
Despite the abundance of possible problems, laparoscopy before IVF ends with them only in 2-5% of cases. Careful preparation for surgery and compliance with all, even minor, rules during recovery after the intervention help reduce the risk of their occurrence.
Laparoscopy capabilities
Laparoscopic intervention can be performed for both diagnostic and therapeutic purposes. Using this type of research, it is possible to identify pathological conditions that are not diagnosed by other methods.
The advantage of laparoscopy is the ability to observe changes in the pelvic organs in real time through the monitor screen. Indications for the study are the following pathologies:
Infertility of any origin. Laparoscopy allows you to identify causes that were not identified by other diagnostic methods.
- Assessment of the condition of the fallopian tubes. Diseases leading to their obstruction are excluded.
- Oncological formations. Laparoscopy is considered a mandatory diagnostic method for suspected ovarian cancer.
- Inflammatory diseases of the pelvic organs. The study determines the presence of endometriosis and myomatous nodes.
- Ectopic pregnancy. Suspicion of abnormal fetal development is confirmed laparoscopically.
Diagnostic manipulation can turn into surgery when the following conditions are detected:
- Violation of the patency of the fallopian tubes. The cause of the pathology is adhesions, cysts and other formations.
- Uterine fibroids. Myomatous nodes are removed using the laparoscopic method. At the same time, it is possible to preserve the organ and the possibility of further pregnancy.
- Ovarian pathology. The most common cause of infertility is polycystic disease. Laparoscopy allows you to remove part of the ovary or puncture the organ capsule. In addition, cysts and other ovarian tumors are excised.
Preparing for surgery
To ensure that female reproductive cells - oocytes - are as healthy as possible at the time of extraction from the ovaries and are not exposed to the harmful effects of various factors, a woman must adhere to a number of recommendations when entering the IVF program:
| Strict compliance with all doctor's instructions | In case of ovarian hyperstimulation, take medications according to the prescribed regimen, follow the schedule for donating blood for hormones and control ultrasound. |
| Proper nutrition | Complete balanced nutrition with essential nutrients: proteins, fats, carbohydrates, vitamins, minerals. Refusal of foods that cause increased gas formation (legumes, cabbage, baked goods, sweets), semi-finished products, canned food, products containing large amounts of preservatives, dyes, and flavor enhancers. Drinks containing caffeine are limited: coffee, tea. |
| Bad habits | A categorical ban on smoking and the consumption of any type of alcoholic beverages. |
| Compliance with drinking regime | Taking the optimal amount of fluid is from 2 to 2.5 liters per day. |
| Drugs | Taking any medications or vitamins is allowed only with the permission of a doctor. |
| Compliance with the work and rest schedule | Lack of excessive physical and emotional stress, healthy sleep, sufficient exposure to fresh air. |
| Sun and water treatments. | Visits to baths, saunas, solariums, and excessive exposure to the sun are contraindicated. |
| Prevention of infections | Carrying out preventive measures to prevent infections with infectious diseases. |
Ovarian puncture, although minimally invasive, is an operation, so before performing it, the following examinations and tests are prescribed:
- Clinical blood test with coagulogram.
- Biochemistry of blood.
- General urine analysis.
- Smear on the flora of the vagina, cervical canal.
- Testing for sexually transmitted diseases.
- Ultrasound of the pelvic organs.
- ECG.
- Examination by a therapist.
The operation is performed on an empty stomach, the last meal is allowed 12 hours before the procedure, liquids 4 hours before.
On the eve of the procedure, you should cleanse the intestines naturally or with the help of enemas and laxatives.
Shave the hair on the forehead and genital area.
Immediately before the procedure, you should urinate and thoroughly wash the external genital area.
A woman comes to the procedure without decorative cosmetics, and there should also be no nail polish.
If the patient wears contact lenses or dentures, they must be removed before surgery.
You need to take with you a change of shoes, a shirt (cotton), and a robe.
Benefits of laparoscopy
Over the past few years, laparoscopy has become one of the most popular types of diagnostics and surgical intervention. This is due to the many advantages of the method. The main ones include:
- Possibility of performing surgical intervention during diagnostics. Cysts, neoplasms, adhesions and other pathological conditions that prevent IVF are removed.
- Reduced volume of operational access. The difference between laparoscopy and abdominal surgery is that a minimum number of incisions are made to gain access to the affected organ.
- Short recovery period. Due to the reduction in the number of injured tissues, the rehabilitation process proceeds much faster.
- Reducing the number of postoperative complications.
- Cosmetic effect. This advantage is especially important for women. Small incisions heal with the formation of invisible scars.
- Organ preservation. Laparoscopy is performed under constant monitoring of the operation via a video monitor. In this way, precise access to the pathological focus is achieved and the ability to remove it while preserving the organ is achieved.
These advantages allow us to consider laparoscopy as the method of choice if it is necessary to perform surgical intervention before in vitro fertilization.
Procedure
Laparoscopy before IVF is a surgical procedure, but it does not leave stitches and does not require long-term rehabilitation. The doctor carries out all manipulations through several small incisions into which a laparoscope and other necessary instruments are inserted.
The procedure is performed under local anesthesia and general anesthesia, so it does not cause any inconvenience to the patient. The duration of laparoscopy ranges from 30 minutes to 1.5-2 hours, depending on the need for treatment.
After the operation, the patient is recommended to stay in the clinic for another two days, and antibiotics are prescribed to prevent infection. If a disease is detected, the doctor prescribes drugs to treat it.
The main advantage of laparoscopy over IVF is its high information content. Doctors are able to examine in detail all the pelvic organs and detect abnormalities. The disadvantage of the procedure is the need for general anesthesia.
How does pregnancy proceed after laparoscopy?
If all the deadlines allotted for the recovery period after laparoscopy are observed, IVF proceeds without complications. In case of a negative protocol result, laparoscopic intervention is not considered as the main reason for failure. Lack of pregnancy may occur due to other chronic diseases of the pelvic organs.
Repeated in vitro fertilization increases the chance of successful completion of the protocol. Experts note that the course of pregnancy after laparoscopy is no different from natural pregnancy.
Varieties
Before in vitro fertilization, laparoscopy is prescribed for various purposes. Its types according to purpose:
- diagnostic – identifying the reasons for the lack of natural pregnancy,
- therapeutic – treatment of pathologies of the uterus, its tubes and ovaries,
- control – checking the condition of the genital organs after the previous intervention,
- mini-operation - characterized by the minimum size of punctures and the subtlety of instruments for performing manipulations.
The most common types of laparoscopy are diagnostic and therapeutic. A control intervention before IVF is carried out after eliminating chronic diseases or pathologies with a high risk of relapse.
Are there any differences from the procedure without pathology?
The presence or absence of fallopian tubes does not have a significant impact on the IVF protocol. Some reproductive specialists note an increase in the chances of pregnancy after laparoscopy.
This is due to the following circumstances:
- Removal of the source of infection. Chronic diseases are a common cause of infertility. These include endometriosis, adhesive disease of the fallopian tubes, the presence of myomatous nodes and other gynecological pathologies. Excision of the etiological factor increases the chances of obtaining a positive result after IVF.
- Excluding the possibility of developing an ectopic pregnancy. The percentage of this complication is not high. However, if there is pathology of the fallopian tubes, the chance increases. The fertilized egg does not enter the uterine cavity and attaches to the fallopian tubes. An ectopic pregnancy is an indication for emergency surgery.
The in vitro fertilization protocol after removal of the fallopian tubes and if they are present will consist of the following steps:
- Diagnostic study. It is carried out for the timely detection of chronic diseases and the appointment of appropriate treatment.
- Ovarian stimulation. To obtain more mature eggs, hormonal stimulation is performed.
- Determining the time of follicle enlargement using ultrasound diagnostics.
- Follicle puncture. During the manipulation, mature oocytes are collected for further fertilization.
- Fertilization of an egg using the sperm of a partner or donor. As a result, an embryo is formed. The resulting embryos are examined to identify the most viable ones.
- Transfer of embryos into the uterine cavity. The final stage of the IVF protocol. It is recommended to take a pregnancy test 14 days after implantation to determine the outcome of the procedure.
Method capabilities
In addition to diagnostics, laparoscopy before IVF allows you to get rid of:
- From chronic infectious foci in the pelvic cavity.
Any foci of inflammation in the pelvis interfere with the implantation of embryos and contribute to their rejection. This is a confirmed, irrefutable fact.
Most often, the cause of inflammation is irreversible changes in the fallopian tubes. If there are such changes, then the question of removing them (one or both) definitely becomes a question. Adhesions in the tube contribute to the accumulation of fluid inside the organ - the outflow is disrupted or stops altogether. This condition is called hydrosalpinx and is accompanied by subacute inflammation. Pathogenic flora and its metabolic products have a detrimental effect on the implantation of the embryo into the wall of the uterus, contributing to its rejection or the onset of ectopic pregnancy. To get rid of a chronic infection, surgical removal of the lesion is required with further administration of antimicrobial therapy.
Some will say that time is running out and the ovarian reserve is decreasing. But, you must agree that refusing laparoscopy for provoked fallopian tubes is not the best option for preparing for the protocol.
One of the possibilities of laparoscopy is to perform reconstruction of the fallopian tubes and create conditions for drainage by separating the adhesions.
- From adhesions.
The long-term consequences of abdominal surgery (any) on the abdominal and pelvic organs and peritonitis is the adhesive process. In the case we are interested in, quite often a degree of spread of the adhesive process occurs in which the pelvic organs (intestines, uterus, bladder, ovaries, both tubes) turn into a conglomerate glued together by adhesions and are in a case of scar tissue. For IVF, this is an extremely unfavorable condition, since puncture of the follicles is difficult and often simply impossible. Laparoscopy before IVF allows you to “free” the ovaries and make them accessible for puncture.
- From foci of endometriosis.
Endometrioid formations are a very common cause of infertility, sometimes asymptomatic. At the same time, endometrioid cysts interfere with the full maturation of eggs and implantation due to the production of substances that inhibit these processes. Carrying out laparoscopy before IVF allows for the surgical removal of endometriotic formations, thereby helping to restore reproductive health and relieve pain. There are frequent cases when, after removal of pathological foci, a natural pregnancy occurs, and women sometimes do not even suspect the existence of endometriosis and go for artificial insemination.
The advisability of removing endometrioid cysts before the protocol remains a controversial issue today. Leading practitioners are inclined to believe that laparoscopy before IVF is necessary to get rid of endometriotic lesions. The main thing is that the operation should be performed by professionals with sufficient experience in the surgical treatment of endometriomas.
- From myomatous nodes.
Benign tumor formations formed in the muscular layer of the uterus deform its cavity. A direct connection between uterine deformation and implantation disorders has been scientifically proven. This happens for a number of reasons.
Among them:
- endometrial damage;
- atrophy of areas of the uterine mucosa;
- inflammation;
- circulatory disorders.
The listed symptoms are a consequence of deformation of the uterus by myomatous nodes. But the presence of nodes itself does not affect the positive outcome of IVF. For patients with this pathology, laparoscopy before IVF is highly desirable. Thus, the implantation rate with the “correct” shape of the uterus is 30%, and with a deformed uterine cavity - slightly less than 9%. These numbers eloquently answer: “Do patients with myomatous nodes need laparoscopy before IVF?”
Preparing a man for the IVF procedure
As you know, in vitro fertilization is used in cases where, due to health problems of the woman, man or both partners, the couple cannot conceive a child naturally.
During in vitro fertilization, a man performs the same role as during natural conception. The day for conception is determined by the woman’s menstrual cycle, therefore sperm collection is carried out on a strictly defined day. As a rule, to extract seminal fluid, a man simply masturbates, but, if necessary, various surgical methods can be used: testicular biopsy, aspiration of epididymal contents, etc. The only contraindication for IVF is the presence of hepatitis B, HIV and other hereditary diseases that can harm life and health baby.
No matter how frivolous it may seem, the correct psychological attitude is no less important than the state of health. If a man is calm and open-minded about the IVF procedure, then he will encounter only minimal problems in the process. It is important to understand: how serious are a man’s intentions to have a child? Will a man be able to support his wife throughout the entire period? Doesn't the in vitro fertilization procedure run counter to a man's worldview and religion? Will a man be able to afford the IVF procedure financially and emotionally? The process should be started only if the man can confidently answer positively to all questions.
Preparing for IVF for men
For men , preparing for the IVF procedure is not much different from preparing for natural conception. You just have to follow these recommendations, and it’s not difficult at all:
- Forget about alcohol, cigarettes and other bad habits. Now you have strong motivation for this, because the life and health of your child is at stake. During the period before conception, it is unacceptable to use drugs, alcohol, or smoke.
- Try not to overheat. Normal viable sperm develop at temperatures no higher than 34°C. Therefore, forget about saunas, steam baths and even hot baths. IVF is an extremely expensive proposition, so don’t neglect advice like this, which will increase your chances of becoming parents on the first try. In addition, you should spend less time driving.
- Stick to moderate physical activity. 2-3 months before the procedure, avoid excessive physical stress, such as strength sports, gym classes, and heavy physical work. But with all this, a completely sedentary lifestyle must be diluted with daily leisurely walks of several kilometers.
- Make sure the underwear you wear is comfortable. For normal sperm maturation, underwear that is as spacious as possible is best. From a scientific point of view, this approach, however, has not yet been justified, but just in case, refuse uncomfortable and tight underwear.
- Monitor the frequency of sexual intercourse. The best option would be to have sexual intercourse for 2-3 months before the procedure, once every three days, not more often. In this situation, the quality of sperm will not suffer, and the sperm themselves will