Thyrotropin (thyrotropin, TSH) is a pituitary hormone that stimulates the thyroid gland. It maintains normal levels of thyroid hormones - triiodothyronine (T3) and thyroxine (T4). Low TSH during pregnancy indicates increased activity of hormones in the blood. Fluctuations in hormonal levels are caused by natural changes in the body during pregnancy, but can also indicate pathologies of the thyroid gland or hypothalamic-pituitary system.
Functions in the body
Thyroid-stimulating hormone (TSH) is necessary for the proper functioning of the thyroid gland. It stimulates the production of thyroxine (T3) and triiodothyronine (T4).
Thyroid-stimulating hormone is responsible for the following functions of the human body:
- metabolic processes of fats, proteins and carbohydrates;
- growth and formation of the human body;
- functioning of the digestive system;
- influence on reproductive function;
- clear vision, good hearing;
- work of the cardiovascular system.
TSH also maintains a person's mood by influencing mental functions. Takes part in the synthesis of protein and retinol. It is important that the norm during pregnancy does not exceed the specified data, since deviations provoke serious illnesses.
What is TSH and its role during pregnancy
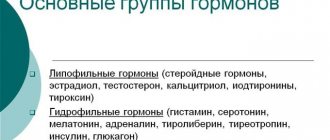
The body develops under the influence of hormones - groups of biologically active substances that are formed in the endocrine glands, as well as in the kidneys, stomach, intestines and other organs. From the place of synthesis, hormones are carried by the blood and regulate biochemical processes in vital systems. It is curious that there are very few hormones in the blood, but these substances, without exaggeration, control the body.
TSH, thyroid-stimulating hormone (another name is thyrotropin), is produced in the anterior lobe of the appendage of the brain - the pituitary gland. The main task of TSH is to control the functioning of the thyroid gland. This butterfly-shaped endocrine gland is located under the larynx and serves as a reservoir for storing iodine.
The size of the thyroid gland is modest - two by four centimeters - but the gland plays a vital role in the functioning of the human body
What happens is this: thyrotropin binds to certain receptors on the surface of the thyroid gland and stimulates the production of two iodine-containing hormones of the gland - T4 (thyroxine) and T3 (triiodothyronine). As a result, all three hormones are responsible in the body for:
- proper metabolism;
- synthesis of nucleic acids, as well as erythrocytes - red blood cells;
- glucose production;
- work of the heart and blood vessels;
- transmission of impulses between neurons in the brain;
- respiratory system support;
- normal functioning of the digestive tract;
- coordinated functioning of the genitourinary system;
- mental condition.
The mutual influence of the three hormones is sometimes called a “swing”: the more TSH is produced, the less T4 and T3 become - and vice versa. The reason is that TSH stimulates the production of two other thyroid hormones until their high levels begin to inhibit the production of TSH itself in the pituitary gland. But gradually thyroxine and triiodothyronine are absorbed in the tissues, the level of both decreases again - which means the secretion of thyrotropin is restored.
It is enough to measure the amount of TSH in the body to find out whether the thyroid gland is in order or not, what pathologies are present.
An analysis of the level of thyroid-stimulating hormone in the blood is prescribed to every expectant mother who is registered at the antenatal clinic. If a woman has been diagnosed with thyroid-related complications during previous pregnancies, TSH levels should be carefully monitored before becoming pregnant again.
Too high or too low hormone production signals that the endocrine system is stalling. This condition triggers negative and often irreversible processes in the body; this leads to health problems, and in severe cases, fetal death. The main consequences are:
- pathologies of the nervous system of the unborn child;
- gestosis or late toxicosis in the mother, which threatens the death of the fetus in the womb; sometimes the woman herself falls into a coma (eclampsia) and dies;
- placental abruption - if the temporary organ formed in the 2nd trimester detaches more than half, the fetus will die;
- intrauterine growth retardation; as a result, the child is at risk of mental retardation after birth;
- miscarriage;
- the birth of a baby with thyroid pathology.
If a woman is trying unsuccessfully to become pregnant, a TSH test is also prescribed; Disturbances in the functioning of the endocrine system provoke abnormal metabolism in the ovaries. In this case, a pelvic ultrasound will detect a lack of egg and follicle, as well as insufficient development of the corpus luteum (the temporary gland that synthesizes the “pregnancy hormone” progesterone).
How and under what conditions is it produced?
The anterior lobe of the pituitary gland is responsible for the production of thyroid-stimulating hormone. TSH controls the functioning of the thyroid gland and other systems in the human body. Due to the production of thyroxine and triiodothyronine, the activity of the heart, blood vessels, digestive and reproductive systems is carried out. Hormones also support material metabolism.
When an embryo is conceived, the body of the expectant mother begins to secrete a special hormone called hCG (human chorionic gonadotropin). It affects not only the entire woman’s body, but also activates increased production of thyroid-stimulating hormone.
The embryo is unable to produce thyroid hormones on its own; it takes them from the mother. There is an excess of thyroxine in a woman’s body.
At the same time, the level of thyroid-stimulating hormone decreases sharply. As the fetus develops, the parameters will be restored, since the baby develops its own thyroid gland and it begins to produce hormones. Therefore, the amount of TSH in a woman’s body is constantly changing throughout the entire period of bearing a child.
If women have elevated TSH during pregnancy: how dangerous is it for the fetus?
An altered level of thyrotropin in relation to its normal value during any trimester of pregnancy is an alarming sign.
I trimester
Until 8-9 weeks, the fetal body cannot independently produce thyroid hormones.
Until this time, he is completely dependent on his mother’s endocrine system. Therefore, even minor deviations in the activity of the maternal gland negatively affect the health of the unborn baby. With a deficiency or excess of TSH in the first 3 months, persistent irreversible disturbances occur in the process of formation of children's organs. Also, your own thyroid gland will develop incorrectly.
II trimester
If by the end of the first and beginning of the second trimester the hormone value does not approach normal, the likelihood of a successful pregnancy outcome decreases significantly.
At this time the following are observed:
- placental abruption;
- miscarriage;
- intrauterine fetal death;
- cholecystectomy;
- adrenal dysfunction;
- persistent psycho-somatic disorders;
- severe gestosis.
III trimester
If it is possible to bring a pregnancy to the desired term with TSH abnormalities, there is always the danger of giving birth to a child with severe developmental defects.
When the thyrotropin level corresponds to the norm in both trimesters and increases in the last trimester, the likelihood of developing defective conditions in the baby is minimal. But the likelihood of incorrect delivery increases.
Considering how dangerous a deviation in the value of this hormone is, a woman needs to constantly monitor its levels, especially when there is a predisposition to problems with it.
Indicator table is normal
During pregnancy, a woman's body goes through numerous changes. The level of thyroid-stimulating hormone is constantly changing.
There are certain norms, taking into account the semester of pregnancy:
| Period | TSH level (mIU/l) |
| 1-13 weeks | 0,1-2,5 |
| 14-27 weeks | 0,2-3,0 |
| 28-40 weeks | 0,2-3,5 |
Significant deviations are a reason to undergo a comprehensive examination to assess the functioning of the thyroid gland. A pregnant woman is prescribed a TSH, T3 and T4 test.
How to treat low TSH in the blood
If TSH is below normal during pregnancy, patients are referred for further examination. To identify the causes of endocrine disorders, the following are prescribed:
- analysis for T3 and T4;
- Ultrasound of the thyroid gland;
- TPO antibody test;
- clinical blood test.
In the case of hyperthyroidism, the basis of therapy is antithyroid drugs - Mercazolil, Tyrosol, Propylthiouracil, Metizol. Additionally, beta blockers (Timolol, Nebivolol) are used, which eliminate arrhythmia, tachycardia and hand tremor.
If there is a lack of TSH due to pathologies of the brain and adenohypophysis, hormone replacement therapy (HRT) is performed. To normalize the level of T3 and T4 in the blood, L-Thyroxine, Bagotirox, Eutirox are used.
Symptoms of increase and decrease
Pathological changes provoke the appearance of characteristic signs in a woman during pregnancy. It is important not to ignore the body’s signals, but to consult a doctor in a timely manner.
TSH (the norm during pregnancy indicates the normal course of all processes in a woman’s body) is low or high and is accompanied by characteristic clinical signs.
Characteristic features:
| Name | Signs |
| Elevated TSH |
|
| Low TSH |
|
In any situation, it is important for a pregnant woman to promptly consult an obstetrician-gynecologist. The specialist will prescribe a medical examination and select the safest treatment.
Is there a connection between conception and the TSH hormone?
Normal TSH during pregnancy
significantly different from that which is typical for a woman in a normal state. For conception, this indicator must be strictly within certain limits - from 1.5 to 2.5 mU/l. If the actual results differ significantly from the norm, pregnancy may not occur at all. Impaired TSH secretion can cause spontaneous miscarriage in the early stages of pregnancy.
If a couple cannot conceive a child for a long time, they should consult a doctor. Hormones are often the cause. TSH is not in last place on the list of “responsible” people.
Immediately after conception, the concentration of TSH decreases sharply. But it should still remain within 0.4–4 mU/l for the gestation process to be normal. Often, even by the state of hormones, it is possible to diagnose conception, when other methods remain uninformative for some time.
TSH is an important hormone of the endocrine system, which partly regulates both the process of conception and childbearing. That is why it is important to find out what standards are established for the first, second, third trimester of pregnancy.
Reasons for promotion and demotion
It is important to determine the underlying source of the pathological condition or disease, since changes in thyroid-stimulating hormone levels can have serious consequences for a pregnant woman.
There are certain factors that provoke a decrease or increase in TSH:
| Name | Causes |
| Low TSH |
|
| Elevated TSH |
|
There are also certain diseases that cause deviations in the level of thyroid-stimulating hormone:
| Name | Description |
| Transient thyrotoxicosis | The disease is diagnosed more often in the first trimester. Hormonal changes in the female body provoke increased secretory activity of the thyroid gland. The concentration of thyroid-stimulating hormone also changes. |
| Pathologies of the pituitary gland | A decrease in TSH occurs due to injury, autoimmune disorders, or as a result of the formation of a tumor of the adenohypophysis. |
| Toxic goiter | The pathological condition is characterized by active activity of the thyroid gland. Associated symptoms include increased sweating, bulging eyes, increased body temperature, and sudden weight loss. |
| Hyperthyroidism | Hormonal imbalances disrupt the functioning of the endocrine system. The result is a deficiency of the pituitary gland and increased activity of the thyroid gland. During the period of bearing a baby, hyperthyroidism is characterized by an excess of iodine in the body of the expectant mother. Autoimmune thyroiditis or ovarian teratomas also appear. |
An endocrinologist is involved in treatment and diagnosis. Therapy is also carried out under the supervision of an obstetrician-gynecologist. It is strictly forbidden to diagnose yourself and take medications on your own.
Functions and interpretation of TSH hormone indicators during pregnancy
Every woman who dreams of having a healthy baby must take responsibility for her health both throughout pregnancy and during its planning. This also applies to the control of hormonal levels, since the outcome of pregnancy and the correct formation of the fetus often depend on its indicators.
From the moment the egg is fertilized, the female body begins to undergo processes that rearrange the functioning of organs and their systems. These changes are aimed at ensuring the full progress of pregnancy and the appearance of a healthy baby. The functionality of the endocrine system also changes - the level of its hormones changes according to the trimesters. But due to a number of factors, this system may fail. Only by monitoring the saturation of the blood with the hormone TSH, the gynecologist-endocrinologist receives a detailed picture of the course of pregnancy.
Indications for the study
Testing for TSH levels during pregnancy is recommended for all expectant mothers. This is especially true for women who have had thyroid problems in the past. The same applies to pregnancies with an unfavorable outcome.
Experts recommend conducting an examination during pregnancy planning in order to prevent negative consequences or complications in the future.
There are certain indications for testing TSH levels:
- severe changes in a pregnant woman’s body weight;
- frequent constipation;
- constant fatigue;
- emotional outbursts;
- swelling of the upper and lower extremities;
- cardiopalmus;
- trembling of the upper limbs;
- causeless anxiety and restlessness;
- heart rhythm disturbance;
- hair loss;
- neck deformity.
In most cases, studies are carried out every 3 months. If there are serious indications or violations, diagnostics are prescribed more often. For each pregnant woman, everything is individual.
Thyroid-stimulating hormone is reduced during pregnancy - what does this mean?
A decrease in TSH levels can be easily determined by behavior. During pregnancy, a woman becomes nervous, aggressive, periodically becomes depressed, and loses weight before her eyes even with a good appetite.
She may suffer from severe headaches, high blood pressure, intestinal problems and fever.
Reasons that can cause a decline in TSH levels during pregnancy.
- Plummer's disease (benign thyroid tumor).
- Reduction, injury or disruption of the pituitary gland.
- Development of hyperthyroidism or thyrotoxicosis.
- Uncontrolled use of medications (cytostatics, corticosteroids, etc.) that affect the level of thyrotropin.
- Severe stress.
- Graves' disease (toxic goiter).
Donate blood from a vein
To establish an accurate diagnosis, the pregnant woman is prescribed additional tests and an ultrasound examination of the thyroid gland.
When treating low TSH, conservative therapy with the prescription of antithyroid drugs is used. When selecting a product, take into account weight, age, how the pregnancy progresses and the risk to the fetus.
Beta blockers are used to eliminate cardiovascular symptoms. The condition is monitored by ECG.
Why is low TSH dangerous?
If the test shows that thyrotropin during pregnancy is below normal, then hyperthyroidism or thyrotoxicosis is most often diagnosed for this condition. These are very serious pathologies that require urgent medical intervention.
What complications can arise with decreased TSH during pregnancy in the mother and fetus:
- early spontaneous abortion;
- hypoxia (lack of oxygen) and developmental delay in the baby;
- the appearance of gestosis;
- premature birth;
- placental abruption;
- anemia;
- stillbirth.
The consequences can be dire
In 3% of cases against the background of thyrotoxicosis during pregnancy, antibodies penetrate the placenta. As a result, the baby develops intrauterine and then neonatal toxic goiter.
How to determine
Diagnostics is necessary to make an accurate diagnosis. It is important to determine the underlying disease or reason behind which the level of thyroid-stimulating hormone has decreased or increased.
TSH (the norm during pregnancy indicates the correct functioning of all internal organs and systems in the body of the expectant mother) diagnosis involves carrying out the tests given in the table.
| Name | Description |
| Analysis of T3, T4, TSH and antibodies to TPO | A comprehensive study that can be used to evaluate the functioning of the thyroid gland. Also detect serious diseases at an early stage. |
| Ultrasound examination of the thyroid gland (ultrasound) | The specialist evaluates the size of the organ, its location, structure, structure. |
Scintigraphy and computed tomography (CT) are contraindicated during pregnancy because they cause radiation exposure.
How to reduce the risks of TSH deviation from normal
Hyperthyroidism caused by hereditary predisposition or hormonal disorders is difficult to prevent. It is important to monitor your own health, hormonal levels, and go to the doctor in time for medications.
Don’t neglect the standard advice given to pregnant women:
- Lead a healthy lifestyle if possible, stop smoking and alcohol;
- eat right - less fatty and sweet foods, more foods rich in proteins; seaweed, red vegetables, persimmons, porridge, introduced by the expectant mother into the diet, will help avoid iodine deficiency, and therefore the danger of hypothyroidism;
- eliminate nervous tension and stress from life; stay calm and positive in any situation.
Preparing and conducting analysis
To obtain the most accurate results, a pregnant woman is recommended to follow simple rules before testing:
- Blood is taken from the antecubital vein in the morning on an empty stomach, when the level of thyroid-stimulating hormone is maximum.
- Before the test, do not eat anything for 8 hours. It is also not recommended to drink mineral water with dyes or flavors.
- Before the tests, exclude fried and fatty foods from your diet 2 days before testing.
- You cannot drink alcoholic beverages.
- Immediately 1.5-2 hours before blood sampling, you should be in a calm emotional state and completely refrain from physical activity.
The test results are negatively affected by hormonal drugs and iodine-containing drugs. They must be put aside a month before the scheduled analysis.
How to take a TSH test: rules
A blood test for this hormone is one of the main laboratory tests. To obtain objective results, the analysis must be performed correctly, i.e.:
- 3-4 days before the analysis, drinking alcohol and smoking is prohibited.
- Avoid any physical activity for the same period.
- Blood sampling is done on an empty stomach from a vein in the morning.
- To monitor fluctuations in hormone concentrations, blood is taken at one time.
In practice, gynecologists prescribe such an analysis at 6-7 weeks, and then the blood is checked once every trimester (when there is no hyperthyroidism or hypothyroidism). But the best option, in their opinion, is a blood test before pregnancy. This approach will help to detect deviations in time and carry out corrective therapy.
Decoding the results
A woman will not be able to establish a diagnosis and decipher test results on her own. A qualified endocrinologist will help her. The specialist will tell you what the deviations indicate and what to do to restore the functioning of the thyroid gland.
Each clinic uses specific equipment, which may cause test results to vary. Therefore, it is necessary to visit an endocrinologist.
Considering the patient’s age, there are certain standards:
| Person's age | TSH level (mIU/l) |
| Newborns | 1,1-17,0 |
| Up to 2.5 months | 0,6-10,0 |
| 2.5 – 14 months | 0,4-7,0 |
| 14 months – 5 years | 0,4-6,0 |
| 5 – 14 years | 0,4-5,0 |
| 14 years old - adults | 0,4-4,0 |
In women carrying a child, the concentration of thyroid-stimulating hormone is 0.2-3.5 mIU/l. Deviations indicate minor changes in the body of the expectant mother or the development of a serious pathology. Medical tests will help you accurately establish the diagnosis.
Why does TSH increase and what does it mean?
A high level of the hormone thyrotropin indicates the development of hypothyroidism. If left untreated, this condition can seriously affect the mother and child.
Reasons for increased TSH levels during pregnancy.
- Tumor or adenoma of the pituitary gland.
- Adrenal gland dysfunction.
- Complex psychosomatic pathologies of severe origin.
- Failure of regulation or resistance to thyrotropin.
- Late toxicosis.
- Hashimoto's thyroiditis.
- Cholecystectomy.
- Kidney pathologies, hemodialysis.
- Poisoning with heavy metal salts (lead).
- Deficiency or, conversely, excess of iodine.
A TSH higher than normal indicates a dysfunction of the thyroid gland, which cannot cope with the production of sufficient amounts of hormones.
Consequences of high TSH during pregnancy without treatment:
- early miscarriage;
- fetal growth restriction;
- deviations in mental development, up to cretinism;
- neuropsychiatric disorders;
- congenital hypothyroidism.
Symptoms of increased TSH during pregnancy
If the level of the hormone thyrotropin has increased by 2 times or more, then this is especially dangerous in the early stages of pregnancy. To prevent consequences, it is necessary to monitor any changes in the body and condition.
Symptoms of elevated TSH in early pregnancy:
- lethargy, a feeling of constant fatigue and weakness, apathy towards everything, lethargy and weakness;
- deformation of the cervical spine, swelling of the face and body;
- is haunted by a gag reflex and constipation, resulting in a complete lack of appetite;
- irritability;
- body temperature drops;
- rapid weight gain, up to obesity;
- external changes (dry skin, pallor, hair loss, brittle nails);
- sleep disorder - you want to sleep during the day and stay awake at night.
Threatening condition – above 7 units. Most of the symptoms coincide with signs of early pregnancy toxicosis, so if there is any suspicion, additional examination is necessary.
TSH is elevated: what to do
Eutirox is often prescribed
If thyrotropin has increased to 4 units with a normal free T4 level, then no treatment is required. Conservative therapy is carried out when the indicator is exceeded by 2.5 times.
To reduce TSH, the drug L-thyroxine is prescribed, and after the birth of the child it cannot be discontinued. Only the dosage is adjusted.
Auxiliary treatment during pregnancy is carried out with Eutirox. When hormone levels normalize, it is canceled.
Sometimes it is enough to correct high TSH by taking Iodomarin, proper nutrition and lifestyle. For example, an individual diet, good sleep at night, reasonable physical activity and walks in the fresh air.
The tactics and course of therapy, dosage and treatment regimen are developed by an endocrinologist.
When to see a doctor
During pregnancy, a woman is recommended to consult an endocrinologist immediately when the first signs of an increase or decrease in TSH appear.
During pregnancy, you need to carefully monitor your TSH level and contact an endocrinologist at the first signs of deviation from the norm.
In most cases, problems are discovered when the expectant mother comes for a routine examination to an obstetrician-gynecologist and undergoes additional examinations. Timely help from an endocrinologist will prevent complications and deliver the baby healthy. It is not recommended to take medications on your own, since you can harm not only your health, but also the fetus.
Correction of TSH levels during pregnancy
If the development of hyper- or hypothyroidism is suspected, the obstetrician-gynecologist observing the pregnant woman will send her for a consultation with an endocrinologist. The endocrinologist, in turn, will prescribe an examination:
- Ultrasound of the thyroid gland (size, volume, presence of nodes, inflammation or tumor);
- donating blood for TSH, T3, T4;
- detection of antibodies to thyroid peroxidase;
- computed tomography of the brain (if a tumor of the pituitary gland or death of its tissue is suspected).
After establishing the cause of an increase or decrease in TSH, drug treatment is prescribed:
- an increased concentration of TSH and a decrease in thyroid hormones requires replacement therapy with levothyroxine (L-thyroxine, eutirox) and the prescription of iodine-containing drugs;
- a decrease in TSH levels and an increase in the concentration of thyroid hormones requires treatment with thyreostatics (methimazole, thiamizole).
It is also important to change the diet of the expectant mother. For hypothyroidism, include foods rich in iodine in your diet (sea reptiles, fish, seaweed, iodized salt) and limit the intake of simple carbohydrates (sweets, baked goods) and dairy products. In case of thyrotoxicosis, eliminate iodine-containing foods from the diet and increase the consumption of proteins, fats and carbohydrates, fresh vegetables and fruits. Also avoid consuming foods that have a stimulating effect on the brain (strong tea and coffee, seasonings and spices, chocolate).
How to get it back to normal
TSH (the norm during pregnancy is slightly different as a result of the influence of numerous factors) deviations are treated by an endocrinologist. The specialist selects a treatment regimen, taking into account the source of low or high concentrations of thyroid-stimulating hormone. The results of the research and the individual characteristics of the female body and fetal development are also taken into account.
Medications
Taking into account the degree of deviation of TSH from the norm, an obstetrician-gynecologist or endocrinologist prescribes appropriate medications:
| Group of drugs | Name | Application |
| Iodine preparations | "Iodomarin", "Antistrumin" | The recommended dosage for pregnant women is 2 tablets. per day. |
| Thyroid hormones | "Euthirox", "L-Thyroxine" | The initial dosage is 25-50 mcg per day. Maintenance therapy includes 100-200 mcg per day. |
| Antithyroid drugs | "Propitsil", "Tyrozol" | The medicine is taken every 6-8 hours. Considering the condition of a pregnant woman, the standard dosage is 25-100 mg. |
| β-blockers | "Bisoprolol", "Atenolol" | Treatment begins with a minimum dose of 5 mg per day. If necessary, it is increased to 10 mg. |
Properly selected therapy will allow you to control the functions of the pituitary gland and the functioning of the thyroid gland, improve the course of pregnancy and prevent abnormalities in the development of the fetus.
Traditional methods
Alternative medicine will allow you to restore the level of thyroid-stimulating hormone if you choose the right medicine. It is important to use traditional methods in complex therapy, strictly after consultation with an endocrinologist. There is a high probability of an allergic reaction or individual sensitivity.
| Name | Recipe | Application |
| Collection of herbs | Mix celandine, birch leaves, coltsfoot, rosehip, yarrow, angelica root and licorice in equal proportions. The herbal mixture is poured with boiling water and left to infuse for 30 minutes. The finished product is filtered and taken orally. | The medicine is taken 30 minutes before meals each time. The course of therapy in most cases is at least 90 days. |
| Rowan and feijoa | Grind the main products using a meat grinder. Mix 200 g each and add sugar to them. | It is recommended to consume the resulting product 20 g every morning before meals. The course of therapy lasts 1 month. |
| Alcohol solution | Mix equal amounts of eleutherococcus root, gorse herb, dandelion and gooseberry. Pour 1 dl. herbal mixture with hot water (500 ml) and leave for 1 hour. | Before use, you must add 60 drops of the tincture obtained from the nut partitions to the finished product. The medicine is taken 4 times. per day 100 g. |
Folk remedies will not help get rid of the underlying disease that provoked changes in TSH levels. It is important to undergo a medical examination and select comprehensive therapy, using traditional medicines along with prescriptions from healers.
Other methods
Minor deviations in the level of thyroid-stimulating hormone can be restored by following a diet:
| TSH level | Authorized Products | Prohibited Products |
| Elevated |
|
|
| Reduced |
|
|
TSH (the norm during pregnancy is determined by special diagnostic tests) deviations require not only a balanced and rational diet, but also following a correct lifestyle.
Principles of a healthy lifestyle:
- exercise regularly and moderately;
- avoid strong emotional stress;
- give up bad habits (cigarettes, alcohol, drugs);
- do not overdo physical activity;
- devote more time to rest;
- review your nutritional diet;
- do yoga or breathing exercises.
It is also recommended to walk more in the fresh air, run, and bike rides. A favorite activity or hobby (drawing, knitting, painting) will help distract you from a negative mood.
Features of donating blood to check TSH levels: what are the rules?
The normal thyroid-stimulating hormone during pregnancy should be within the acceptable limit, which eliminates the risks and likelihood of premature termination of pregnancy. Deviations are dangerous for the normal course of pregnancy, so some adjustment will be required. If you ignore the doctor's recommendations, this may subsequently affect the baby's health. He may have congenital thyroid dysfunction.
If a woman has not donated blood for hormones before conception, she will be advised to do so at 6–8 weeks of pregnancy. The time frame may shift upward or downward - it all depends on the time of the first visit to the gynecologist after pregnancy and the presence or absence of thyroid dysfunction in the past.
In order for the tests to be effective and true, blood should be donated according to certain rules:
- Go to the laboratory in the morning - it is advisable to set a time for visiting from 7 to 11 o'clock;
- You should not eat food before tests. You can drink some clean water without gas, but you should still avoid coffee and tea;
- You should forget about cigarettes within 24 hours. In general, during pregnancy, smoking harms not only the health of the mother, but also the unborn child. He receives a “full cocktail” of harmful substances directly through the umbilical cord;
- You need to tell your doctor about the medications you are taking. He decides whether the appointment should be delayed or whether a TSH test can be taken during pregnancy without stopping medications. This is especially important for those undergoing replacement therapy.
If there is a deviation in the functioning of the thyroid gland and pituitary gland, periodic testing may be required. How often this should be done is up to the attending physician to decide. It also determines the need for tests for other hormones.
Possible complications
In pregnant women, minor deviations are observed in the first 3 months, when medical treatment is not required. The hormone concentration stabilizes on its own by week 16. There are serious diseases, against which the glandular tissue grows, the level of T3 and T4 increases, which provokes serious complications.
| Thyroid stimulating hormone (TSH) level | Complications |
| Short |
|
| High |
|
Expectant mothers are recommended to be registered with a doctor in order to promptly identify deviations and take action. There is a threat not only to the health of the mother, but also to the child. Hypothyroidism causes problems with memory and intelligence in children. The child does not adapt well to society and is diagnosed with mental and physical retardation.
Normal functioning of the thyroid gland will allow you to bear and give birth to a healthy child.
It is important to constantly monitor your thyroid-stimulating hormone (TSH) levels. Timely diagnosis of abnormalities during pregnancy will allow you to quickly take action and prevent negative consequences for the woman and the fetus.
Consequences for the fetus and the expectant mother
If TSH decreases due to excessive production of iodine-containing hormones, a hyperthyroid state is diagnosed. Untimely correction of hormonal levels leads to an acceleration of metabolism and rapid depletion of the energy reserves of the expectant mother’s body.
With low TSH, pregnancy can have consequences for the mother and fetus:
- early toxicosis with constant vomiting;
- threat of spontaneous miscarriage;
- placental abruption;
- fetoplacental insufficiency;
- gestosis (late toxicosis);
- premature birth;
- myocardial failure;
- anatomical abnormalities of the fetus;
- neonatal thyrotoxicosis;
- thyrotoxic crisis.
In 2.5% of patients with an excess of T3 and T4 in the blood, complications arise due to the transfer of autoantibodies to target cells into the child’s body. As a result, fetal malnutrition occurs, which is manifested by delayed growth and psychomotor development of the child after birth.
Thyrotropin deficiency due to pathologies in the hypothalamic-pituitary system leads to a decrease in iodine-containing hormones in the blood. In this case, low TSH levels during pregnancy will lead to:
- hypertension;
- fetal underdevelopment;
- threat of miscarriage;
- premature birth;
- early toxicosis;
- neonatal fetal death;
- placental insufficiency;
- weak labor activity;
- asphyxia of the fetus when passing through the birth canal.
After childbirth, 1/3 of patients experience postpartum thyroiditis.
Children born to mothers with endocrine disorders often exhibit memory and thinking disorders.
Transient thyrotoxicosis
Transient gestational thyrotoxicosis is the most common cause of decreased TSH in the first trimester. This is a temporary condition associated with physiological changes in the body of a pregnant woman. Gestational thyrotoxicosis persists up to 14-16 weeks, after which hormone levels normalize. Less commonly, this condition remains in the second trimester.
Distinctive features of transient thyrotoxicosis:
- first detected during pregnancy;
- no history of thyroid disease;
- occurs exclusively in the first trimester;
- disappears spontaneously after 8-10 weeks.
The risk of developing gestational thyrotoxicosis is higher in multiple pregnancies.
The symptoms of the transient state are similar to those of true hyperthyroidism. Diagnosing pathology during gestation is quite difficult. Characteristic symptoms - rapid heartbeat, fatigue, sweating, nausea and vomiting - can easily be confused with the usual manifestations of a normal pregnancy. Often hyperthyroidism is disguised as early toxicosis. Therefore, all women with severe vomiting of pregnancy (weight loss of 5% or more, signs of dehydration) need to donate blood to determine TSH.
Diagnostic markers of transient thyrotoxicosis:
- decrease in TSH less than 0.1 mU/l;
- an increase in total T4 by 1.5 times or more from the norm for a certain gestational age;
- increase in free T4;
- Ultrasound shows no changes in the thyroid gland.
Gestational hyperthyroidism goes away on its own by the beginning of the second trimester. Treatment is usually not required. In rare cases, drugs that reduce the activity of the thyroid gland, as well as symptomatic drugs, are prescribed. If laboratory changes persist after 16 weeks, you need to look for another cause for this condition.
Symptoms of thyrotropin level imbalance in a pregnant woman
During pregnancy, it can be very difficult to distinguish symptoms of an imbalance in TSH levels from manifestations of toxicosis and other factors of an “interesting situation”. But identifying this pathology is extremely important at an early stage of pregnancy, so the expectant mother should very carefully monitor the changes occurring in her body. And if you have “alarming symptoms,” immediately consult a doctor.
An endocrinologist should decide whether it is necessary to conduct an examination to determine the TSH level and further analyze the results obtained.
Table: manifestations of elevated thyrotropin levels
| Target | Manifestations |
| Nervous system | Decreased memory, lethargy, drowsiness, irritability, absent-mindedness, polyneuropathy (manifested by a feeling of tingling, pain, trembling of fingers and toes) |
| The cardiovascular system | Low blood pressure (hypotension), slow heart rate (bradycardia) |
| Digestive system | Decreased appetite, frequent attacks of nausea and vomiting, tendency to constipation |
| Reproductive system | Ovarian dysfunction, hormonal imbalance, decreased libido |
| Skin and hair | Slower growth and increased fragility of hair and nails, dry skin, excessive hair loss |
| Exchange processes | Low body temperature, increased chilliness, rapid weight gain |
| Protein metabolism | Puffiness of the face, lips, periorbital edema, swelling of the ENT organs (nasal mucosa, middle ear, vocal folds), leading to worsening nasal breathing, decreased hearing and hoarseness of the voice |
| Hematopoietic system | Various types of anemia, dysfunction of the coagulation system |
Table: manifestations of low thyrotropin levels
| Target | Manifestations |
| The cardiovascular system | Increased heart rate (tachycardia), observed even during sleep, arrhythmias (irregular heart rhythm) |
| Digestive system | Increased appetite, tendency to diarrhea, abdominal pain, nausea and vomiting |
| Nervous system | Tremor, increased sweating, restlessness, anxiety, irritability, memory loss, increased distractibility |
| Exchange processes | Acceleration of basal metabolism (even with normal or increased appetite, weight loss is noted) |
| Thyroid | Increase in size or detection of compactions upon palpation |
| Appearance | Exophthalmos (bulging eyes) |
What to do if there are deviations from the norm?
For any deviations from the norm, an obstetrician-gynecologist and endocrinologist will be able to choose the correct and optimal course of treatment for you. Under no circumstances should you self-medicate, much less prescribe yourself hormonal medications.
Most often, when TSH levels are elevated, a synthetic drug is prescribed: Euterox, Levothyroxine, Bagotyrox and others.
Previously, dried and crushed animal thyroid glands were used for treatment. However, now doctors rarely use such a remedy, since synthetic drugs have a constant level of activity and are much purer. The drug is initially prescribed in minimal doses, gradually increasing. Reception continues until the level of the hormone in the blood returns to normal.
Just as with low hormone levels, the drug, as well as its dosage, is prescribed exclusively by the doctor treating or monitoring you.
In addition, after preliminary consultation with your doctor, you can resort to traditional medicine methods. For example, a medicinal decoction of: birch leaves, angelica, licorice root, yarrow and celandine is considered effective in this matter.
Symptoms of elevated TSH
TSH levels affect the functioning of many body systems. A change in its indicators affects the general well-being of the pregnant woman. Some symptoms of increased thyroid-stimulating hormone are quite difficult to distinguish from the first manifestations of pregnancy in the early stages.
These are:
- weakness;
- feeling of slight malaise;
- high fatigue;
- decreased physical activity;
- slow thinking;
- decreased body temperature;
- apathy;
- absentmindedness;
- loss of appetite.
All these phenomena can be observed in a woman in the early stages due to a general change in hormonal levels. This is why many pregnant women often do not realize that their TSH levels are abnormal before taking tests.
However, there are some distinctive signs indicating increased levels of the hormone. They can be observed with a significant deviation of TSH from the norm. It is in these cases that there are risks for the mother and fetus.
A pregnant woman experiences a slight lump in the neck area. It appears due to an increase in the volume of the thyroid gland. Such changes occur due to the fact that the organ cannot cope with the normal production of the hormones T3 and T4. Also, due to general changes in hormonal levels, a pregnant woman experiences a significant weight gain. In the first trimester, a woman should gain only a few kilograms. If the weight gain is more than 6 kilograms, then this is quite an alarming signal.
If a pregnant woman detects one or more of the described symptoms, in combination with elevated TSH, additional studies are carried out and the necessary treatment is prescribed.
An increase in TSH is quite common in pregnant women. It can be either normal or pathological. Only the attending physician can make a correct diagnosis based on the analysis data and prescribe appropriate treatment.
During pregnancy, a restructuring of a woman's entire hormonal system occurs, including the endocrine system. Therefore, it is important to monitor your thyroid hormone levels. The TSH norm during pregnancy by trimester and symptoms of deviations - this is the subject of the next article.
What are the reasons for the increase in thyroid hormone, we will consider in this material.
Diagnostics
To find out whether TSH is elevated during pregnancy or not, you need to take a blood test for thyrotropin.
To do this you need:
- For two days, avoid taking iodine preparations or medications containing steroid and thyroid hormones.
- Avoid physical and psycho-emotional stress throughout the day.
- 2-3 hours before the test, do not take any liquid other than pure still water.
In cases where TSH is elevated, more in-depth testing should be done during pregnancy to find out the cause of this condition.
For this purpose, the attending doctor prescribes other laboratory and instrumental examination methods, for example:
- Ultrasound of the thyroid gland;
- MRI of the brain;
- a complete profile of hormones responsible for the function of the thyroid gland - total, free T3, T4, antibodies to thyroid peroxidase (TPO), thyroglobulin, and TSH receptors.
Video
I suggest you watch an interesting video in which the doctor describes all the intricacies of the relationship between TSH and gestation, what its normal level is in pregnant women. What does this indicator indicate, what medications can be prescribed for treatment and adjustment.
When planning and during pregnancy, the expectant mother will have to undergo a number of studies and tests, since the birth of a new life in her places a large burden on her body. In addition, using the results of the tests, you can find out not only what state the mother’s body is in, but also how the baby is developing.
Will you now share your experience with us in the comments on the website, have you been tested for TSH levels, were any abnormalities found, what treatment was prescribed to you and how do you and your baby feel now?
How do TSH levels change in pregnant women?
In a healthy person, triiodothyronine, thyroxine and TSH interact according to the principle of an inverse relationship: with an increase in T3 and T4, thyroid-stimulating hormone is suppressed. This pattern is the cause of normal physiological fluctuations in TSH during pregnancy at different stages.
If in an adult non-pregnant woman the normal level of thyroid-stimulating hormone is 0.4–4.0 mU/l, then during pregnancy the norm is in the range from 0.1 to 3 mU/l. In addition, TSH norms during pregnancy are distinguished by trimester.
The 1st trimester is the period when the intensive formation of triiodothyronine and thyroxine is actively influenced by the “pregnancy hormone” - human chorionic gonadotropin (hCG). At this time, the baby’s developing body is not yet able to produce its own T3 and T4. This means that their only source is the maternal endocrine system. Under the influence of hCG, a vigorous increase in T3 and T4 occurs, and under their influence the level of thyroid-stimulating hormone decreases. The TSH norm during early pregnancy is reduced to 0.2–0.4 mU/l. By 12–16 weeks this figure increases.
The 2nd trimester is a time of intensive growth of internal organs in the fetus. By this time, the fetus has already formed the basic elements of various body systems, including the endocrine one. In the second trimester of pregnancy, the baby’s own thyroid gland is already working and the process of producing hormones is gradually improving. At this time, pregnant women's hormonal levels change: the amount of thyroxine and triiodothyronine decreases, and the concentration of thyroid-stimulating hormone increases. Its indicator differs from the TSH index in the first trimester and is 0.3–2.8 mU/l.
In the 3rd trimester, TSH norms in pregnant women approach the general values and amount to 0.4–3.5 mU/l.
In terms of TSH levels, the norm in women during pregnancy varies not only depending on the trimester, but also on the number of fetuses. If the birth of twins or triplets is expected, thyroid-stimulating hormone in pregnant women can decrease to almost zero.
Even if there is only one fetus, a slight decrease or increase in TSH is considered a physiological norm and in most cases does not require correction. In addition, there is some discrepancy in the methods assessing the recommended TSH level during pregnancy.
The table of TSH parameters used in Russia during pregnancy contains the following data on the concentration of thyroid-stimulating hormone in the blood plasma:
- I trimester – 0.2–0.4 mU/l,
- II trimester – 0.3–2.8 mU/l,
- III trimester – 0.4–3.5 mU/l.
In the USA, the TSH hormone and pregnancy correlate somewhat differently week by week and lower levels are considered normal.
A high level of thyroid-stimulating hormone, especially in the first 12–16 weeks, is a sign of trouble and requires a detailed examination. But even if the indicator increases slightly and the pregnancy is proceeding normally, the gynecologist may prescribe an additional consultation with an endocrinologist. The specialist will adequately assess the concentration of the TSH hormone and, if necessary, recommend appropriate treatment.