1
Author of the article: Marina Dmitrievna
2017.10.01
12 354
Blood analysis
A blood test is the main and first test that doctors prescribe when a patient is admitted to the hospital. It provides complete, quick and cheap information about the patient’s condition. However, such tests are different; one option is a study on the number of blast bodies. What are they, why are they needed and what is the normal level in the blood? Let's figure it out!
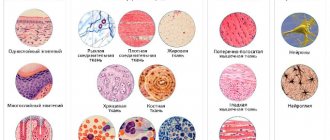
Identification of cells under a microscope
Blast cells: their number and condition in a healthy body
When a person has not been diagnosed with any disease, there is no stress, no infectious diseases or other factors, the following occurs:
- blast cells are completely absent in the bloodstream;
- in the bone marrow they are recorded in no more than 5% of the total number of cells.
Let us repeat: normally, blast cells should be completely absent in a blood test; “0%” should be written on the result form. Even a small number of blasts in the bloodstream is a very serious reason to consult a doctor and conduct additional research.
What do normoblasts in the blood mean?
A complete blood count is regularly used by medical professionals to identify hidden diseases.
Interpretation of the results obtained is carried out thanks to special tables with indicators of the calculated norm for each component of the biomaterial. If there are any pathologies in the patient, the ratio of markers will be disrupted. However, if leukocytes or red blood cells must be detected during diagnosis, then blasts in the blood will often indicate disturbances in the functioning of the immune system.
What are normoblasts?
Blast cells are an intermediate form of erythrocytes (red blood cells), responsible for saturating body tissues with oxygen, as well as removing carbon dioxide from the body.
These substances are formed, like all formed elements of blood, in the bone marrow. Blue-violet cells at this stage of development are actively enriched with hemoglobin, which provokes a decrease in the nucleus.
When it is completely dissolved, normoblasts will acquire smaller sizes and transform into pinkish reticulocytes.
Blast cells in a blood test under a microscope
They, in turn, leave their abode, entering directly into the bloodstream, where over the course of 1–3 days they get rid of unnecessary organelles (mitochondria, endoplasmic reticulum). Reticulocytes can already carry out oxygen transport, but their functionality increases significantly after they are fully transformed into biconcave erythrocytes.
Often, when deciphering indicators, experts mention normocytes or blastocytes. It must be remembered that these terms are the medical interpretation of normoblasts.
If the level of blasts in the blood is sufficiently elevated, the body may be affected by the following diseases:
- osteosarcoma;
- DiGugliermo Pathology;
- acute erythroleukemia;
- myeloblastic anemia;
- bone marrow cancer;
- glioblastoma;
- multiple metastases;
- lymphoblastic leukemia;
- thalassemia;
- hepatoma;
- extramedullary hematopoiesis;
- megaloblastic anemia;
- hypoplastic anemia;
- bronchogenic carcinoma.
Sometimes the reason for the appearance of normoblasts in a blood test is hemolysis, a disease characterized by the pathological destruction of red blood cells with the release of hemoglobin into the blood.
When the human body loses the most important carriers of carbon dioxide and oxygen, hypoxia develops.
In order to avoid irreversible consequences, the bone marrow sends normoblasts to help the immune system, which temporarily replace their more mature “brothers”.
Often, the number of normocytes is diagnosed in women after heavy menstruation or difficult childbirth, which resulted in damage to internal organs. If the patient has previously suffered an infectious disease, the results of his general blood test will most likely also show normocytes.
Serious blood loss caused by severe injury will normally be characterized by the appearance of normoblasts that stabilize hematopoietic function
How is blood drawn?
Typically, the OAC procedure requires capillary blood from the ring finger. After his pad is disinfected with medical alcohol, a painless puncture is made using an automatic scarifier. Periodically squeezing the finger at the nail plate, the laboratory technician draws out about 2-3 ml of biomaterial using a glass capillary.
When the blood samples are distributed into containers, the wound is again disinfected and a sterile cotton pad is applied to it. Much less often, venous blood is taken from the ulnar vessel for laboratory testing. In this case, a tourniquet is first applied to the shoulder and the puncture site is treated, after which the needle of a vacuum system or a disposable syringe is inserted into the vein.
The angle of the needle is gradually reduced, making it easier to collect material. As soon as the procedure is completed, a gauze swab is pressed to the puncture area, the needle is removed from the vessel and the tourniquet is removed. You need to hold the cotton wool until the wound becomes clogged with a blood clot, otherwise a painful subcutaneous hematoma will form in the fold area.
Preparing for diagnosis
Blood test for RFMK + interpretation
Having received the results of a general analysis, the attending physician will never evaluate only one of its parameters, without paying attention to the others.
To ensure that the balance of the quantitative content of all blood cells in addition to normoblasts is not artificially disrupted, you should adhere to certain preparation rules for several days before diagnosis.
A week before the procedure, you need to inform the specialist about the list of medications you are taking so that he can assess the degree of their effect on the composition of the blood. If certain medications cause undesirable changes, their use may be temporarily suspended. In 3–4 days, harmful foods and drinks are removed from the diet, especially fast food, alcohol, marinades, fatty and fried foods.
It is also necessary to stop sports activities for 1-2 days; running and swimming are no exception. You should visit a medical facility on an empty stomach. Smoking is prohibited before diagnosis. If the patient hastily came to the clinic, he definitely needs to catch his breath before entering the office.
It is not recommended to abuse confectionery products on the eve of blood sampling - exceeding the daily dosage of sweets entails a false test result
Is an elevated level always a sign of pathology?
Not at all. For example, normoblasts in a general blood test in absolutely healthy infants up to 3–4 months are a completely acceptable phenomenon associated with the active physiological formation of a small organism.
In older children, blastocytes should be observed only in the bone marrow and not in the blood.
If biomaterial is collected from a patient with pernicious (malignant) anemia, then the detection of normocytes is considered a harbinger of imminent remission.
Under such circumstances, blast cells will indicate the presence of functional defense mechanisms. Moreover, people sometimes get disappointing results that are overshadowed by repeat diagnostic rates. Therefore, you should not worry when you see alarming numbers on the form; you need to calmly visit a specialist to confirm or refute them.
Source: https://apkhleb.ru/krov/chto-znachat-normoblasty-krovi
Shifts in the formula as health status changes
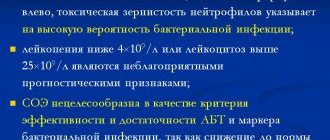
If the bone marrow contains 1% blasts, this is a standard indicating that everything is fine with the body. A result of 5% to 10% is not normal, but it is not yet an indicator of a specific hematological disease.
Blasts in the bone marrow in such quantities can be either as a result of severe stress or as a consequence of an acute infectious process.
If blast cells in the bone marrow are found in an amount of more than 10%, this is a reason for the doctor to diagnose leukemia.
However, such a diagnosis is made based on a combination of factors:
- low red blood cells, platelets and hemoglobin;
- high white blood cells;
- the presence of blast cells in the bloodstream;
- the presence of blasts in the bone marrow in an amount of more than 10%.
It is important to note that the test to determine the number of immature blood cells is not done independently; As a rule, it is referred to it by a doctor - a therapist or hematologist - if there are compelling reasons. For example, if a patient during an examination presents complaints that could lead to a diagnosis of leukemia, the doctor may refer such a patient for analysis, where they will determine whether his level of blast cells in the blood is exceeded.
Blast cells in a blood test - what kind of cells are they, their norm in the blood and what deviations indicate
A blood test is the main and first test that doctors prescribe when a patient is admitted to the hospital. It provides complete, quick and cheap information about the patient’s condition. However, such tests are different; one option is a study on the number of blast bodies. What are they, why are they needed and what is the normal level in the blood? Let's figure it out!
What are blast cells?
Blood is the most important fluid in the human body. Performs many functions: from nutrition to protecting organs from infections and bacteria. Blood cells are responsible for each “task”, for example: erythrocytes - red blood cells, deliver oxygen to the corners of the human body.
The precursors of blood elements are blasts. They develop in the spinal cord and, as needed, turn into red blood cells, white blood cells, and so on. Healthy cells are ready to “transform” during acute crises in large quantities, appearing in the blood in the form of protective or other cells.
What is acute leukemia?
Acute leukemia is a consequence of a disruption in hematopoiesis in the initial stages. In a normal state, blast cells turn into functional blood cells and fulfill their mission. Each such little body immediately after “birth” has its own line of development. For example: for erythrocytes one type of such cells is “produced”, and for leukocytes another, and so on.
https://www.youtube.com/watch?v=9L2fgTdUUSg
When the hematopoietic system fails and the creation of healthy base cells is disrupted, the corpuscles behave differently.
They do not turn into “working” cells - they only consume useful substances and multiply. Over time, they replace healthy cells and penetrate the bones, destroying them without supplying useful substances.
The number of useful cells sharply decreases, hemoglobin, platelets and leukocytes drop.
This disease is lymphoblastic and myeloblastic - depending on what type of cells became the “culprit” of the disease. They are divided into other, smaller categories, depending on the purpose of the damaged blast elements.
They can be designated, for example: acute B-lymphoblastic leukemia, which implies a failure in the creation of blasts at the level of “production” of elements such as B-lymphocytes, or acute monoblastic leukemia, which arose due to problems in the creation of monocytes. Depending on the degree of complexity and type of leukemia, the prognosis for a patient’s cure varies.
Preparation for analysis for the presence of blasts in the blood
To ensure that the analysis result is not distorted and does not have to be retaken, it is recommended to follow a few simple rules:
- the last meal should be 8 hours before the test;
- the day before the study you should not drink any alcoholic beverages;
- 2 hours before the test, eliminate the effects of nicotine on the body;
- It is recommended to stop taking medications 72 hours before the test.
If it is not possible to complete any of the points, you must definitely tell the laboratory assistant who will take your blood.
Tell him about all medications you are taking 3 days before the medication test. If for health reasons you cannot go without food for a long time, be sure to tell the laboratory assistant exactly what you ate. This information will help you correctly adjust the analysis results. They will still most likely be distorted, but the doctor in the conclusion will be able to correctly reflect the information, taking into account the information you provided.
How to recognize leukemia by blood test?
Hematologist, Doctor of Medical Sciences Sergei Semochkin about acute lymphoblastic leukemia
Hematologist, Professor of the Department of Oncology, Hematology and Radiation Therapy, Russian National Research Medical University named after. N.I. Pirogova of the Ministry of Health of Russia, Doctor of Medical Sciences Sergei Semochkin said: is it possible to recognize acute lymphoblastic leukemia (ALL) at an early stage and make a diagnosis using a blood test; explained how ALL is treated and who is eligible for bone marrow transplantation (BMT).
What are the early symptoms of acute lymphoblastic leukemia? Can they be seen and recognized by ALL?
In this case, everything is quite simple, because the word “acute” means that the disease is sudden and often the symptoms are very expressive. The most common symptom is fever, i.e. increase in body temperature.
Fever can be either low-grade or severe, up to 39 degrees. Changes associated with bone marrow damage will appear. A decrease in hemoglobin will lead to weakness and fatigue.
The lymph nodes may become enlarged and discomfort may appear in the abdominal cavity due to the increase in the size of the liver and spleen. There may be signs of bleeding - even while brushing your teeth.
In some patients, ALL may begin with neurological manifestations - headaches, dizziness and other problems. The symptoms are extensive, but in this case they are quite acute and suddenly arisen.
Watch the video on our website.
Can a diagnosis be made using a blood test? What will it show?
As a rule, a blood test contains clearly defined indicators: hematopoiesis is altered, the number of leukocytes is outside the normal range - it may fall below normal values, or it may become prohibitively large. I have met patients in whom the number of leukocytes, which was normal from 4 to 9 thousand, increased to 200 thousand per μl.
Platelets are also in some cases very much reduced, but the main thing is the change in the number of leukocytes. A very important marker is the release of tumor cells into the blood, when immature early cells, called blast cells, appear in the blood.
If a blood test reveals blast cells, it is most likely either acute leukemia or myelodysplastic syndrome.
How does a patient get to a hematologist?
A blood test with characteristic changes is a reason to immediately call an ambulance and hospitalize the patient in a specialized hospital. When treating children and adolescents, an oncohematologist usually has one or two days to diagnose; treatment must begin as early as possible.
The diagnosis includes a repeat blood test, then verification of the diagnosis, for which a bone marrow biopsy is performed. In young children it is performed under general anesthesia, in adults - under local anesthesia. Using a small needle, I puncture the sternum or ilium. In children, sternum puncture is not performed.
The resulting bone marrow sample, which looks like a regular tube of blood, will be sent to a laboratory where a range of tests will be performed to confirm the diagnosis. The main criterion is an increase in the number of blast cells. It is impossible to determine the type of leukemia only by appearance and by the number of blast cells.
Back in 1913, it was established that there is a lymphoid and a myeloid variant of leukemia. For verification, special laboratory methods are used: immunological and chemical. There is a special device - a flow cytometer, which is used to determine markers characterizing a given cell type.
To determine the subtype of acute leukemia, a whole range of genetic studies are used to develop more targeted therapy for these patients.
What are the causes of ALL? There is an opinion that this type of leukemia is very closely related to environmental problems, is inherited and often occurs in those who have already suffered from some kind of cancer. Is this true or not?
The true cause of leukemia in adults can be identified only in 5% of cases, in 95% it is completely unclear what led to what. For children, everything is a little more interesting.
How does leukemia occur? A certain primary mutation occurs in the genetic material of the cell, which in itself does not always lead to leukemia.
Subsequently, this mutation is joined by others, and when the disease does occur, many molecular events have already accumulated in the cell, the combination of which led to the onset of the disease.
The peak of acute lymphoblastic leukemia occurs in children aged two to four years, then the incidence decreases. The next peak occurs at 18-29 years old, then decline again. After 60 years – small growth again.
In some young children, a certain congenital component of this problem can be traced. There are cases of ALL in the fetus or newborn, when the child is born with the disease or becomes ill during the first year of life. Studies of cord blood have shown that newborns have leukemic defects, congenital mutations that can lead to leukemia.
And this mutation is caused by a hereditary factor that worked during intrauterine development. According to various sources, the total number of such babies ranges from 1 to 5%. Then a lot depends on the infectious situation around the child. Numerous infections suffered in childhood contribute to the formation of a normal immune system, which neutralizes the hereditary factor.
If we talk about environmental problems, then no clear connection has been identified with them.
Does UV radiation, microwave, sun rays, radiation affect?
In Hiroshima and Nagasaki, the increased incidence persisted for about 12 years. After Chernobyl, many people suffered damage to their thyroid gland, but the incidence of leukemia did not increase. It all depends on the type of isotopes released into the environment. This did not happen in Fukushima either, because the concentration of radioactive substances was greatly diluted by seawater.
The harm of ultraviolet radiation has been scientifically proven only in relation to melanoma. There is no clear connection with ALL. We do not allow our former patients to visit the solarium and do not recommend sunbathing, because although the connection has not been proven, this factor cannot be completely ruled out.
When it comes to microwave radiation, home microwave ovens are absolutely safe.
How is ALL treated? What awaits the patient?
The concept of treating ALL, which still underlies treatment protocols for ALL, was developed by American pediatrician Donald Pinkel back in 1962. It includes four stages: induction of remission, consolidation, effects on the central nervous system and a long stage of maintenance therapy for two to three years.
All over the world, treatment is carried out according to clinical protocols developed as a result of cooperative studies. According to some studies, strict adherence to protocols increases patient survival by 15-20% compared to individualized treatment. The protocol specifies all actions: from the first day to the last.
It contains instructions on how and at what point to assess complications that arise and what to do about them. There are two centers in Russia that actively conduct such protocols. Center named after Dmitry Rogachev, where Alexander Isaakovich Karachunsky has been conducting a series of protocols “Moscow - Berlin” for many years, since the early 1990s.
Every five years, the design of the protocols is reviewed to improve the treatment of certain categories of patients. for many years since the beginning of the 90s, a series of Moscow-Berlin protocols. Every five years, the design of protocols is changed to improve the treatment of certain categories of patients.
In adult practice, this is the National Medical Research Center for Hematology, where they conduct cooperative research on acute lymphoblastic leukemia in adults.
In what cases is bone marrow transplantation (BMT) indicated?
Unlike acute myeloid leukemia, there are fewer indications for allogeneic (donor) BMT. It is prescribed to patients who have not achieved remission within the time period specified by the protocol or have an unfavorable cytogenetic variant of the disease. In pediatric practice, more than 90% of children recover, and approximately 15-20% are candidates for allogeneic BMT.
In adults, the percentage of patients requiring transplantation is slightly higher, due to the fact that there are many more high-risk genetic operations and the response to standard treatment is worse. When we discussed chronic myeloid leukemia, the Philadelphia chromosome translocation (9;22) appeared there. In ALL, this is an absolutely negative prognosis factor.
In children, this mutation occurs in less than 5% of cases; in people over 50-60 years of age, approximately half of B-lineage ALL will have the Philadelphia chromosome. Unlike chronic myeloid leukemia, the use of tyrosine kinase inhibitors in acute lymphoblastic leukemia is not as successful. That is why in adult practice TCM should be performed on approximately 30% of patients.
The age threshold for allogeneic BMT is around 55 years old, which is reasonable.
How often do relapses occur with ALL?
If we are talking about adults, then relapses occur in almost 40% of cases. There are early relapses that happen right during therapy.
In this case, it is necessary to change the treatment, make it more intense and severe. In such cases, TCM is usually indicated. Late relapse can occur after 20 years.
Unfortunately, we cannot remove the cause that causes this disease - it can return.
Is it possible to plan a pregnancy after ALL?
Long-term chemotherapy impairs fertility, so it is better to cryopreserve the sperm/egg, or even better, the embryo - this is a more reliable method. In men, as a rule, spermatogenesis is seriously impaired, but in women the situation is somewhat better. The likelihood of getting pregnant and bearing a healthy child is high. If at least five years have passed in remission, there are no restrictions.
Can pregnancy be a trigger for relapse?
Probably not. This is not as common as with some other diseases, where pregnancy can actually become a provoking factor.
Is ALL inherited?
Lymphoblastic leukemia is a rare disease, so the likelihood that it will occur in a child born to parents with ALL is extremely low.
How will ALL be treated in the future?
It seems that the basis of cancer treatment in the future will be the activation of one’s own immunity. We need to tune the immune system so that it recognizes and eliminates cancer cells.
We are currently at an early stage in the development of CAR-T therapy, but over time the technologies will improve so much that it will most likely become one of the main methods of therapy for a wide range of hematological oncological diseases.
The essence of the method is that the patient’s own T-lymphocytes are collected and sent to a special laboratory. This laboratory may be in another city, country - it doesn’t matter. In the laboratory, these T-lymphocytes are reprogrammed: they contain information about the tumor cells present in the patient’s body.
After reprogramming, the T-lymphocytes are injected back into the patient, they find cancer cells and remission occurs. The main challenges are to create a high-quality recognition process and develop standard treatment protocols.
Many questions arise in understanding the biology of the disease, because each specific case is very individual. We are only familiar with severe breakdowns, but each individual breakdown provokes a different course of the disease.
We can now completely sequence the genome of a tumor cell and the main thing is to learn to understand what is key in pathogenesis and how it can be influenced, then we will come closer to a complete cure of the disease.
This is the future.
Source: https://leikozu.net/press/stati/kak-postavit-diagnoz-po-analzu-krovi-i-vylechit-oll.html
Bone marrow puncture
Such a study is carried out under local anesthesia and is prescribed only if the absolute content of blast cells in the blood has been exceeded according to the analysis, and so much so that the factor of stress and infectious diseases can be immediately excluded. Then the doctor has reason to suspect a certain type of leukemia. To confirm or refute this diagnosis, a bone marrow puncture is prescribed.
The punctate is examined under a microscope, the number of blast cells is determined. Let us remember: normally it is very small even in the bone marrow - about 1%.
The doctor’s diagnosis will most likely be confirmed if, according to the results of a puncture study, more than 10% blasts are detected in the bone marrow.
Types of leukemia
In medicine, there are many different forms of this disease. In this article we will look at only some of the most common ones. For example, there is acute leukemia, characterized by a large composition of young blast cells. Therefore, we can say with certainty that up to 55% of all cases develop the myeloblastic form of acute leukemia.
Acute lymphoblastic leukemia is also known, which most often occurs mainly in children. In addition, there is also some division into subtypes. Thus, monoclonal antibodies are used for immunological phenotyping of blast cells. Such features are more important for proper research and for identifying an accurate diagnosis. Therefore, the forms of leukemia are fully taken into account in detail.
As for the symptoms, they do not always coincide with the course of the disease, so it is quite difficult to identify all the features of the disease at an early stage.
Interesting information about blast cells (Video)
Related Articles
Bone marrow diseases: symptoms, diagnostic methods and treatment
Mantle cell lymphoma: causes, symptoms and treatment methods
Myelogram: what is it and what diseases does it help identify?
What is lymphoma: symptoms, treatment methods and prognosis
Lymphocytes: normal in men, causes and signs of deviation
Bone marrow: structure, purpose and functioning features
Reason for deviation: leukemia
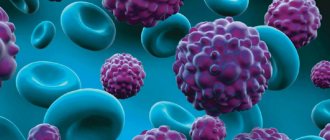
The main reason for the appearance of blast cells in the sample is leukemia. This disease is otherwise called leukemia or blood cancer. The pathology is accompanied by uncontrolled division of immature cells in the bone marrow, which subsequently form a tumor.
Doctors distinguish two forms of leukemia:
- spicy;
- chronic.
In acute leukemia, a huge number of blast cells are found in the blood. Their concentration can be more than 20%. In the chronic form of blood cancer, the rate of immature elements usually does not exceed 5-10%.
Other blood indicators
When studying the results of the analysis, the doctor must pay attention to other indicators of the clinical study. The presence of blast cells in the biomaterial is always considered in combination with other blood parameters. The presence of leukemia may be indicated by the following data:
- Leukocytosis. In approximately 15% of patients with acute leukemia, the white blood cell count is tens of times higher than normal.
- Low hemoglobin. Patients with blood cancer have severe anemia and a decreased number of red blood cells.
- Drop in platelet levels. For this reason, patients with leukemia experience increased bleeding.
- Decrease in reticulocytes. These cells are young forms of red blood cells. Their small quantity leads to anemia.
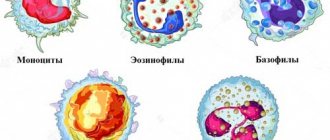
- Complete absence of eosinophils and basophils. This causes a sharp decrease in immunity.
The above signs, together with the appearance of blast cells in the blood, allow the doctor to diagnose leukemia.
What it is
It will take some time for them to transform into mature blood cells. First of all, the formation of a basophilic erythroblast occurs, which has a nucleus in the center. It has a round shape and a size of about 18 microns.
Such cells have a bright blue color. Soon, a polychromatophilic erythroblast is formed from it, which decreases in size in comparison with the basophilic one. Such cells have a wheel-like appearance of chromatin, and the cytoplasm becomes pink-blue in color.
Next, it is converted into an oxyphilic erythroblast. The nucleus of such a cell, which was previously purple, loses its clear structure. The cell becomes even smaller in size and becomes close in appearance to such a blood component as red blood cells.
After some time, the nucleus becomes pyknotic and the cytoplasm changes its color to light blue. This indicates the transformation of erythroblast into polychromatophilic. Next, transformation occurs into reticulocytes, after which mature red blood cells are formed in the blood, which lack a nucleus.
Preparing for diagnosis
Having received the results of a general analysis, the attending physician will never evaluate only one of its parameters, without paying attention to the others.
To ensure that the balance of the quantitative content of all blood cells in addition to normoblasts is not artificially disrupted, you should adhere to certain preparation rules for several days before diagnosis.
A week before the procedure, you need to inform the specialist about the list of medications you are taking so that he can assess the degree of their effect on the composition of the blood. If certain medications cause undesirable changes, their use may be temporarily suspended. In 3–4 days, harmful foods and drinks are removed from the diet, especially fast food, alcohol, marinades, fatty and fried foods.
It is also necessary to stop sports activities for 1-2 days; running and swimming are no exception. You should visit a medical facility on an empty stomach. Smoking is prohibited before diagnosis. If the patient hastily came to the clinic, he definitely needs to catch his breath before entering the office.
It is not recommended to abuse confectionery products on the eve of blood sampling - exceeding the daily dosage of sweets entails a false test result